Published on
Urgent Message: Inappropriate antibiotic prescribing in the outpatient setting has been a longstanding public health challenge. An educational session implemented in a large Midwestern healthcare system group of urgent care and convenience care clinics resulted in a statistically significant reduction in antibiotic prescribing for acute sinusitis and a statistically significant increase in antibiotic guideline adherence.
Dr. Amy K. Rasmussen, DNP, FNP-C
ABSTRACT
Background: Inappropriate antibiotic prescribing in the outpatient setting is a longstanding problem and a public health challenge. Despite clear antibiotic guidelines and educational campaigns, antibiotics continue to be overprescribed for sinusitis in urgent care centers. However, there is evidence that antibiotic stewardship interventions can improve guideline adherence to manage sinusitis.
Objective: Determine the effect of an educational program on provider antibiotic prescribing practices.
Methods: This study used a one-group, pre- and poststudy design and Levin’s Change Theory Model to determine if an educational intervention decreased inappropriate antibiotic prescribing for sinusitis for providers practicing in Midwest urban urgent care and convenience care clinics. Incidentally, timing of this study provided an opportunity to compare prescribing practices between in-person and virtual care environments.
Results: Comparing each of the calculated values of z to critical or table value of z, which is +/-1.96 for an α of .05, there was a statistically significant reduction of antibiotic prescribing after the educational intervention and a statistically significant improvement in guideline adherence for diagnosis and treatment. The education intervention resulted in a 22.8% (z=10.32, p=0.000) reduction in inappropriate antibiotic prescribing and a 6.1% (z=1.95, p=0.025) increase in antibiotic guideline adherence. Additionally, there were 16.2% (p=0.001) fewer antibiotics prescribed for sinusitis during virtual care visits when compared with in-person visits.
Conclusions: The statistically significant reduction in inappropriate antibiotic prescribing for sinusitis and increase in antibiotic guideline adherence suggests provider-targeted education to be an effective intervention. The COVIC-19 pandemic provided an unexpected opportunity to explore the prescribing patterns of the same providers in virtual and in-person environments.
Key words: Acute sinusitis, antibiotic resistance, antibiotic stewardship, quality improvement
BACKGROUND
Antibiotic Use
Each year in the United States, 80 million prescriptions are written for antibiotics and 30% of those prescriptions are written for viral respiratory illnesses that should not be treated with antibiotics.1,2 Most of these prescriptions are written in outpatient care settings; of these, urgent care has the highest antibiotic prescribing rate.3 Studies have shown that about 80% of the antibiotic prescriptions written in urgent care centers each year are for sinusitis, a respiratory tract infection (RTI) that usually resolves without treatment.3-5 Inappropriately prescribed antibiotics in the outpatient setting has been a longstanding problem that continues to be a public health challenge.
Sinusitis is a common RTI that causes inflammation of the mucosal lining of the nasal passage and paranasal sinuses and is the most common complaint in outpatient urgent care centers each year in the U.S.6,7 Symptoms include runny nose, congestion, facial pain and pressure, headache, sore throat, and cough. Treatment for acute viral sinusitis is focused on symptom management, with symptoms typically resolving in 7 to 10 days. Centers for Disease Control and Prevention guidelines can help in differentiating between acute viral sinusitis and acute bacterial sinusitis.
Sinusitis is generally considered to have a bacterial etiology if symptoms persist more than 10 days without improvement; the patient experiences worsening symptoms over 3 to 4 days (such as new onset of fever, daytime cough, or nasal discharge after initial improvement); or symptoms are severe, such as fever of 102°F or higher, purulent nasal discharge, or facial pain.1 In these circumstances, antibiotic treatment is appropriate.
Sinusitis accounts for 11.1% of over 2.7 million urgent care visits each year.2,7 Ninety-eight percent of sinus infections are viral, and current national guidelines do not recommend antibiotics in treating acute viral sinusitis.8
Resistance and Stewardship
The overuse and inappropriate prescribing of antibiotics is associated with increased healthcare costs, unnecessary adverse drug effects, and the emergence, persistence, and transmission of antibiotic-resistant organisms, like methicillin-resistant Staphylococcus aureus (MRSA).4,9,10 Antibiotic-resistant organisms cause more than 2.8 million infections and 35,000 deaths in the United States each year.1 Infections caused by antibiotic-resistant organisms cost patients an estimated $35 billion in lost wages and contribute $20 billion to excess healthcare costs.1
Inappropriate use of antibiotics can have serious consequences. Antibiotic resistance is associated with antibiotic exposure and patient nonadherence to prescribed antibiotic regimens. Studies suggest that up to 40% of patients fail to complete the full course of antibiotic treatment.11 Antibiotic reactions, along with unwanted and uncomfortable effects from medications, are also the most common cause of adverse drug events resulting in physical, mental, and functional injuries.12 Using antibiotics when they are not necessary can decrease their effectiveness and reduce options for treating infections.
Antibiotic stewardship programs are designed to promote appropriate use of antibiotics, improve patient outcomes, and decrease the spread of resistant organisms.13 There is evidence that antibiotic stewardship interventions can improve guideline adherence to manage sinusitis diagnoses.7 Targeted education on appropriate use of antibiotics for sinusitis is needed in urgent care settings to help reduce inappropriate antibiotic prescribing.
Inappropriate use of antibiotics in urgent care centers is a costly problem that contributes to increased healthcare costs, increased antibiotic resistance, and exposing patients unnecessarily to antibiotics and their side effects.1,2,1110 Studies suggest that even with current prescribing guidelines, inappropriate prescribing is influenced by providers’ lack of knowledge, attitudes regarding antibiotic use and resistance, and patient expectations and pressures to prescribe.14,15 Understanding what influences this practice is imperative in order to design effective interventions.3
Clinical Question
For urgent care and convenience care providers, does the implementation of an antibiotic stewardship training and education program reduce the number of unnecessary prescribed antibiotics for sinusitis over a 2-month period of time, compared with no training or education?
Literature Search
A systematic literature search was conducted in PubMed, MEDLINE, and Cumulative Index to Nursing and Allied Health Literature (CINAHL). Abstracts of relevant papers were reviewed and hand searching of other relevant publications was used to identify additional sources. The Cochrane Library was also searched for additional publications. Finally, the CDC and Infectious Disease Society of America (IDSA) websites were searched for additional publications relevant to the clinical question.
A broad search strategy was used to locate current prescribing habits of antibiotics for respiratory illnesses. Keywords and search terms that were used alone and in combination that related to the clinical question were: antibiotic stewardship, sinusitis, provider, urgent care, and acute respiratory illness. The search strategy used Medical Subject Headings (MeSH).
The initial search resulted in over 5,000 articles; to identify relevant publications, inclusion criteria included: date range of 2014 to 2021, adults 18 to 65 years of age, full-text, peer-reviewed, English language, and outpatients. The search excluded publications that discussed the pediatric population, as well as literature related to inpatient settings, chronic illnesses such as cystic fibrosis or acute exacerbation of chronic obstructive pulmonary disease, and pneumonia. This initial search resulted in 29 relevant publications; the Cochrane Library resulted in two additional articles. Results were manually checked for duplicates and for articles that were outside of the search parameters. Reference sections of relevant publications were also reviewed. The comprehensive literature review of PubMed, MEDLINE, CINAHL, the Cochrane Library and government websites resulted in adequate literature to support the clinical question.
DESIGN AND METHODS
Setting
An educational antibiotic stewardship intervention was implemented at 10 urgent care clinics and seven convenience care clinics at a Midwest urban healthcare network using the Lewin’s Change Theory. Due to the COVID-19 pandemic, the urgent care setting developed a virtual urgent care platform in the summer of 2020 to treat and diagnose those patients that did not want traditional in-person visits. The virtual platforms are managed by the same providers in the urgent care and convenience care clinics. The virtual urgent care clinic was used to capture some of the post study data.
Study Design
The project used a one-group pre/poststudy design to determine if an education intervention decreased inappropriate antibiotic prescribing among urgent care and convenience care providers (medical doctors [MDs], physician assistants [PAs], and nurse practitioners ]NPs]) through the increased use of prescribing guidelines for sinusitis. Antibiotic prescribing data were collected retrospectively from patient records dated January 1, 2020 through February 29, 2020, to establish a pre-intervention baseline. After the project education intervention, comparison data were collected from the same time period in 2021 (January 1through February 28) to account for the seasonality of RTI.
Population
The provider population included all providers (MDs, PAs, and NPs) from the network of urgent care and convenient care clinics. The clinics are staffed with 76 full and part-time MDs, PAs, and NPs and 64 casual MDs, PAs, and NPs. Each clinic utilized the same EMR and was part of the same healthcare organization. All providers floated among the 10 urgent care clinics and seven convenience care clinics. Providers’ experience level ranged from new graduates to experienced providers.
Sampling
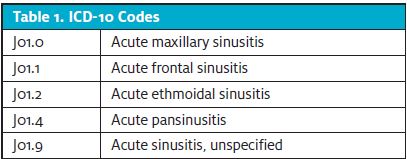
The sample included adult patients treated for acute sinusitis from January 1, 2020, through February 29, 2020, and January 1, 2021, through February 28, 2021. Inclusion criteria were a) age 18 or older and b) diagnosed with acute sinusitis using five ICD codes (Table 1). Patients were excluded from the study if they had a concomitant infection (ie, acute otitis media, strep pharyngitis) which might influence the antibiotic choice. During the pre- and poststudy periods, there were 495 and 383 patients diagnosed with acute sinusitis based on the International Classification of Disease (ICD) codes before and after the educational intervention, respectively.
PROCEDURES
Phase 1
Baseline retrospective chart audit
A retrospective chart audit was conducted to establish a baseline of the prescribing rate and guideline use for the urgent care and convenience care providers. The information technology (IT) department at the healthcare organization provided an electronic report to identify a list of patients who met inclusion criteria (ICD sinusitis codes, patients >18-years-old, treatment received at one of the urgent care or convenience care clinics, and date range of January 1, 2020, through February 29, 2020). These initial data provided 532 patient charts for review.
The student investigator performed all chart reviews. The CDC sinusitis clinical treatment guideline presented in the educational session was used as a benchmark to determine inappropriate prescribing of antibiotics (ie, antibiotic is not needed, the wrong antibiotic is prescribed, or the wrong dose is given or the antibiotic is prescribed for the wrong length of time). For each chart reviewed, an Excel spreadsheet was used to collect data. Data recorded were 1) Was an antibiotic prescribed? (yes/no) and 2) Were CDC sinusitis guidelines followed? (yes/no). Charts that showed concomitant infection during the visit, which could have influenced antibiotic choice, were eliminated from the study. After review, 495 charts were appropriate for the prestudy data collection.
Phase 2
Antimicrobial stewardship education
Education was provided to urgent care and convenience care providers at a department staff meeting on December 13, 2020. The meeting was conducted via Microsoft Teams. Eighty-nine providers (64% of urgent care/convenience care providers) attended the meeting. All providers had access to the educational handouts, as well as a recording of the presentation. The educational PowerPoint content covered purpose and selection of antibiotics for sinusitis, the significance of overuse of antibiotics, antibiotic effect on resistance, and evidence-based treatment guidelines from the CDC on treating sinusitis. The presentation lasted 20 minutes.
Posteducation chart audit
Because sinusitis is most prevalent in the winter months, posteducation data were collected from January 1, 2021, through February 28, 2021, to match the prestudy data from the previous year. The data collection process was identical to the retrospective data collection, and 113 patient charts were appropriate for review. Eighteen charts were eliminated due to concomitant infection that required antibiotic treatment, leaving a total of 95 charts. Given the large discrepancy between the pre and post patient visit data, the student investigator had to address the issue of low in-person clinic encounters.
To improve access to care during the pandemic, the healthcare organization where the study took place launched a virtual urgent care synchronous (real-time) platform in August of 2020. An asynchronous (no real-time interaction between patient and provider) telehealth platform existed prepandemic; however, patient usage was minimal. Using the same inclusion criteria, the IT department identified an additional 310 patient records from the virtual care environments data. After review, 288 virtual visits were appropriate for the study. A total of 383 charts were deemed appropriate for post study analysis.
RESULTS
Pre-intervention data were compared to postintervention data (Table 2), looking specifically at the overall number of antibiotics prescribed for sinusitis and adherence to sinusitis CDC guidelines.
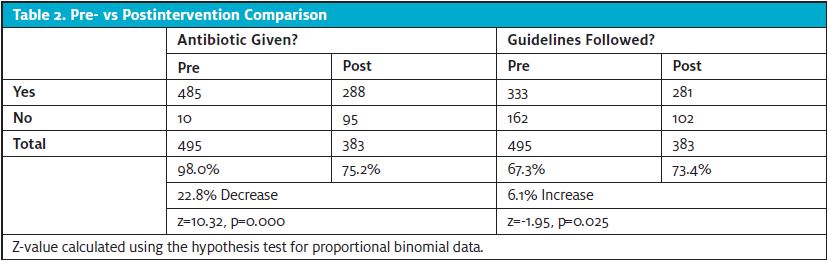
Antibiotic prescribing pre- and postintervention showed a decrease of 22.8% (z=10.32, p=0.000). Antibiotic guideline adherence showed an increase of 6.1% (z=1.95, p=0.025). Comparing each of the calculated values of z to critical or table value of z, which is +/-1.96 for an α of .05, there was a statistically significant reduction of antibiotic prescribing after the educational intervention and a statistically significant improvement in guideline adherence for diagnosis and treatment.
The outcome objective for this project was to have at least a 5% reduction in inappropriately prescribed antibiotics for sinusitis by urgent care and convenience care providers when comparing pre- and poststudy; this was met. The second goal was to have at least 85% of the providers utilize an evidence-based antibiotic recommendation guideline for treatment of sinusitis. The data showed a statistically significant improvement from the prestudy data, though only 73.4% of providers used the antibiotic guidelines, indicating that the objective was not met.
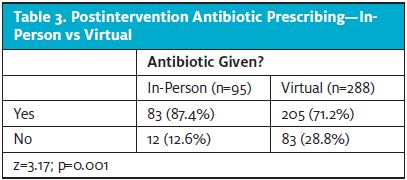
This study provided a unique opportunity to compare prescribing practices between in-person and virtual care environments. A comparison was made between provider antibiotic prescribing rates postintervention and between in-person visits (n=95) and virtual visits (n=288). In-person antibiotics given was 87.4% (n=83), and virtual visit antibiotics given was 71.2% (n=205). There was a statistically significant reduction, 16.2% (p=0.001) (Table 3), in antibiotics prescribed when comparing in-person to virtual care visits.
PROTECTION OF HUMAN SUBJECTS
The project directly involved the urgent care and convenience care providers and indirectly affected the patients at the clinic sites. The provider names were kept anonymous during the collection of retrospective chart review and poststudy chart review data. All information used for this project was kept on a secured flash drive. All research data obtained from the EMR were collected and recorded in a deidentified manner on an Excel spreadsheet. Any sharing of project information was through encrypted email. The Institutional Review Board (IRB) process at the university and the healthcare organization where the study took place was followed.
VALIDITY
The statistically significant results suggest that the educational intervention aimed at reducing inappropriate antibiotic prescribing of sinusitis using evidence-based guidelines from the CDC was effective in reducing inappropriate antibiotic prescribing for sinusitis. Specific measures were implemented to preserve the integrity of the data and reduce threats to the internal and external validity of the study. To promote internal validity of the independent variable (provider education), the antibiotic stewardship education was administered by only the student investigator. The data collection tool remained consistent to avoid changes in the collection procedure. To promote external validity, inclusion and exclusion criteria were used to clearly define the population being studied.
LIMITATIONS
This study had several limiting factors.
First, with the poststudy data collected, the student investigator cannot determine if the antibiotic stewardship education presented to the providers was the sole influence for the decrease in antibiotic prescribing and increase in guideline adherence. Outside influences that may have contributed to the study results could have come from attendance at educational conferences, webinars, professional journal articles, or the use of other antibiotic stewardship guidelines for sinusitis.
Second, the study’s 2-month observation period following the intervention, January through February 2021, is insufficient to understand the sustainability of the decreased antibiotic prescribing.
Third, the COVID-19 pandemic may have had a significant impact on the research validity.
Fourth, the asynchronous virtual environment provided guideline adherence recommendations to prompt the provider in making a decision on whether or not an antibiotic was warranted. This could have contributed to providers following guideline adherence and not prescribing antibiotics for sinusitis infections.
Fifth, the intervention was implemented with urgent and convenience care providers within a healthcare organization, excluding primary care providers and clinics associated with the network.
This study was in process prepandemic and continued during the pandemic. As a result, many individuals who may have typically sought care in an urgent care or convenience care setting may have elected to not have their symptoms treated. This could result in a study with a sample that is less representative of the target population, risking the generalizability of the research. Also, there could have been patient pressure experienced in the in-person visits compared to the virtual visits, resulting in increased prescribing.
DISCUSSION
Pre-intervention data were compared to postintervention data, looking specifically at the overall number of antibiotics prescribed for sinusitis and adherence to sinusitis CDC guidelines. Antibiotic prescribing pre- and postintervention showed a decrease of 22.8% (z=10.32, p=0.000). Antibiotic guideline adherence showed an increase of 6.1% (z=1.95, p=0.025).
The statistically significant results suggest that the educational intervention aimed at reducing inappropriate antibiotic prescribing of sinusitis using evidence-based guidelines from the CDC was effective in reducing inappropriate antibiotic prescribing for sinusitis.
SIGNIFICANCE OF FINDINGS
The project used a one-group pre- and poststudy design to determine if an education intervention decreased inappropriate antibiotic prescribing among urgent care and convenience care providers through the increased use of prescribing guidelines for sinusitis. The results were consistent with findings found in the literature review that showed evidence of a decrease in antibiotic prescribing, which suggests provider-targeted education to be an effective intervention.
The study was in process pre COVID-19 pandemic and continued during the pandemic. As a result, many individuals who may have typically sought care in an urgent care or convenience care setting, may have elected to not have their symptoms treated. This caused a large discrepancy between pre and post patient visit data. To address the issue of low in-person clinic encounters, virtual care visits for sinusitis were used in the post study data collection. The study data showed that patients were more likely to receive an antibiotic in an in-person visit compared to virtual care visits.
Implications for Future Projects
Inappropriately prescribed antibiotics in the outpatient setting have been a longstanding problem, and continue to be a public health challenge. Given the lack of new antibiotics, increased antibiotic stewardship efforts have been undertaken to prevent and slow antibiotic resistant infections.2
This quality-improvement project suggests an education intervention can reduce the rate of inappropriately prescribed antibiotics; however, the 2-month study period does not reflect sustainability of continued antibiotic prescribing practice. This project focused solely on sinusitis. Future studies broadening the scope of the educational intervention to include all other conditions for which antibiotics are frequently prescribed may be beneficial in improving inappropriate prescribing.
To further advance effective evidence-based antibiotic stewardship efforts, future projects should focus on implementation and sustainability strategies within ambulatory settings, especially urgent care and convenience care settings. With the increased use of telehealth and virtual care, there is also a need for studies that explore prescribing practices between in-person and virtual visits, as well as factors that influence provider prescribing in these settings.
CONCLUSION
Inappropriate use of antibiotics is associated with increased healthcare costs, unnecessary adverse drug effects, and the emergence, persistence, and transmission of antibiotic-resistant organisms.4,9,11 Antibiotic stewardship programs are designed to promote appropriate use of antibiotics, improve patient outcomes, and decrease the spread of resistant organisms.13 The results of this study are consistent with other similar studies found in the literature and suggest that antibiotic stewardship education is an effective intervention in influencing provider antibiotic prescribing for viral sinusitis in the urgent care setting. This study included providers working in the urgent care and convenience care clinics in a single healthcare organization during the COVID-19 pandemic and there were changes to healthcare-delivery systems, including the transition from in-person to virtual visits. This had an impact on postintervention data collection and may have confounded the results; however, it also provided an unexpected opportunity to explore the prescribing patterns of the same providers in the different care environments. In addition, the timeframe for this study was insufficient to understand whether the improvements would be sustained. Because of these limitations, the findings from this study cannot be generalized to other infection types or care settings, and therefore future research is needed.
REFERENCES
- Barlam TF, Morgan JR, Wetzler LM, Christiansen CL, Drainoni ML. Antibiotics for respiratory tract infections: A comparison of prescribing in an outpatient setting. Infect Control Hosp Epidemiol. 2015;36(2):153-159.
- Center for Disease Control and Prevention. Antibiotic use in outpatient settings, 2017. https://www.cdc.gov/antibiotic-use/stewardship-report/outpatient.html. Published August 2019. Accessed January 17, 2021.
- Chater A, Courtenay M. Community nursing and antibiotic stewardship: The importance of communication and training. Br J Community Nurs. 2019;24(7):338-342.
- Dekker AR, Verheij TJ, van der Velden AW. Inappropriate antibiotic prescription for respiratory tract indications: Most prominent in adult patients. Fam Pract. 2015;32(4):401-407.
- Dosh SA, Hickner J, Mainous AG, Ebell MH. Predictors of antibiotic prescribing for nonspecific upper respiratory infections, acute bronchitis, and acute sinusitis. J Fam Pract. 2015;49(5):407-414.
- Hingorani R, Mahmood M, Alweis R. Improving antibiotic adherence in treatment of acute upper respiratory infections: A quality improvement process. J Community Hosp Intern Med Perspect. 2015;5(3).
- Incze M, Redberg RF, Katz MH. Overprescription in urgent care clinics: The fast and the spurious. JAMA Intern Med. 2018;178(9):1269-1270.
- Jones-Holley M, Veenma-Goodwin TA. A multimodal intervention to reduce antibiotic use for common upper respiratory infections in the urgent care setting. The Journal of Urgent Care medicine. 2015;81(1):92-93.
- Jung IY, Kim JJ, Lee SJ, et al. Antibiotic-related adverse drug reactions at a tertiary care hospital in South Korea. Biomed Res Int. 2017;2017:4304973-7.
- Tillekeratne L, Bodinayake CK, Dabrera T, et al. Antibiotic overuse for acute respiratory tract infections in Sri Lanka: A qualitative study of outpatients and their physicians. BMC Fam Pract. 2017;18(37):37-47.
- Link TL, Townsend ML, Leung E, Kommu S, Vega RY, Hendrix CC. Reducing inappropriate antibiotic prescribing for adults with acute bronchitis in an urgent care setting. Adv Emerg Nurs J. 2016;38(4):327-335.
- McDonagh MS, Peterson K, Winthrop K, Cantor A, Lazur BH, Buckley DI. Interventions to reduce inappropriate prescribing of antibiotics for acute respiratory tract infections: Summary and update of a systematic review. J Int Med Res. 2018;46(8):3337-3357.
- Rezal R, Hassali M, Alrasheedy A, Saleem F, Yusof F, Godman B. Physicians’ knowledge, perceptions and behaviour towards antibiotic prescribing: A systematic review of the literature. Expert Rev Anti Infect Ther. 2015;13(5):665-80.
- Sanchez GV, Fleming-Dutra KE, Roberts R.M, Hick LA. Core elements of outpatient antibiotic stewardship. MMWR Surveill Summ. 2016;65(6):1-12.
- Sybold M., Tse-Faber H. Antibiotic stewardship and sinusitis: A quality improvement project. The Journal of Urgent Care Medicine. 2020;15(2):19-24. https://www.jucm.com/antibiotic-stewardship-and-sinusitis-a-quality-improvement-project/
Author affiliations: The author has no relevant financial relationships with any commercial interests.
Read More
- Antibiotic Stewardship And Sinusitis: A Quality Improvement Project
- On Antibiotic-Seeking, Predicting Prognosis In Rhinosinusitis And Mortality In Head Injuries, And When To Use Antibiotics In Conjunctivitis
- Antibiotic Stewardship In Pediatric Acute Otitis Media—Pearls And Pitfalls

