Urgent message: The treatment of acute otitis media is a common problem throughout healthcare. Many national provider organizations have emphasized the significance of proper diagnosis and treatment is essential for a full, uncomplicated recovery.
Jessica M. Crandall, DNP, ARNP-FNP-BC and Misty Schwartz, PhD, RN
Citation: Crandall JM, Schwartz M. Improving adherence to clinical practice guidelines for the treatment of acute otitis media in pediatric patients. J Urgent Care Med. 2023;17(11):25-34.
Click Here to download the article PDF
Keywords: acute otitis media, pediatrics, antibiotic stewardship, quality improvement
ABSTRACT
Background: The management of acute otitis media (AOM) in pediatric patients has been a growing issue in many healthcare settings. AOM is the second most common pediatric diagnosis seen in outpatient clinics. It is noted that approximately 80% of children will have a diagnosis of AOM at least once in their lifetime. AOM contributes to increased healthcare cost in the United States. The American Academy of Pediatrics (AAP), American Academy of Family Physicians (AAFP), and the American Academy of Otolaryngology (AAO) all note that the management of AOM is a significant problem throughout the United States. The AAP notes that children 2 years of age and older should refrain from antibiotic use for 48 to 72 hours pending assessment and symptoms. The main clinical problem addressed throughout this project is clinic providers not following clinical practice guidelines as they were unaware of them which is leading to inappropriate management of AOM.
Objectives: The main objectives of this quality improvement (QI) project were to provide clinicians with an up-to-date evidenced-based algorithm and education on diagnosis, treatment, and management for AOM for children between the age of 2 and 18 years.
Methods: All providers were educated via an emailed PowerPoint with the current algorithm and modifications, significance of clinical problem, watch and wait component, and current recommendations. Parents/caregivers were educated with flyers in the exam rooms along with handouts at discharge. EPIC electronic medical records (EMR) were used to collect data pre- and postintervention data. The percentage of providers utilizing the current clinical practice algorithm was calculated pre- and postintervention.
Results: There was a 35-point increase in adherence to the clinical practice guideline algorithm. There was an 18% decrease in antibiotic prescriptions overall with a 12% increase in the appropriate first-line antibiotic therapy with amoxicillin. Providers noted that the education and algorithms helped them better manage patients with ear complaints.
Conclusion: The importance of proper management of AOM by following clinical practice guidelines is noted throughout this project. Education played a key role in the success of this project and sustainability will be achieved through continuous education at these locations and eventually to other clinics throughout the network.
BACKGROUND
Acute otitis media (AOM) is defined as an infection of the middle ear. AOM is the second most common pediatric diagnosis seen in family practice, urgent care, and emergency departments.1 This infection is most seen between the ages of 6 to 24 months but can occur at any age. Approximately 23% of children 1 year of age and under will experience at least one episode of AOM and 60% of children will experience one or more episodes of AOM by the age of 3 years.2
Approximately 80% of children will have a diagnosis of AOM at least once in their lifetime.1 AOM can lead to conductive hearing loss, speech and language delays, and side effects from increased antibiotic use.3 Improper diagnosis and treatment can lead to complications such as tympanic membrane perforation, hearing loss, mastoiditis, and antibiotic resistance.3
Common complaints leading to AOM are unilateral or bilateral ear pain/tugging, fever, and fussiness.5 Most guidelines support earlier treatment with antibiotics for a bilateral AOM diagnosis verse a unilateral AOM diagnosis. 2 The prognosis for patients diagnosed with AOM is excellent; however, proper diagnosis and treatment are essential in the prevention of complications such as tympanic membrane perforation, labyrinthitis, mastoiditis, meningitis, brain abscess, petrositis, hearing loss, and lateral and cavernous sinus thrombosis.1
The American Academy of Pediatrics (AAP), American Academy of Family Physicians (AAFP), and the American Academy of Otolaryngology (AAO) all affirm that the management of AOM is a significant problem throughout the United States.2 It is recommended that children 2 years of age and older refrain from antibiotic use for 48 to 72 hours pending assessment and symptoms. Approximately 60% of symptoms related to AOM will completely resolve without the use of antibiotics within about 24 hours, while approximately 80% will resolve on their own without treatment within three days.4
Clinical guidelines are created to help combat AOM complications consistently while achieving the best patient outcomes and decreasing the economic burden on healthcare costs.2 A summary of the best practice guidelines includes proper diagnosis of AOM based on the presentation of moderate to severe bulging of the tympanic membrane (TM), new onset of otorrhea without the presence of acute otitis externa, ear holding, tugging, rubbing in nonverbal children, and extreme erythema of the TM.2
Initial treatment with analgesics along with antibiotics should be reserved for patients with bilateral or unilateral severe AOM, in children 6 months of age and older. Children 24 months and older without severe signs or symptoms such as mild otalgia for less than 48 hours and temperature less than 102.2°F should be initially offered observation with close follow-up rather than antibiotics.2
Amoxicillin should be the first line as long as the child does not have an allergy. If the child has had amoxicillin in the past 30 days, an antibiotic with Beta-lactamase coverage should be utilized.3 Patients should be reassessed if the caregiver reports a lack of improvement or worsening of symptoms within 48 to 72 hours of implementation of the antibiotics. Prophylactic antibiotics should not be prescribed to patients with frequent episodes of AOM.3
The AAFP states that approximately 87% of patients seeking care for AOM get an antibiotic. Clinical guidelines have helped decrease unnecessary prescriptions by up to 12% and increase the accuracy of antibiotic choice by up to 58%. 4 Clinical practice guidelines were created by the AAP and AAFP to provide clinicians with evidence-based recommendations for the management of AOM.5 Treatment to reduce pain such as acetaminophen and ibuprofen should be discussed with parents regardless of AOM diagnosis.
High-dose amoxicillin (Amoxil) should be initiated upon diagnosis of AOM. The “watch-and-wait” method should also be utilized with patients greater than 2 years of age who present with mild symptoms and reliable follow-up. It was noted that 66% of patients who completed the watch-and-wait method recovered without the use of antibiotics.1
The treatment of acute otitis media is a common problem throughout healthcare settings in the United States. It leads to increased healthcare costs, more frequent antibiotic use, and increased morbidity. The AAO, AAFP, and AAP all state that AOM is one of the most common, recurring medical problems in childhood which leads to the most frequent office visits when compared to other complaints such as cough and sore throat. 2 The purpose of this quality improvement (QI) project was to provide clinicians at a rural Iowa urgent care (UC)/emergency department (ED) with a revised up-to-date, evidence-based clinical practice algorithm and education on the diagnosis, treatment, and management for AOM for pediatric patients between the ages of 2 and 18 years.
DESIGN AND METHODS
The three overarching goals of this QI project were to implement an algorithm for the management of AOM based on clinical practice guidelines, to include a watch-and-wait component, and increase adherence to those guidelines through educational interventions. Kurt Lewin’s change theory along with the PDSA method was utilized throughout this project to ensure the sustainability of implemented interventions. The initial focus of this project standardized the use of the clinical practice guideline algorithm for the management of AOM in patients 2 to 18 years of age. The interventions included developing the updated algorithm with watch-and-wait component, educating the providers on the proposed algorithm, exam room flyers, and patient/caregiver handouts. Pre- and post-chart audits were completed for data collection. All nine providers in the UC and ED participated. The proposed outcome of this project was to increase adherence of providers that correctly utilize the proposed clinical practice algorithm for the management of AOM by 50%.
Setting and Population
The setting was a rural UC with an attached ED in a Midwest community. The UC is open 7 days a week, 361 days a year. The hours of operation for the clinic are 7:30 am–7:30 pm Monday through Friday and 8 am–2 pm on Saturday and Sunday. The ED is open 24 hours a day, 7 days a week, 365 days a year. The UC and ED are staffed with both physicians and nurse practitioners (NP).
There was a total of six full-time providers and three per diem providers that included both NPs and physicians that rotate throughout the two departments. Providers work varied shifts between 12 to 72 hours continuously and on site, depending on the department. Other key stakeholders for this project included the DNP supervisors, the UC and ED medical director, the members of the antibiotic stewardship program, and the project leader.
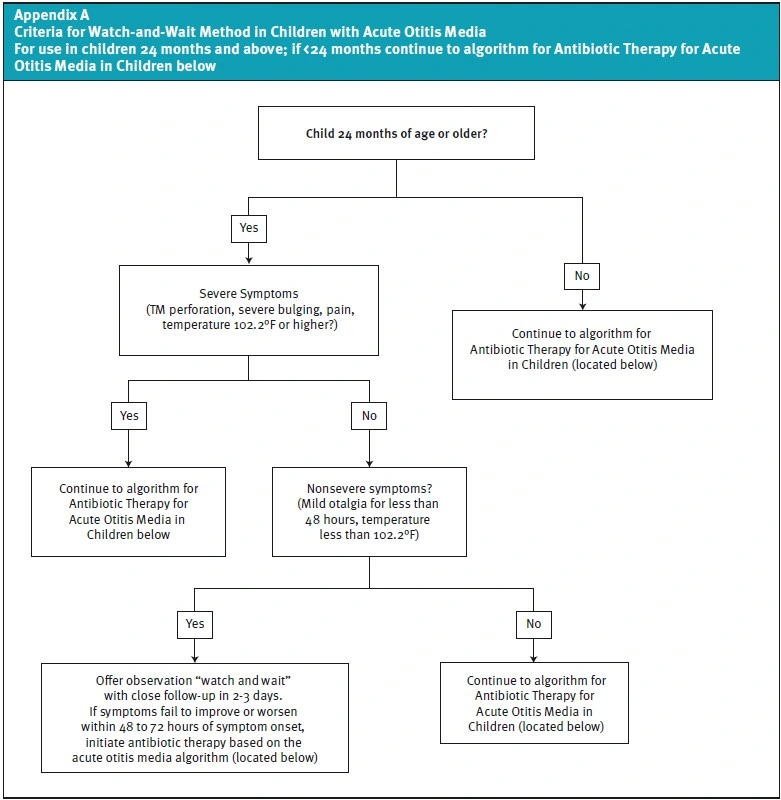
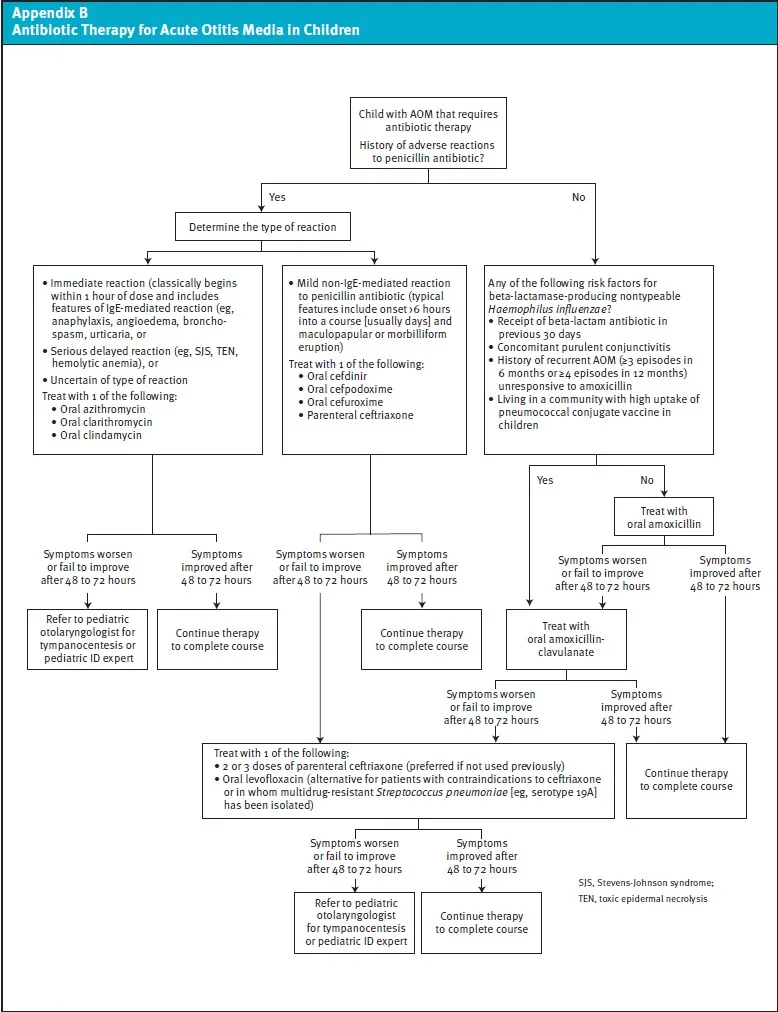
The algorithm developed and utilized was based on clinical practice guidelines from the AAP and UpToDate (see Appendix A and B). The education was provided in the form of a PowerPoint presentation to providers. Educational posters were posted in each exam room. Patient education handouts developed by the Centers for Disease Control and Prevention were provided at the discharge of each visit. The posters and handouts explain management of AOM in plain language.6
Educational Interventions
The developed algorithm, based on current clinical practice guidelines, was the focus of the PowerPoint education. An email of the PowerPoint presentation was distributed to all the providers in the UC/ED explaining the purpose of the project and contained the updated clinical practice guideline algorithm along with a description of the recommended management of AOM. Flyers for exam rooms and discharge handouts were also provided within the educational presentation and were all based on AAP along with CDC recommendations. The algorithm is in an easy-to-follow flow sheet form. It begins by ensuring the child is greater or equal to 24 months of age. From there, the severity of the symptoms is outlined; if symptoms are deemed non-severe (ie, no TM perforation, fever greater than 102°F, severe pain or bulging of TM), the algorithm guides the provider to offer watch-and-wait with close follow-up. If there are severe symptoms, the algorithm guides the provider to the treatment management algorithm that was present at the UC/ED.
Data Collection
This project utilized pre- and postimplementation chart audits. Data collection was implemented with the use of the EPIC electronic medical record (EMR) query system. Patient data were coded and entered in an Excel spreadsheet. The charts were coded based on the number reviewed and did not include any patient identifying information. Within the spreadsheet the code using “Y” for yes and “N” for no signified if the algorithm was utilized with each patient chart to assess the percentage of patients with a diagnosis of AOM who were treated per current clinical guidelines. The pre-intervention chart audit from August through October 2021 resulted in 177 charts, with 60 meeting the inclusion criteria. Data gathered included age; documentation of diagnosis of bilateral or unilateral AOM H66.001, .002, .003, H65.111, 112, 113, H60.502; length of time with symptoms; type of symptoms such as fever, otalgia, pulling/rubbing ears, presence of fluid behind TM; plan for patient such as antibiotic prescribed, analgesic prescribed, antibiotic and for how long; and clinical judgment noted in the chart such as medication allergies or recent treatment. Exclusion criteria included patients with pressure equalizer (PE) tubes, patients under the age of 24 months and over the age of 18, and patients who had additional diagnosis during the visit such as acute sinusitis, streptococcal pharyngitis, urinary tract infection, soft tissue or skin infection, and acute conjunctivitis. The additional 117 pre-intervention charts were eliminated due to exclusion criteria such as age or additional diagnosis such as otitis externa, respiratory infections, or sinusitis.
Following initial pre-intervention chart audit, the PowerPoint presentation, exam room signs, and patient/caregiver education were implemented. Follow-up emails and/or personal interviews were sent to providers for feedback and question responses as needed. The chart audit postimplementation occurred over 8 weeks following the educational interventions from the months of August through October 2022. This audit included 153 charts, with 91 charts being included. Queries using the EPIC EMR were done similarly as in the pre-intervention audit. The same inclusion/exclusion criteria were applied to the postimplementation audit.
PROTECTION OF HUMAN SUBJECTS
This project posed no risk to human subjects and was reviewed and deemed QI by the Institutional Review Board at Creighton University. The project was approved by the Healthcare Management and Information System at the UC/ED. The provider and patient names were kept anonymous during the data collection and all data was stored on a secure server until it was transferred to the excel spreadsheet where all the patient and provider information was de-identified.
RESULTS
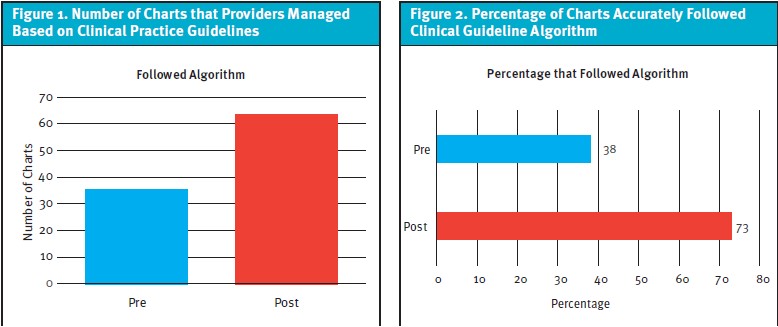
Data revealed an absolute 35-point increase from pre to post intervention. Pre-intervention data revealed that only 38% (n=23) of the time patients were managed based on clinical practice guidelines, while 62% (n=37) of the time they were not. Postintervention data showed that 73% (n=66) of the time patients were managed based on clinical practice guidelines, while only 27% (n=25) of the time they were not (Figures 1 and 2).
The pre-intervention data showed 83% of patients being diagnosed with AOM were unilateral, while 17% were bilateral. Of those with pre-intervention unilateral diagnosis, 100% of the patients received antibiotics, while 90% of patients diagnosed with bilateral AOM received antibiotics. The postintervention data revealed a total of 60% unilateral AOM diagnoses;40% were bilateral. Of those unilateral diagnoses, 89% were given antibiotics, indicating a decrease of 11% in antibiotic prescriptions. Of those bilateral, 65% were given antibiotics also showing a 25% decrease in prescriptions (Figure 3).
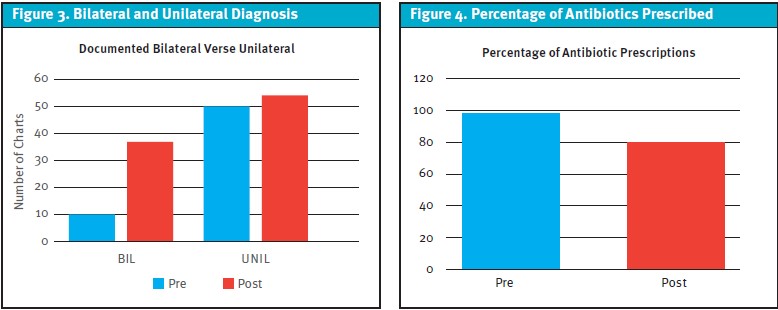
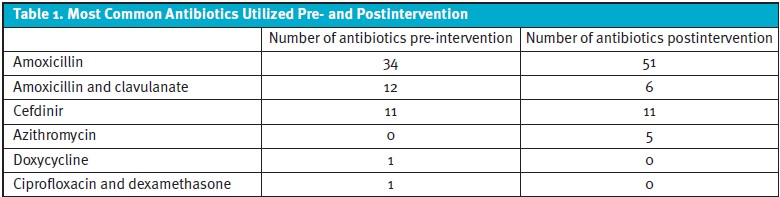
Antibiotics were prescribed 98% of the time in the pre-intervention data. This decreased to 80% in the postintervention data (Figure 4). The most common antibiotics utilized pre-intervention data were amoxicillin at 57%, amoxicillin and clavulanate (Augmentin) at 20%, cefdinir (Omnicef) at 19%, doxycycline at 2%, and ciprofloxacin and dexamethasone at 2%. The most common antibiotics postintervention data were amoxicillin at 69%, amoxicillin and clavulanate at 8%, cefdinir at 14%, and azithromycin at 6% (Table 1).
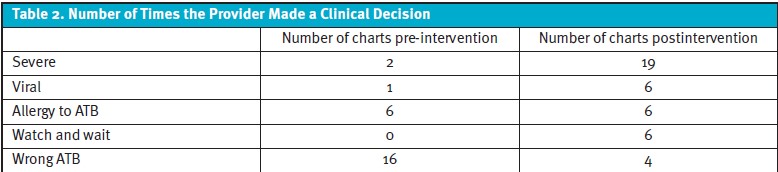
When it came to clinical judgment, pre-intervention data showed 3% of patient symptoms documented as severe, 2% documented as viral, 10% had allergies to first-line medications, and 27% utilized the wrong antibiotic based on the clinical practice algorithm; 0% utilized watch-and-wait. Postintervention data revealed 20% were documented as severe, 6% viral, 6% had allergies to first-line medications, 15% of charts utilized watch-and-wait, and only 4% utilized the wrong antibiotic based on the clinical practice algorithm (Table 2).
DISCUSSION
The purpose of this project was to improve provider adherence to the newly modified evidence-based clinical practice algorithm for the management of AOM in patients ages 2 to 18 years of age. Clinical practice guidelines were present at the UC/ED; however, they were not being utilized. The watch-and-wait component of the algorithm was created and presented to the providers to allow for standardization and quick, easy access to the algorithm for the management of AOM.
First Objective: Providing the Algorithm and Clinician Education
There were three primary objectives for this project. The first was providing clinicians with an up to date, evidenced-based algorithm and education on diagnosis, treatment, and management of AOM for pediatric patients. This objective was achieved by reviewing the available knowledge and recommendations from multiple professional organizations. It was found that the clinical practice guidelines at the UC/ED were up to date with first-line antibiotic recommendations; however, this did not include the watch-and-wait component.
The literature supports the use of up-to-date clinical practice guidelines to aid in recommended diagnosis and management of AOM and the reduction of antibiotic usage. Clinical practice guidelines created by the AAP should be followed when treating patients with ear complaints with special attention to delaying antibiotic prescriptions by utilizing the watch-and-wait recommendation.7 Watching and waiting helps eliminate the side effects of possible unnecessary antibiotic use and results in similar outcomes when compared to a placebo.8 The education and modified algorithm aided in the overall increased adherence to the clinical practice guidelines. The pre-intervention audit revealed only 38% of providers were utilizing the clinical practice algorithm but after the interventions, there was a 35-point increase when comparing pre-intervention and postintervention data. The literature outlines the importance of following recommendations and data analysis from this project also revealed an 18% decrease in antibiotic prescriptions which supports the use of the algorithm.7
Second Objective: Implementation of Watch-and-Wait
The second objective was the implementation of the watch-and-wait component for an evidenced-based algorithm for the management of AOM for patients between the age of 2 and 18 years. This objective was achieved through the creation and implementation of the watch-and-wait section of the algorithm. Chart audits were completed to determine if the revised evidence-based clinical practice algorithm and educational module improved adherence rates for the management of AOM in patients in an 8-week timeframe. Antibiotic resistance along with inappropriate antibiotic prescribing is an important health issue which most providers view as more of an outpatient provider issue.9 A trend of prescribing outside of current clinical recommendations was recognized by outpatient providers at this UC/ED. Pre-intervention data revealed that providers were diagnosing AOM in their patients properly, but not utilizing the clinical practice guideline algorithm correctly or consistently. Postintervention data revealed a 35-point increase in adherence to the clinical practice guideline algorithm which led to better management of pediatric patients with ear complaints.
The watch-and-wait” component was added to the current AOM management algorithm and should be utilized in any patient over the age of 24 months with non-severe symptoms. This method is supported by the AAP and allows for a watchful waiting period of 48 to 72 hours prior to initiating antibiotics for AOM5. The pre-intervention data showed that no patients were managed with the watch-and-wait method. The postintervention data showed that 7% (n=6) were managed with the watch-and-wait method. The literature supports the initiation of this method as it decreases unnecessary antibiotic use.
The algorithm was also reviewed for current antibiotic recommendations and was found to be accurate in that area. The first-line antibiotic recommendation for the treatment of acute otitis media is high-dose amoxicillin for 5 to 10 days.11 To help combat antibiotic resistance and promote antibiotic stewardship, it is imperative to follow all clinical practice guideline recommendations, which includes first-line antibiotic choice2. The pre-intervention data revealed that only 27% of the charts were managed with the first-line antibiotic choice, while the postintervention revealed that 96% of the charts were managed with the first-line antibiotic.
Third Objective: Education Around Application of the Algorithm
The third and final objective was education around the application of the algorithm. Provider and parent education was essential to the success of this project. Inappropriate antibiotic usage could be decreased by more than 45% if providers accurately diagnosed patients by recognizing differences between viral and bacterial infections, providing patient education, and improving access to decision-making tools.10 Education presented to all providers in this UC/ED allowed for increased knowledge on examination, diagnosis, and treatment for patients with ear complaints.
Anecdotally, providers noted that the easy-to-follow algorithm, with additional education, helped them better manage patients, along with increasing their confidence in educating caregivers. They did not feel pressured to prescribe antibiotics when not appropriate and felt most parents/caregivers were satisfied with the management at the time of the.
This objective was achieved by analyzing the data and determining that there was increased utilization of the algorithm and overall improved outcomes such as increased use of the watch-and-wait recommendation, decreased antibiotic use, and the correct antibiotic prescribed 96% of the time. Education included appropriate first-line antibiotic choice along with duration when an antibiotic was deemed necessary. Current clinical practice guidelines recommend a 10-day course of antibiotics for the treatment of acute otitis media although shorter duration of antibiotics can be effective for the management and treatment of acute otitis media.12 Pending further studies, this medication duration could change the current clinical practice guidelines.
LIMITATIONS
This study was limited to UC/ED providers at this location. The primary care and ear, nose, and throat clinic staff were not included. Reports through EPIC for specific ICD codes for AOM and charts that did not have those codes but still had AOM as a specific diagnosis may have been missed in the query. The timing of data collection was also a limitation; the project was conducted between the months of August and October, which historically have lower numbers of illnesses including AOM. If the study were done between the months of November through February, the number of charts retrieved would most likely have been larger. Lastly, knowing whether the educational posters in the exam rooms were beneficial to the caregivers/patients was not measured; therefore, the only way of knowing if that intervention was effective was from informal feedback from the providers.
SUSTAINABILITY
It is essential for providers to remain up to date on current clinical practice guidelines for the management and treatment of acute otitis media to provide the patient with the best possible care. This project showed a 35-point increase in adherence to clinical practice guidelines. Continued monthly and bimonthly education to both providers and nurses will take place in the clinical setting. Next steps include presenting the current algorithm along with the watch and wait component to the primary care, pediatric, and ear, nose, and throat clinic providers within this network. Education via advertisements and social media pages will continue to be presented to the public to inform them of the current guidelines and management of AOM.
CONCLUSION
Proper management of AOM, along with the importance of following clinical practice guidelines, were priorities throughout this project. Clinic providers at this UC/ED were not following current clinical practice guidelines for the management and treatment of acute otitis media as they were unaware of the most recent updates, which led to inappropriate management and treatment of acute otitis media. The modification of the evidence-based clinical practice guidelines adding an easy-to-follow watch-and-wait component and education to providers in this UC/ED played an essential role in the success of this project. There was a 35-point increase in adherence to clinical practice guidelines along with an 18% decrease in antibiotic prescriptions following the interventions. Sustainability will be achieved through continuous education to staff, providers, and the community.
REFERENCES
- Danishyar A, Ashurst J. Acute otitis media. In: StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK470332/. Accessed August 5, 2023.
- Spoiala E, Stanciu G, Bild V, et al. From evidence to clinical guidelines in antibiotic treatment in acute otitis media in children. Antibiotics (Basel). 2021;10(1):52.
- Meek R. Middle ear, eustachian tube, inflammation/infection. Medscape. Available at:
https://emedicine.medscape.com/article/858777-overview#a6. Accessed August 5, 2023. - Venekamp R, Damoiseaux R, Schilder A. Acute otitis media in children. Am Fam Physician. 2017;95(2):109-110.
- Lieberthal A, Carroll A, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Am Acad Pediatr. 2013;131(3):e964-e999.
- Antibiotic prescribing and use. 2022. Centers for Disease Control and Prevention.
Available at: https://www.cdc.gov/antibiotic-use/community/downloads/factsheet-preventing-ear-infection_508.pdf. Accessed August 5, 2023. - Gaddey HL, Wright MT, Nelson TN. Otitis media: rapid evidence review. Am Fam Physician. 2019;100(6):350–356.
- Evridiki K, Vouloumanou E, Karageorgopoulos M, et al. Antibiotics versus placebo or watchful waiting for acute otitis media: a meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2009;64(1):16-24.
- Zetts RM, Stoesz A, Garcia AM, et al. Primary care physicians’ attitudes and perceptions towards antibiotic resistance and outpatient antibiotic stewardship in the USA: a qualitative study. BMJ Open. 2020;10(7):e034983.
- Tedijanto C, Grad YH, Lipsitch M. Potential impact of outpatient stewardship
interventions on antibiotic exposures of common bacterial pathogens. Elife. 2020 Feb 5;9:e52307. - Meissner H. Understanding otitis media in 2018. AAP News. June 26, 2018. Available at:
https://www.aappublications.org/news/2018/06/26/idsnapshot062618. Accessed August 5, 2023. - Uhl B, Boutzoukas A, Gallup N, et al. Increasing adherence to acute otitis media treatment duration guidelines using a quality improvement approach. Pediatr Qual Saf. 2021;15;6(6):e501.
Author affiliations: Jessica Crandall, DNP, MSN – ARNP, Greater Regional Health, Creston, IA. Misty Schwartz, PhD, RN College of Nursing, Creighton University, Omaha, NE.
Read More
- Antibiotic Stewardship In Pediatric Acute Otitis Media—Pearls And Pitfalls
- Urgent Care Management Of Acute Otitis Media In Children
- If Not Otitis Externa…Then What?