Published on
Urgent message: Though use of point-of-care ultrasound in the evaluation of first trimester pregnancy complaints is not as common in the urgent care setting as it is in th ED, its use can expedite diagnosis and, potentially, lifesaving treatment.
Benjamin Mati MD and Richard Rutherford, MD
Citation: Mati B, Rutherford R. Point-of-care ultrasound diagnosis of ruptured ectopic pregnancy in an urgent care setting. J Urgent Care Med. 2023;17(7):19-21.
Key words: ultrasound, POCUS, ectopic pregnancy, urgent care, ruptured ectopic pregnancy, intrauterine device, IUD
ABSTRACT
Pregnancy while using an intrauterine device is rare, but when it occurs the risk of ectopic pregnancy is increased. Rupture of ectopic pregnancy is associated with high morbidity and mortality that can be mitigated with prompt diagnosis and treatment. Point-of-care ultrasound is easily learned, expedites diagnosis and treatment, and improves outcomes in patients with ruptured ectopic pregnancy.
INTRODUCTION
Ruptured ectopic pregnancy is a rare diagnosis but it is associated with high morbidity and mortality.1 Prompt diagnosis leads to expedited treatment, which is associated with better outcomes.2 Point-of-care-ultrasound (POCUS) use in the evaluation of first trimester pregnancy complaints is considered standard of care in emergency departments.3,4,5 However, its adoption is not as widespread in the urgent care setting. This case highlights how POCUS use in the urgent care setting potentially saved the life of a pregnant woman with a ruptured ectopic pregnancy. We illustrate how POCUS can augment history and physical exam to lead to expedited diagnosis and treatment.
CASE PRESENTATION
A 21-year-old G2P1 female presented to urgent care with complaints of abdominal cramping and pain. She reported starting her menstrual cycle the day prior and having associated pelvic cramping, nausea, and vomiting that were progressively worsening. She reported an intrauterine device (IUD) placed about a year prior. She also reported a negative home pregnancy test 3 days ago. She came to the urgent care for symptomatic relief. However, upon standing to walk to the restroom to provide a urine sample in the urgent care, she had a syncopal episode.
She was found to be diaphoretic but awake, alert and oriented. Her heart rate was 132, blood pressure 85/56 then 100/66, oxygen saturation 98% on room air. She had mild tenderness to palpation of the abdomen. She was adamant that she did not want EMS called and did not want to be brought to the emergency department. She reported that she often feels lightheaded during her menstrual cycles and this was not far from how she usually felt.
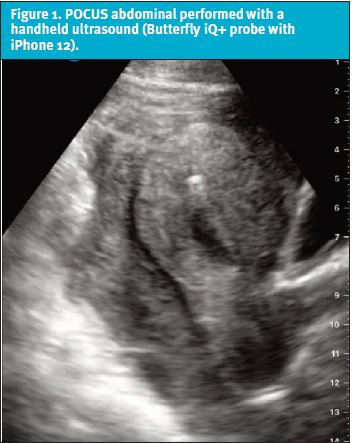
Upon re-evaluation, a POCUS abdominal protocol was performed with a handheld ultrasound (Butterfly iQ+ probe with iPhone 12) while nursing placed an intravenous (IV) catheter, collected labs, and started IV fluids. (See Figure 1.)POCUS showed no intrauterine pregnancy. A thickened myometrium with a small amount of free fluid and a large amount of mixed echogenic material concerning for blood was found in the pelvis. A hyperechoic structure was identified within the uterus, consistent with an IUD. There was free fluid in the right upper quadrant (RUQ) and in the left upper quadrant (LUQ). Her right ovary was difficult to identify, though an abnormal-appearing cystic structure was noted outside of the uterus.
The differential diagnosis at this point included ruptured ovarian cyst, ruptured ectopic pregnancy, tubo-ovarian abscess, acute appendicitis, diverticulitis, and ruptured abdominal aorta. Although she had an IUD and reported a recent negative pregnancy, the POCUS was concerning for an abnormal appearing adnexal structure and pelvic free fluid.
We reassessed her vital signs, which showed a slightly improved blood pressure but persistent tachycardia. On further conversation, with the information provided by the POCUS discusses and shown to the patient, she was amenable at this point for transport to the local emergency department. An ambulance was called immediately, and arrived prior to any labs returning. She was unable to provide urine for a point-of-care pregnancy test.
While in route to the ED, she became hypotensive. She arrived in hemorrhagic shock and experienced two more syncopal episodes with mean arterial pressures dropping below 50. In the emergency department, a massive transfusion protocol was started, and she ultimately received five units of packed red blood cells and was started on pressors.
A bedside ultrasound performed by the EM physician confirmed the findings of the urgentologist. In consultation with obstetrics, she was brought directly to the operating theater, where a right tubal ruptured ectopic pregnancy and over 2 liters of hemoperitoneum were identified. She underwent a successful right salpingectomy and the IUD was left in the uterus. She was discharged 2 days later and subsequently had the IUD removed by her outpatient provider.
DISCUSSION
Hemorrhage from ruptured ectopic pregnancy is among the most common causes of first trimester mortality in North America.1,6 During the COVID-19 pandemic, an increased rate of ruptured ectopic pregnancies has been noted.7,8 Timely and accurate diagnosis is critical to providing definitive treatment, often emergent surgery.
Since these patients are often young and healthy, vital sign abnormalities can be late manifestations of shock. It is important to avoid cognitive biases such as anchoring or premature closure; routinely incorporating the use of symptom-based POCUS protocols into patient evaluations can help protect urgentologists against such biases.
In this particular case, the identification of free fluid in the pelvis pushed ruptured ectopic pregnancy to the top of the differential diagnosis despite the report of a negative home pregnancy test. This noninvasive, affordable, and easily learned intervention allowed the clinician to arrive at the correct, life-threatening diagnosis much sooner than would have been possible with a traditional diagnostic approach.
Ectopic pregnancies have a prevalence of 1%-2% and cause about 2.7% of pregnancy-related deaths.2,6,9,10. In the acute care settings, abdominal pain and vaginal bleeding should raise concern for the potential of an ectopic pregnancy.6,11Although up to half of women diagnosed with an ectopic pregnancy have no identifiable risk factors, some potential risk factors include fallopian tube pathology, pelvic inflammatory disease, previous ectopic, and pregnancy while an IUD is in place.2
IUDs are the most commonly used long-acting reversible contraceptive methods worldwide.12 They are extremely effective at preventing pregnancy, providing up to a 99% effective prevention rate.2 However, when pregnancy occurs in the presence of an IUD, the risk for an ectopic pregnancy is significantly increased, up to 53%.2
A cornerstone of efficient and effective diagnosis of first trimester pathology is point-of-care ultrasound. POCUS is standard of care for symptomatic pregnant patients in the emergency department3,4,13 and is becoming more common in urgent care, as well.14 POCUS decreases time to diagnosis, time to obstetrics consult, and time to definitive management for ruptured ectopic pregnancy when compared with ultrasound conducted by a radiologist or ultrasound technician6,11,15,16,17 POCUS has also been found to enable nonsurgical treatments to be offered more frequently; for example, in cases of early detection of cervical pregnancy, methotrexate may be offered.18
POCUS Findings
Stone, et al demonstrated a simple transabdominal POCUS protocol to assess for the presence of ruptured ectopic: 1.) evaluate for IUP, 2.) evaluate for free fluid in the pelvis and 3.) evaluate for free fluid in the RUQ/LUQ.16 A full bladder assists with visualization of IUP and pelvic free fluid, but should not cause delay of evaluation. The presence of an intrauterine yolk sac seen as a hyperechoic ring within an anechoic fluid collection is the first definitive evidence of an IUP. This can generally be seen on transabdominal ultrasound at around six weeks of gestation.11 Most ectopic pregnancies are tubal and can be seen as an extra-uterine yolk sac or embryo.11 The incidence of heterotopic pregnancy outside of assisted fertilization is very rare.11 Outside of these relatively uncommon risk factors, the presence of an intrauterine pregnancy makes an ectopic pregnancy unlikely.11,17
In women presenting with a positive pregnancy test and symptoms of pelvic pain and/or bleeding, a POCUS showing lack of an IUP and the presence of free fluid in the pelvis and/or RUQ is strongly suggestive of ruptured ectopic pregnancy.19 As in our case, these findings should trigger immediate transfer to an emergency department for evaluation by an obstetrician.
CONCLUSION
This case illustrates the importance of avoiding premature closure and anchoring bias in urgent care evaluations. It also highlights the value of POCUS use in the urgent care setting, specifically in evaluation of first trimester pregnancy presentations and protection against cognitive biases. Relying too heavily on initial pieces of information (presence of IUD and report of a negative home pregnancy test) would have limited the differential in this case, delayed the diagnosis and endangered the patient. Without POCUS, evidence of a ruptured ectopic would have been significantly delayed, preventing prompt transfer for definitive management.
The patient described in this case report consented to its publication.
REFERENCES
- Pregnancy Mortality Surveillance System | Maternal and Infant Health | CDC. Published June 23, 2022. Available at: https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm. Accessed August 17, 2022.
- Hendriks E. Ectopic Pregnancy: diagnosis and management. Ectopic Pregnancy. 2020;101(10):8.
- Durham B, Lane B, Burbridge L, Balasubramaniam S. Pelvic ultrasound performed by emergency physicians for the detection of ectopic pregnancy in complicated first-trimester pregnancies. Ann Emerg Med. 1997;29(3):338-347.
- Hahn SA, Lavonas EJ, Mace SE, et al, American College of Emergency Physicians Clinical Policies Subcommittee on Early Pregnancy. Clinical policy: Critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2012;60(3):381-390.e28.
- ACEP Board of Directors. Ultrasound Guidelines: Emergency, Point-of-care, and Clinical Ultrasound Guidelines in Medicine. ACEP Policy Statement. Published online 2016. Available at: https://www.acep.org/globalassets/new-pdfs/policy-statements/ultrasound-guidelines—emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdf. Accessed March 3, 2023.
- Urquhart S, Barnes M, Flannigan M. Comparing time to diagnosis and treatment of patients with ruptured ectopic pregnancy based on type of ultrasound performed: a retrospective inquiry. J Emerg Med. 2022;62(2):200-206.
- Casadio P, Youssef A, Arena A, et al. Increased rate of ruptured ectopic pregnancy in COVID‐19 pandemic: analysis from the north of Italy. Ultrasound Obstet Gynecol. 2020;56(2):289-289.
- Dvash S, Cuckle H, Smorgick N, et al. Increase rate of ruptured tubal ectopic pregnancy during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol. 2021;259:95-99.
- Gaetani SL, Garbade GJ, Haas SI, et al. A ruptured ectopic pregnancy in a patient with an intrauterine device: a case report. Radiol Case Rep. 2021;16(12):3672-3674.
- Jones D, Kummer T, Schoen J. Ruptured ectopic pregnancy with an intrauterine device: case report and sonographic considerations. Clin Pract Cases Emerg Med. 2020;4(4):559-563.
- Moake MM, Price AB, Titus MO, Barnes RM. Point-of-care ultrasound facilitates management of ruptured ectopic pregnancy. Pediatr Emerg Care. 2021;37(5):282-285.
- Buhling KJ, Zite NB, Lotke P, Black K. Worldwide use of intrauterine contraception: a review. Contraception. 2014;89(3):162-173.
- Blaivas M, Sierzenski P, Plecque D, Lambert M. Do emergency physicians save time when locating a live intrauterine pregnancy with bedside ultrasonography? Acad Emerg Med Off J Soc Acad Emerg Med. 2000;7(9):988-993.
- Jackson DN, Planinic P. An urgent care approach to complications and conditions of pregnancy part 2. J Urgent Care Med. Available at: https://www.jucm.com/an-urgent-care-approach-to-complications-and-conditions-of-pregnancy-part-2. Accessed July 9, 2022.
- Rodgerson JD, Heegaard WG, Plummer D, et al. Emergency department right upper quadrant ultrasound is associated with a reduced time to diagnosis and treatment of ruptured ectopic pregnancies. Acad Emerg Med. 2001;8(4):331-336.
- Stone BS, Muruganandan KM, Tonelli MM, et al. Impact of point-of-care ultrasound on treatment time for ectopic pregnancy. Am J Emerg Med. 2021;49:226-232.
- Moore C, Todd WM, O’Brien E, Lin H. Free fluid in Morison’s Pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007;14(8):755-758. doi:10.1197/j.aem.2007.04.010
- Casikar I, Reid S, Condous G. Ectopic pregnancy: ultrasound diagnosis in modern management. Clin Obstet Gynecol. 2012;55(2):402-409.
- Scibetta EW, Han CS. Ultrasound in early pregnancy. Obstet Gynecol Clin North Am. 2019;46(4):783-795.
Manuscript submitted September 30, 2022; accepted October 25, 2022.
Author affiliations: Benjamin Mati, MD, Ventura County Medical Center, Department of Emergency Medicine, Department of Critical Care Medicine. Richard Rutherford, MD,Ventura County Medical Center Department of Emergency Medicine. The authors have no relevant financial relationships with any commercial interests.
Read More
- Pitfalls Of Point Of Care Ultrasound (POCUS)—A Perspective
- A POCUS-Based Approach To Acute Renal Colic In The Urgent Care Center
- Point Of Care Ultrasound (POCUS) In Urgent Care
- Ruptured Ectopic Pregnancy With A Negative Urine Pregnancy Test
