Urgent message: Ultrasound can provide essential data in the evaluation and urgent care of abnormal uterine bleeding, by facilitating a rapid diagnosis and immediate and appropriate decisions regarding management.
Andrew Alaya, MD, MSc
Citation: Alaya A. How useful is ultrasound in abnormal uterine bleeding? J Urgent Care Med. 2023;17(7):13-18.
Key words: abnormal uterine bleeding, AUB polyp, adenomyosis, leiomyoma, uterine malignancy
ABSTRACT
Abnormal uterine bleeding (AUB) is one of the most common gynecological conditions presenting at urgent care clinics. AUB before and after menopause is caused mainly by benign conditions such as endometrial polyps, intracavitary fibroids, hormonal disturbances, or endometrial hyperplasia. Up to one-third of women experience AUB in their life. AUB occurs most commonly at menarche and perimenopause and can negatively affect aspects of a woman’s physical, emotional, sexual, and professional quality of life.
The International Federation of Gynecology and Obstetrics (FIGO) uses the acronym PALM-COEIN to stratify anatomically localizable pathology (PALM) from those not distinguishable (COEIN). The majority of the underlying pathology is benign; however, care must be taken to exclude malignancy such as endometrial or cervical cancer.
Ultrasound is the primary diagnostic imaging tool to investigate AUB and is ideal for investigating and classifying AUB with the FIGO classification. The skill and the experience of the ultrasound operator is of utmost importance for a proper and accurate evaluation. Ultrasound in urgent care medicine can facilitate rapid diagnosis and immediate and appropriate decisions regarding management—hence, reassuring patients of the findings and reducing unnecessary hospital visits and related costs.
INTRODUCTION
Abnormal uterine bleeding (AUB) is one of the most common gynecological conditions presenting at urgent care clinics. As it is, most published studies focus on the diagnosis of malignancy. However, AUB in women before and after menopause is caused mainly by benign conditions such as endometrial polyps, intracavitary fibroids, hormonal disturbances, or endometrial hyperplasia.1
AUB is defined by changes in the menstruation cycle involving the abnormal frequency, regularity, duration, and volume of flow outside of pregnancy. A “normal” menstrual cycle has a frequency of 24 to 38 days, with each period lasting 7 to 9 days and involving 5 to 80 mL of blood loss. However, up to one-third of women will experience AUB in their lifetime, most often at menarche and perimenopause.1 It can negatively affect physical, emotional, sexual, and professional aspects of the lives of women.
Terms such as oligomenorrhea, menorrhagia, and dysfunctional uterine bleeding are no longer used in favor of simple terms to describe the nature of the abnormal uterine bleeding, such as heavy menstrual bleeding, intermenstrual bleeding, and postmenopausal bleeding.
AUB can be divided into two categories: acute and chronic AUB. Acute AUB is one that causes excessive bleeding that requires immediate intervention to prevent further blood loss. It can also occur on its own or superimposed on chronic AUB. In this case irregular menstrual bleeding has occurred in the previous 6 months.2
The management of AUB varies depending on the patient’s age, chronicity, severity of bleeding, comorbidities, medications, and whether or not the patient is pregnant. To make a diagnosis of the underlying pathology and treat the patient appropriately, one has to know the menstrual cycle and history of that patient.
This article focuses on the physiology of menstruation, presents evidence-based information on the causes of AUB in women, and how ultrasound can be useful in determining the cause of the problem.
BASIC PHYSIOLOGY
The menstrual cycle and ovulation constitute a complex hormonal feedback mechanism regulated by the hypothalamus, the pituitary, and the ovary.
The first half of the menstrual cycle is known as the follicular phase. In this phase, the hypothalamus secretes gonadotropin-releasing hormone (GnRH) which stimulates the pituitary to release both luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These two hormones influence the ovary. Firstly, a dominant follicle matures and secondly it secretes estrogen. Estrogen stimulates the endometrium and the stroma to grow and proliferate causing the endometrium to thicken.
In about 36 hours, estrogen levels reach a threshold level and a surge in LH occurs, causing a rupture of the dominate follicle leading to ovulation. This is the beginning of the second half of the menstrual cycle, known as the luteal phase.
Under the influence of LH, the ruptured dominant follicle cyst rapidly evolves into the corpus luteum, which secretes progesterone. During this time, a pregnancy can occur. If no pregnancy occurs, after 14 days, the corpus luteum involutes and progesterone levels drop. When this happens, prostaglandin is released. Prostaglandin causes vasospasm of the arteries feeding the endometrium leading to enzymatic breakdown of the functionalis layer of the endometrium. This breakdown leads to blood loss and sloughing, which make up menstruation. Any derangement of the structure of the uterus, such as fibroids, polyps, adenomyosis, malignancy, and hyperplasia or derangements to the clotting pathways such as coagulopathies and iatrogenically or disruption of the hypothalamic-pituitary-ovarian axis can affect menstruation and lead to abnormal uterine bleeding.3
EPIDEMIOLOGY
The prevalence of AUB among reproductive-aged women is difficult to estimate because many women do not seek treatment for their symptoms. However, internationally this is estimated to be anywhere from 3% to 30%, with higher incidence occurring around menarche and perimenopause. Many studies are limited to heavy menstrual bleeding. When considering irregular and intermenstrual bleeding the prevalence rises to 35% or more.3
AUB is the fourth most-common reason for referral from urgent care clinics to gynecological services, resulting in a loss of more than $2,000 per patient per year due to work absence and home management cost.4
ETIOLOGY
The International Federation of Gynecology and Obstetrics (FIGO) classified the underlying etiologies of AUB in the acronym PALM-COEIN. PALM describes AUB based on structural factors, with each letter of the acronym indicating one of the etiologies of bleeding:
P: uterine polyp
A: adenomyosis
L: leiomyoma
M: precursor and malignant lesions of the uterus body
One or more etiologies from the above list can contribute to the patient’s AUB. At the same time, some of these etiologies, such as endocervical polyp, endometrial polyp, or leiomyomas, may be asymptomatic and not the primary cause of the patient’s AUB.
The second portion of the acronym, COEIN, describes AUB based on nonstructural factors. Each letter of the acronym indicates one of the following etiologies of bleeding:
C: coagulopathies
O: ovulatory dysfunction
E: endometrial dysfunction
I: iatrogenic
N: not yet classified
COEIN classifications are nonstructural factors that are not measurable or visible by ultrasound. For this reason, they are not covered in this article.
ULTRASOUND AND PALM
The underlying causes of AUB in PALM are usually benign pathologies, though these warrant investigation to exclude other, more sinister underlying pathology. Ultrasound can provide rapid, accurate diagnosis with minimum invasiveness and cause for hospital visits, which are often expensive and time-consuming.
P: Polyp
Endometrial polyps are an overgrowth of endometrial glands and stroma that protrude out of the endometrium. They can be sessile or pedunculated excrescences of endometrial tissue. They may be found as a single lesion or multiple lesions, filling the entire endometrial cavity.
Endometrial polyps may be seen in all ages. However, they are most common between 40 and 50 years of age. Their exact etiology is unknown. Polyps are associated with abnormal estrogen levels and other endometrial aromatase activity and genetic factors.
Ten percent of asymptomatic premenopausal women have been shown to have endometrial polyps, compared with 50% of premenopausal women with AUB. Premenopausal women are less likely to have a malignant endometrial polyp compared with postmenopausal women.
Malignancy in an endometrial polyp is associated with the patient’s age and menopausal status.6 The risk of malignancy in asymptomatic postmenopausal women is 1.5%; the risk increases to 4.5% in symptomatic postmenopausal women.5
Endometrial abnormalities, including the development of polyps, are associated with chronic tamoxifen therapy and occur in 20% to 35% of women.7
Although the risk of malignancy is small, polyps are often removed by hysteroscopic resection in both symptomatic and asymptomatic women. Hysteroscopic resection is not without risk. A study over a 2.5-year period showed that small endometrial polyps frequently regressed, whereas larger polyps were more likely to persist and were associated with the development of abnormal bleeding.8
On transvaginal ultrasound (TVU), polyps may have a varied appearance. They have nonspecific thickened endometrium, a focal echogenic area within the endometrium or occasionally present as a mass in the endometrial cavity surrounded by fluid. They generally have a homogeneous texture without disruption of the myometrial-endometrial interface.
Using Doppler ultrasound, it may be possible to see the pedicle that supplies blood to the polyp. The pedicle is the polyp’s feeding vessel. The use of 3D TVU can clearly visualize a polyp in the endometrium.
Polyp visualization will confirm the diagnosis, and further tests such as saline infusion sonohysterography (SIS) and hysteroscopy will not be necessary.1 Occasionally, problems may arise in distinguishing between larger polyps and submucous fibroids. As ultrasound is operator-dependent, experience is an essential element to distinguish between the two.
A: Adenomyosis
Adenomyosis is the presence of ectopic endometrial glands and stroma in the myometrium. Adenomyosis is found in women of reproductive age, most often in those having more than one child (multiparous).
Adenomyosis is thought to occur when uterine curettage, caesarean birth, termination of pregnancy, and multiple parity occur, due to a disruption of the endomyometrial junction allowing infolding of the endometrium with myometrial invasion.9
Adenomyosis usually affects the inner third of the endometrium and rarely affects the cervix.
Adenomyosis is also associated with exposure of estrogen and tamoxifen with increasing age.9
At cellular level, adenomyosis may occur due to damage of the endomyometrial junction caused by matrix metalloproteinases, cyclo-oxygenase enzymes, vascular endothelial growth factor, and stem cell progenitors. The use of biomarkers has been explored in research settings for diagnosis of adenomyosis; however, no biomarkers have yet been adapted for clinical use.10
It is still unclear how adenomyosis is related to AUB. Adenomyosis may be both focal or diffuse and may coexist with fibroids, which can make it challenging to ascertain a differential diagnosis. Histological confirmation of adenomyosis may differ from 5% to 70%.7
The modality of choice for the diagnosis of adenomyosis is TVU. On TVU, adenomyosis may appear nodular with circumscribed aggregates or diffuse with foci scattered throughout the myometrium with hypoechoeic areas, heterogeneous myometrial echotexture, asymmetric uterine enlargement and subendometrial cysts .
3DTVU may improve the sensitivity when the junctional zone is poorly defined. Ultrasound is dependent on the skill of the operator and the presentation of the patient’s anatomy, which play a very important role in diagnosis. MRI is also useful in diagnosis of adenomyosis and has slightly higher accuracy than TVU.11
L: Leiomyoma
Leiomyoma, also known as fibroids or myoma, represent the most common tumor in women. By the age of 50, almost 70% of White women and more than 80% of Black women will have developed at least one fibroid. Most women have no symptoms. Others may have discomfort and pressure symptoms, typically urinary.
With large fibroids, compression of the renal tract and pelvic vasculature may occur leading to renal function impairment and venous thromboembolism. Fibroids are associated with subfertility, miscarriage, preterm labor, and obstruction of labor.12
Many women who present to urgent care with AUB are associated with iron-deficiency anemia. Thirty percent of patients with leiomyoma will require treatment because of the presence of symptoms, including AUB.13 Treatment can be use of medication or a surgical approach. Surgical treatment should be considered when clinical treatment does not help.14
The path and type of treatment approach depend on the number, location, and size of the leiomyoma and the desire for conception. For those women whose everyday life is disrupted by the symptoms caused by leiomyomas, hysterectomy remains a leading indicator for treatment. For others, newer medical options may offer genuine effective relief for both AUB and other symptoms associated with leiomyoma.15 In the U.S., it is estimated that the annual direct treatment costs and indirect costs from lost working hours as a result of leiomyomas is $4.1 to $9.4 billion and $1.55 to $17.2 billion, respectively.16
The mechanisms of AUB and leiomyomas are not completely understood. The prevalence of leiomyomas is high in women with AUB, while other women may have entirely normal bleeding patterns. It is theorized that leiomyoma increases the endometrial surface area, leading it to become fragile, and the engorged vasculature in the perimyoma area results in increased flow along these enlarged vessels which may overcome platelet action.17 Other studies have sought to associate leiomyomas and the complex cellular and molecular changes in angiogenesis, alteration in vascoactive substrates, and growth factors, as well as alteration on coagulation.18 Currently, it is believed that leiomyomas have a field change within the uterine cavity rather than limited to regions overlying the leiomyoma(s) which may have an impact on endometrial receptivity, implantation and AUB.19
Due to their smooth muscle and varying degree of connective tissue, leiomyomas appear on ultrasound as a well-defined, heterogeneous, or hypoechoeic mass . The mass may have cystic areas if the leiomyoma is degenerating. In postmenopausal women, leiomyomas are often seen having calcifications.
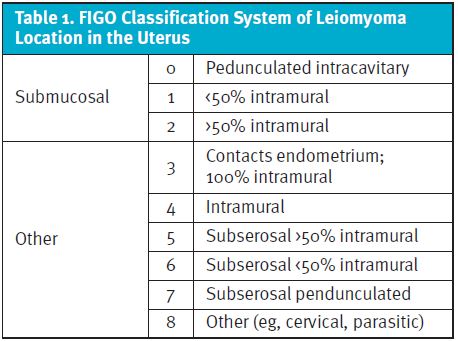
Ultrasound is the modality of choice for diagnosing fibroids and their calcifications with regards to size, number, and location. TVU has 100% sensitivity and 94% specificity in the diagnosis of leiomyomas.12 FIGO has developed a subclassification of leiomyomas according to their size, number, and location in the uterus (Table 1).
It may be difficult to differentiate between endometrial polyps and submucosal leiomyomas. This can be avoided by performing the ultrasound examination in the proliferative phase rather than in the secretory phase of the menstrual cycle. In cases when the leiomyomas are large, a transabdominal ultrasound examination should be performed to ascertain the exact size and location of the mass.
M: Malignancy
One of the most common gynecological malignancies in the Western world is endometrial cancer. Historically, endometrial cancer has rarely occurred in premenopausal women. However, increase in obesity and metabolic syndrome led to a marked increase in an endocrine-driven subset of endometrial malignancy. More than 90% of uterine cancers occur in the endometrium.20
Endometrial cancer is the fourth most common cancer in women in the U.S. In 2021, an estimated 66,570 women were diagnosed with uterine endometrial cancer, causing 12,940 deaths in the U.S.21 Ninety percent of women with endometrial cancer have AUB. At the same time, it is good to realize that AUB is a common symptom of many benign diseases, and only 1% to 2% of premenopausal women and 9% of postmenopausal women have indicated the presence of endometrial cancer.22,23
About 5% of women seeking help in primary care medicine have postmenopausal bleeding (PMB). The majority of these women have benign findings, and the cause is usually genital tract atrophy. However, 9% will have primary or secondary malignancy. Eighty percent of these women will have endometrial cancer. The risk of having endometrial cancer with PMB increases with age. At the age of 50 it is 1%; by age 80 it increases to 25%.24
TVU is the first modality of choice to investigate women with PMB. A cutoff of 8 mm or above for endometrial thickness is considered to be abnormal, with further tests such as hysteroscopy and endometrial biopsy required to rule out endometrium cancer. ndometrium thickness of <2 is associated with endometrial atrophy.25 Ten percent of the pretest women with PMB will have their probability reduced to 1% following normal TVU. Fluid in the endometrium cavity is consider of no significance.24
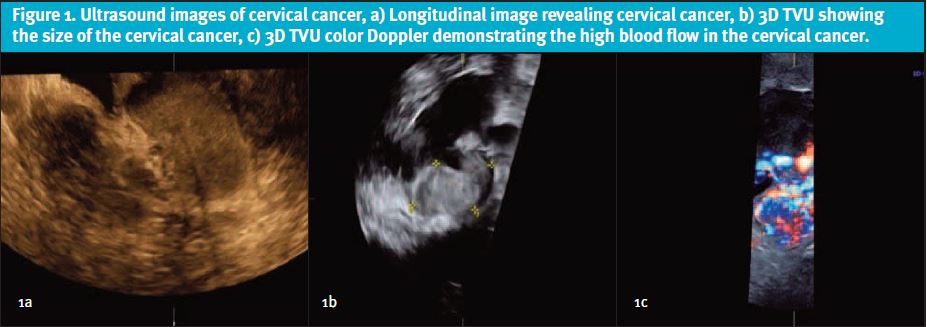
Cervical cancer may be considered when there is persistent intermenstrual bleeding. This is especially important for women who do not undergo screening of Papanicolaou (PAP) test or human papillomavirus (HPV) test.
The second most frequent gynecological malignancy worldwide is cervical cancer.26 Effective ultrasound depends on the experience of well-trained operators for accurate diagnosis. Ultrasound may provide highly accurate information on detecting tumour presence and evaluation of local tumour extent.27 This can be done by TVU (see Figure 4a). Using 3D TVU, one can measure the volume of a tumour quite accurately28 (see Figure 4b). 3D TVU colour Doppler may be used to demonstrate the high vascularization of the cervix tumour (see Figure 4c).
Another cause of AUB may be uterine sarcoma. Ultrasound is not the ideal modality for the diagnosis of uterine sarcoma. Although it is said that uterine sarcomas are rare, one woman per 340 in the U.S. is reported to have leiomyosarcoma unexpectedly diagnosed following surgery for anticipated “benign” leiomyomas.29
Age is associated with increased risk of developing leiomyosarcoma. In women under the age of 30 years, risk is estimated to be less than one in 500, compared with one in 98 among women in the age range of 75-79 years.29
Other risk factors for uterine leiomyosarcoma include the long-term use of tamoxifen, previous pelvic radiation therapy, and rare inherited disorders such as hereditary leiomyomatosis and renal cell carcinoma (HLRCC).30 Contrary to the belief that a rapidly enlarged uterus would raise suspicion of malignancy, this is no longer held to be true. Benign fibroids may grow rapidly, and sarcomas grow slowly.31
CONCLUSION
AUB is one of the common presentations among women visiting urgent care. Most of the underlying pathology is benign, but care must be taken to exclude malignancy such as endometrial or cervical cancer. Ultrasound (TA, TV, DTV and 3DTV) is the primary diagnostic tool to investigate AUB and is ideal for investigating the FIGO classification of AUB, the PALM-COEIN. Skills and experience of the ultrasound operator are of utmost importance. Ultrasound in urgent care medicine can facilitate rapid diagnosis and management, hence, reassuring the patients of the findings and reducing unnecessary hospital visits and costs. By determining or eliminating the cause the of AUB, the patient can be adequately counseled and referral to the appropriate specialist.
REFERENCES
- Timmermans A, Opmeer BC, Khan KS, et al. Endometrial thickness measurement for detecting endometrial cancer in women with postmenopausal bleeding: a systematic review and meta-analysis. Obstet Gynecol. 2010;116(1):160-167.
- ACOG committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol. 2013;121(4):891-896.
- Munro MG, Critchley HOD, Fraser IS, Committee FMD. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet. 2018;143(3):393-408.
- Frick KD, Clark MA, Steinwachs DM, et al. Financial and quality-of-life burden of dysfunctional uterine bleeding among women agreeing to obtain surgical treatment. Womens Health Issues. 2009;19(1):70-78.
- Lee SC, Kaunitz AM, Sanchez-Ramos L, Rhatigan RM. The oncogenic potential of endometrial polyps: a systematic review and meta-analysis. Obstet Gynecol. 2010;116(5):1197-1205.
- Karakaya BK, Ozkan NT, Kansu-Celik H, et al. Malignancy risk of endometrial polyps among geriatric women. Int J Gerontol 2018; 12(3): 215–217.
- Emons G, Mustea A, Tempfer C. Tamoxifen and endometrial cancer: A Janus-Headed Drug. Cancers (Basel). 2020;12(9):2535
- DeWaay DJ, Syrop CH, Nygaard IE, et al. Natural history of uterine polyps and leiomyomata. Obstet Gynecol. 2002;100(1):3-7.
- Abbott JA. Adenomyosis and abnormal uterine bleeding (AUB-A)-pathogenesis, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. 2017;40:68-81.
- Chodankar R, Critchley HOD. Biomarkers in abnormal uterine bleeding. Biol Reprod. 2019;101(6):1155.
- Andres MP, Borrelli GM, Ribeiro J, et al. Transvaginal ultrasound for the diagnosis of adenomyosis: systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25(2):257-264.
- Baird DD, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1):100-107.
- Dolmans MM, Cacciottola L, Donnez J. Conservative management of uterine fibroid-related heavy menstrual bleeding and infertility: time for a deeper mechanistic understanding and an individualized approach. J Clin Med. 2021;10(19):4389.
- Donnez J, Dolmans MM. Hormone therapy for intramural myoma-related infertility from ulipristal acetate to GnRH antagonist: a review. Reprod Biomed. Online. 2020;41:431–442.
- Merrill RM. Hysterectomy surveillance in the United States, 1997 through 2005. Med Sci Monit. 2008;14(1):CR24-31.
- Cardozo ER, Clark AD, Banks NK, et al. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol. 2012;206(3):211.e1-9.
- Munro MG. Classification of menstrual bleeding disorders. Rev Endocr Metab Disord. 2012;13(4):225-234.
- Stewart EA, Nowak RA. Leiomyoma-related bleeding: a classic hypothesis updated for the molecular era. Hum Reprod Update. 1996;2(4):295-306.
- Doherty L, Mutlu L, Sinclair D, Taylor H. Uterine fibroids: clinical manifestations and contemporary management. Reprod Sci. 2014;21(9):1067-1092.
- Reeves GK, Pirie K, Beral V, et al. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ. 2007;335(7630):1134.
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33.
- Clarke MA, Long BJ, Del Mar Morillo A, et al. Association of endometrial cancer risk with postmenopausal bleeding in women: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(9):1210-1222.
- Pennant ME, Mehta R, Moody P, et al. Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG. 2017;124(3):404-411.
- Van Hanegem N, Breijer MC, Khan KS, et al. Diagnostic evaluation of the endometrium in postmenopausal bleeding: an evidence-based approach. Maturitaa. 2011; 68:155.
- Ozdemir S, Celik C, Gezginç K, et al. Evaluation of endometrial thickness with transvaginal ultrasonography and histopathology in premenopausal women with abnormal vaginal bleeding. Arch Gynecol Obstet. 2010;282(4):395-399.
- WHO. WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention. Second editon ed. Geneva: World Health Organization; 2020.
- Haldorsen IS, Lura N, Blaakær J, et al. What is the role of imaging at primary diagnostic work-up in uterine cervical cancer? Curr Oncol Rep. 2019;21(9):77.
- Chou CY, Hsu KF, Wang ST, et al. Accuracy of three-dimensional ultrasonography in volume estimation of cervical carcinoma. Gynecol Oncol. 1997;66(1):89-93.
- Lumsden MA, Hamoodi I, Gupta J, Hickey M. Fibroids: diagnosis and management. BMJ. 2015;351:h4887.
- Giuntoli RL, Metzinger DS, DiMarco CS, et al. Retrospective review of 208 patients with leiomyosarcoma of the uterus: prognostic indicators, surgical management, and adjuvant therapy. Gynecol Oncol. 2003;89(3):460-469.
- Peddada SD, Laughlin SK, Miner K, , et al. Growth of uterine leiomyomata among premenopausal black and white women. Proc Natl Acad Sci U S A. 2008;105(50):19887-19892.
Manuscript submitted April 16, 2022; accepted August 17, 2022.
Author affiliations: Andrew Alaya, MD, MSc, Bronovo Hospital, The Hague, Netherlands. The author has no relevant financial relationships with any commercial interests.

