Urgent message: Point-of-care ultrasound (POCUS) is well established as an imaging tool in the urgent care center. Although it is generally considered safe and easy to use, safety and hygiene considerations are frequently ignored—possibly leaving patients at risk for infection and excessive radiation exposure.
Avijit Barai MBBS, MRCS, MSc, PgCertCPU, FRNZCUC; Martin Necas, MMedSonography, AMS, RDMS, MRT, RVT; and Bruce Lambie, MBBS, FACEM
INTRODUCTION
Point-of-care ultrasound (POCUS) is well established as an imaging tool in the urgent care center. Although it is generally considered safe and easy to use, ultrasound is a potential fomite. Further, the biological effects of ultrasound energy are not completely understood (and not always inconsequential). Here, we review the safety and proper maintenance of POCUS.
BACKGROUND
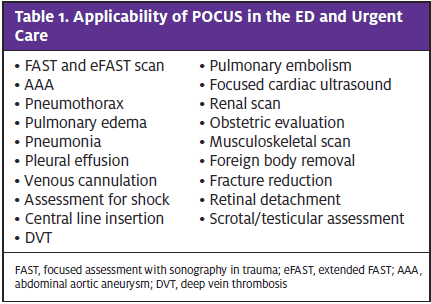
Although its use was initially limited to certain specific applications such as focused assessment with sonography in trauma (FAST), evaluation for abdominal aortic aneurysm (AAA), and pneumothorax, the spectrum of POCUS indications has expanded to include a much wider variety of other applications (Table 1). During many of these procedures, ultrasound probes may come into contact with blood and/or other potentially infectious body fluids. In addition, lack of familiarity with possible bioeffects of ultrasound and energy and utility associated with various modes of US use might not only provide poor diagnostic information but also may lead to theoretical harms from indiscriminate use of US.
MYTHS AND REALITIES
- It’s safe. The general perception is that US is categorically safe in all settings. However, the complete biological safety of US energy has not been conclusively established. Additionally, contamination of US probes can lead to transmission of organisms.1-3 Inappropriate reliance on US also can lead to harm through misdiagnosis in the hands clinicians without adequate training or understanding of its limitations.
- It’s effective. As US provides a real-time graphical representation of internal anatomic structures, clinicians tend to assume that this is always reliable. However, US is a highly operator-dependent modality and there are many sources of artifact which can lead to misinterpretation in less experienced operators.
- It’s an easy tool. Many novice clinicians assume anybody can pick up a probe and start scanning. While technically true, the quality of such scans is generally poor. Understanding the physics of US, appropriate settings for given indications, and the US findings in various disease states is actually highly complex and takes extensive practice.
BIOEFFECTS AND BIOHAZARDS
Ultrasound propagates through soft tissues as an oscillating, longitudinal, mechanical wave. During this process, much of the transmitted sound energy is converted to heat. Although the amount of such thermal bioeffects is small, prolonged exposure to such thermal bioeffects may pose a hazard and cause damage to sensitive tissues, like nerves, and developing embryonic fetal tissues.4 Thermal bioeffects are particularly increased during the application of spectral and color Doppler settings because these technologies use longer pulses resulting in greater energy transfer to the human body.
In addition, US may have non-thermal bioeffects like cavitation (stable and inertial), microstreaming, and acoustic force streaming. Of these, inertial cavitation is particularly concerning as it causes rupture of gas bubbles in soft tissue (such as the lung or gut) with intense localized effects including high pressures, free radical formation, cell membrane disruption, etc.
The magnitude and significance of these effects has been poorly characterized and remains largely theoretical. However, knowing that this can occur is important for appreciating that US is not a zero-risk technology as is commonly believed.
Specific Safety Issues
- Cross-transmission of organisms: A soiled probe is a potential source of transmission of microbesincluding Pseudomonas, methicillin resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococcus (VRE).1 A simple paper wipe fails to sterilize probes and can allow for cross-transmission of such microbes.5-7
- Blood borne organisms: It has been well documented that Hepatitis B, Hepatitis C, and HIV can be transmitted by blood, blood products, and body fluids on instruments.8,9 The risk of transmission of such blood borne pathogens should be considered if using US over an open wound.
- Pregnancy: Concerns have been raised about the risks to the fetus due to the application US imaging during pregnancy.10,11 In addition, evidence collated from laboratory studies revealed potential clinically significant effects to fetal development from the energy of US waves.12 However, multiple authors and professional bodies agree that ultrasound is safe during pregnancy provided that certain precautions are undertaken.13,14
- Ophthalmology: Ultrasound may pose a thermal risk to highly sensitive tissues of the eye.15
Safety Indices
All US machines feature a real-time display of thermal and mechanical indices for the operator to monitor. As these indices vary with system settings of the machine, it is important to ensure these remain within recommended values.
Thermal index (TI) is defined as the ratio of the current acoustic power output to the acoustic output power required to cause a temperature rise of 1°C in tissues. Because different tissues have a different capacity for heating, three types of TI have been developed: TI in soft tissue at the focus (TIS), TI in the bone at the focus (TIB) and TI at the cranial surface (TIC).
TIS is applicable in all soft tissues and during pregnancy <8 weeks gestational age. TIB is specifically applicable in pregnancies dated >8 weeks gestational age. TIC is used in neonatal brain ultrasound. It is important to remember that the TI is a ratio, not an absolute value. For instance, during early pregnancy scanning, the following information may be displayed: “TIS=0.5.” This should be interpreted as, The current power output is 0.5 times that which would cause temperature rise in soft tissues at focus of 1°C. This is not the same as saying the temperature will rise by 0.5°C.
In addition, Mechanical index (MI) provides some information about the probability of cavitation events in the tissue. The MI ranges from 0 to 1.9. Transient cavitation can occur with MI values of >0.3. Inducing transient cavitation probably confers very little clinical risk to adults. However, in neonates or pediatric patients, keeping the MI <0.4 is advisable if gaseous bodies are present within the beam path (ie, lung, gut etc.).
MAINTENANCE ISSUES
Ultrasound is not only operator-dependent but also machine-dependent. A defective machine may give improper diagnostic information. Maintenance of the machine is the clinician’s responsibility. It is important to check for worn or damaged parts and damaged transducer cables, and to verify the integrity of the transducer face and proper functioning of all the elements. Finally, an image uniformity check can be easily accomplished by applying a small amount of gel to the transducer surface and running a finger back and forth.
AWARENESS AMONG CLINICIANS
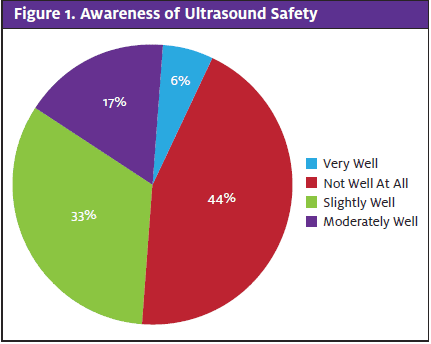
Although there are safety consideration regarding the clinical use of US, there is generally a lack of awareness of this issue among most clinicians.16,17 We recently conducted a local survey among ED clinicians which revealed that awareness of the safety and maintenance of ultrasound varies considerably from one clinician to the next. In the survey, 44% of the ED clinicians felt that they were not well aware of the issue of safety and maintenance of ultrasound (Figure 1). Multiple studies across Europe, North America, and Australasia have demonstrated that even experienced users of ultrasound knew little about the safety considerations in diagnostic US use.18
The Australasian College for Emergency Medicine (ACEM) endorses policies and guidelines on the credentialing of US in the ED.19,20 However, there is a lack of rigorous protocols for the safety and maintenance of US. There is a demand from the ACEM for such protocols on the clinical applications of US.21 Moreover, how these policies will be created and practiced remains unclear. We are currently conducting a nationwide survey in New Zealand among ED clinicians to examine the current trends in the applicability of ultrasound in the ED.
RECOMMENDATIONS
- Minimizing the risk of cross-infection by US surfaces
- Transducers which have not been in direct contact with body fluids or broken skin should be cleaned by first removing all gel with an absorbent cloth followed by wiping the transducer and cable with a low to medium level disinfectant. However, some cleaning wipes may not be suitable for all systems. Specifically, frequent use of alcohol wipes after every patient may degrade the rubber seal of the probe on some transducers.22 The system console and cables also require regular cleaning.
- Applying a sterile cover on the probe during a sterile procedure may reduce the risk of cross-infection. Remember that regular US gel is not sterile unless it is specifically labeled as such.
- The use of single disposable gel bottles is the preferred option for UC and ED use. If the gel is decanted into gel bottles from bulk containers, there must be provision for cleaning of gel bottles.
- Minimizing biological effects of US
- Prudent use: US should be used by suitably qualified health professionals to provide medical benefit to the patient.23 Alternatively, it is reasonable for the US to be used by trainees under direct supervision whereby direct correction of a technical or diagnostic error is possible.
- ALARA principle: The acoustic dose to the patient should be as low as reasonably achievable (ALARA). Common breaches of ALARA include excessive scanning times, high power output, and inappropriate use of high energy modes.
- During pregnancy: Observe the TIS in pregnancies <8 weeks and TIB in pregnancies >8 weeks. If the TI is >1.0, turn down the acoustic output power control. Routine use of Doppler ultrasound in the first trimester is not advisable.13
- In neonates and pediatric patients: If possible, minimize the probability of inertial cavitation when scanning near air-filled structures (eg, lung, bowel) by reducing the power output until MI <0.4.
- Ophthalmology: The eye may be covered with a Tegaderm, especially if there is a wound in or around the eye. Some ultrasound machines have settings for ophthalmologic use to prevent US-induced eye injury.
- Minimizing misdiagnoses
- Formal education in POCUS and established protocols for demonstrating competency should be developed to ensure prudent use of POCUS in the hands of clinicians. Those holding certifications in limited areas (eg, FAST, eFAST) should resist the compulsion to expand their practices into other areas without formal training and oversight.
REFERENCES
- Fowler C and McCracken D. US probes: risk of cross infection and ways to reduce it- comparison of cleaning methods. Radiology. 1999; 213(1): 299-300.
- US Food and Drug Administration. FDA Safety Communication: update on bacteria found in other-sonic generic ultrasound transmission gel poses risk of infection. 2013. Available at: http://dhhs.ne.gov/han%20Documents/Advisory042012.pdf. Accessed February 5, 2021.
- Young J. Burkholderia cepacia Outbreak in NICU. Infec Cont. 2011. Available at: http://www.infectioncontrol.co.nz/uploaded/file/downloads/Jude%20Young%20%20Burkholderia%20cepacia%20Outbreak%20Waikato%20Hosp.pdf. Accessed February 5, 2021.
- Abramowicz JS. Ultrasound in obstetrics and gynecology: is this hot technology too hot? J Ultrasound Med. 2002;21:1327-1333.
- Muradali D, Gold WL, Phillips A, Wilson S. Can ultrasound probes and coupling gel be a source of nosocomial infection in patients undergoing sonography? An in vivo and in-vitro study. AJR. 1995;164:1521-1524.
- Spencer P, Spencer RC. Ultrasound scanning of post-operative wounds: the risks of cross infection. Clin Radiol. 1988;39:245-246.
- Tesch C, Fröschle G. Sonography machines as a source of infection. AJR. 1997;168:567-568.
- Kiyosawa K, Sodeyama T, Tanaka E, et al. Hepatitis C in hospital employees with needlestick injuries. Ann Inter Med. 1991;115:367-369.
- Bronowicki JP, Venard V, Botté C et al. Patient-to-patient transmission of hepatitis C virus during colonoscopy. N Engl J Med. 1997;337:237-240.
- Barnett SB, Kossoff G, eds. Safety of diagnostic ultrasound. Progress in Obstetrics and Gynecological Sonography Series. London: Parthenon Publishing Group; 1998.
- WFUMB Symposium on Safety of Ultrasound in Medicine. Conclusions and recommendations on thermal and non-thermal mechanisms for biological effects of ultrasound. Kloster-Banz, Germany. 14–19 April 1996. World Federation for Ultrasound in Medicine and Biology. Ultrasound Med Biol. 1998;24 (Suppl 1):i–xvi, S1–S58.
- Docker MF, Duck FA, eds. The Safe Use of Diagnostic Ultrasound. London: British Institute of Radiology; 1991.
- Joy JJ, Cooke I, Love M. Review: Is ultrasound safe? Obstet & Gynaecol. 2006;8: 222-227.
- Schwarze V, Marschner C, de Figueiredo GN, et al. Single-center study: evaluating the diagnostic performance and safety of contrast-enhanced ultrasound (CEUS) in pregnant women to assess hepatic lesions. Ultraschall in der Medizin-European J Ultrasound. 2020;41:29-35.
- Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9:791-799.
- Conner S, Chia D, Lalani F, et al. Minding the gap(s): hospitalists experience aspirational, safety, and knowledge deficits that prevent them from practicing POCUS. POCUS J. 2019;14;4:27-32.
- Miller DL, Abo A, Abramowicz JS, et al. Diagnostic ultrasound safety review for point-of-care ultrasound practitioners. J Ultrasound in Medicine. 2020;39:1069-1084.
- Necas M. New Zealand sonographers do not outperform their European or American colleagues in the knowledge of ultrasound safety. Austral J Ultrasound Medicine. 2010;13:28-32.
- Policy on credentialing for focussed echocardiography in life support. Policy P61. Australas Coll Emerg Med. 2016;3:1-5.
- Guidelines on minimum criteria for ultrasound workshops. Guideline G25. Australas Coll Emerg Med. 2016;6:1-5.
- Bomann JS. The case for an ultrasound mandate. Emerg Med Australa. 2016; (Early view).
- Koibuchi H, Fujii Y, Kotani K, et al. Degradation of ultrasound probes caused by disinfection with alcohol. J Med Ultrason. 2011;38(2):97-100.
- Fowlkes JB, Holland CK. Mechanical bioeffects from diagnostic ultrasound: AIUM consensus statements. American Institute of Ultrasound in Medicine. J Ultrasound Med. 2000 Feb;19(2):69-72.
Author affiliations: Avijit Barai, MBBS, MRCS, MSc, PgCertCPU, FRNZCUC, Christchurch Hospital, Christchurch, New Zealand.University of Otago, New Zealand. Martin Necas, MMedSonography, AMS, RDMS, MRT, RVT, Waikato Hospital, Hamilton, New Zealand; University of Otago, New Zealand. Bruce Lambie, MBBS, FACEM, Dunedin Hospital, Dunedin, New Zealand; Dunedin School of Medicine, University of Otago, Dunedin, New Zealand.
View Similar Articles
- A POCUS-Based Approach To Acute Renal Colic In The Urgent Care Center
- Utility Of POCUS In Skin And Soft Tissue Infection
- Point Of Care Ultrasound (POCUS) In Urgent Care
- Point-Of-Care Ultrasound In Urgent Care: A Game Changer For The Practice—And The Practitioner
- The Time For Urgent Care Clinicians To Embrace Bedside Ultrasound Is Here

