Andrew Alaya, MD, MSc
Urgent Message: For time-sensitive diagnoses related to acute pelvic pain, ultrasound is generally the recommended initial diagnostic imaging study. While not universally available in urgent care, it can often be completed more rapidly than computed tomography or magnet resonance imaging.
Citation: Alaya A. How Useful Is Ultrasound In Acute Female Pelvic Pain? J Urgent Care Med. 2024;18(7):35-40
Introduction
Acute pain in the pelvic or lower abdominal region among women of reproductive age who are not pregnant is a common reason for seeking care at urgent care (UC) centers and emergency departments (ED). In 2018, there were over 500,000 obstetrics/gynecology (OB/GYN) ED visits by adolescents in the United States.[1] For the purposes of this review, the term “acute pelvic pain” refers to a sudden onset of severe pain of the lower abdomen.[2]
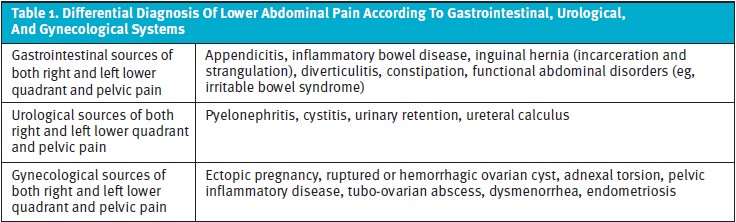
When a woman of reproductive age presents to a UC center for sudden pelvic or lower abdominal pain, it is crucial to rule out conditions that might be associated with significant morbidity, loss of fertility, and/or potential mortality without rapid medical or surgical intervention.1 Such interventions will necessitate rapid OB/GYN consultation, or if unavailable, referral to an appropriate ED. Given the diversity of etiologies for acute pelvic pain—which may be related to pathology of the gastrointestinal, gynecological, urological, or vascular system—ultrasound (US) is often a highly effective and economical initial imaging modality for risk stratifying such presentations.
Gynecological emergencies represent a significant proportion of cases involving acute pelvic pain.[3] The underlying pathological conditions leading to the onset of pain are rather diverse,[4] and they can be categorized based on age group, pregnancy status, and organ of origin.[5]
For females of reproductive age, it is crucial to exclude pregnancy with human chorionic gonadotropin (βhCG) testing. A qualitative urine hCG is highly accurate at excluding pregnancy and rarely results in false negative results.[6] Correctly diagnosing the cause of pelvic pain requires a comprehensive assessment, taking into account the patient’s past medical history, presenting history, physical exam, and investigative findings. Specific historical features that are important to assess include:
- The onset, location, quality, radiation, duration, aggravating and alleviating factors, and any temporal changes of the pain over time
- Associated symptoms, such as vomiting, diarrhea, fever, flank pain, dysuria, hematuria, frequency, urgency, vaginal bleeding, and vaginal discharge
- Relevant related medical history, such as last menstrual period, regularity and duration of menses, age of menarche, sexual history, history of sexually transmitted infections, and a complete obstetric history
The physical examination should concentrate on accurate and complete vital signs, abdominal exam, and genitourinary exam, including a bimanual and speculum exam.
Depending on the history and physical exam, the etiology of the pain can be categorized as likely gastrointestinal, urological, or gynecological in origin. US then can be used subsequently to further refine the differential diagnosis presented in Table 1.
Laboratory investigations that may be considered include:
- Complete blood count that may reveal anemia or thrombocytopenia to suggest degree and cause of hemorrhage or leukocytosis, which is non-specific but may suggest an inflammatory condition
- Urinalysis that may reveal hematuria and/or pyuria
- Urine pregnancy test
- Vaginal wet mount or pathogen assay to assess for trichomonas, bacterial vaginosis, or Candida.
- Endocervical or vaginal polymerase chain reaction swabs for chlamydia (CT) and gonorrhea (GC)
Acute pelvic pain can represent a wide spectrum of conditions, ranging from a benign and self-limited disease to surgical emergencies. This remainder of this article focuses on acute gynecological sources of pelvic pain and how US offers excellent additional diagnostic information in differentiating many of the gynecological issues that can cause acute pelvic pain including:
- Adnexal torsion
- Ectopic pregnancy
- Pelvic inflammatory disease
- Ovarian cysts
- Adhesions
- Endometriosis
Adnexal Torsion
Adnexal torsion, a condition where the ovary and fallopian tube twists around its vascular axis, can result in ovarian ischemia and necrosis. It occurs most commonly in women of reproductive age (70%), though it can occur in any age from prepuberty to postmenopause.[7] Torsion can be intermittent and resolve spontaneously in certain cases, however, identification necessitates prompt diagnosis and emergency surgical intervention to preserve the ovary and prevent infertility.
Adnexal torsion is ranked as the 5th most common gynecologic emergency.[8] Diagnosing ovarian torsion can be challenging due to the diverse underlying causes of lower abdominal pain in females. Clinical manifestations, such as acute pelvic pain that can be constant or intermittent due to twisting and untwisting of the adnexa, occurs in 94-100% of cases. Due to the intense pain, vomiting is common and occurs in 70% of cases. As the clinical presentation is variable and overlaps with many other conditions, misdiagnosis is common, and delays in diagnosis increase the risk of unsalvageable ovary.[9]
US is useful for differentiating ovarian torsion from other pelvic pain conditions. βhCG should be performed in women of childbearing age to exclude ectopic pregnancy as a possible cause of sudden pelvic pain. A ruptured ovarian cyst is a common condition that may mimic ovarian torsion as it also causes the sudden onset of sharp pain. Cyst rupture commonly occurs during physical activity or sexual intercourse, but this history is not universal for this diagnosis. On the other hand, a gradual onset of pelvic pain (especially if accompanied by fever) likely indicates an alternate diagnosis, such as tubo-ovarian abscess (TOA), pelvic inflammatory disease (PID), appendicitis, or diverticulitis.[10]
There are no laboratory test that can confirm or exclude ovarian torsion. However, leukocytosis from the acute stress reaction is not an uncommon finding.10
One of the main risk factors for ovarian torsion is a previous history of adnexal torsion. Between 11-19% of patients with torsion have had a previous adnexal torsion event.10 Another important risk factor is the presence of ovarian cysts or other causes of ovarian enlargement, as torsion occurs much more commonly with adnexal enlargement. The right ovary is more commonly affected than the left, likely due to more potential space owing to the location of the sigmoid colon.10 While ovarian masses increase the risk of torsion, particularly those larger than 5cm, the risk of torsion seems to be mitigated by endometriosis and malignant lesions possibly due to the presence of adhesions from chronic inflammation.[11]
US with Doppler is generally the preferred initial imaging modality for diagnosing ovarian torsion. Accuracy is highest if both transabdominal and transvaginal views are obtained. While US is recommended as the initial imaging study for suspected torsion, it is a more specific than sensitive modality. US findings of torsion, when present, are highly valuable and rule in the diagnosis with up to 100% positive predictive value.[12] It is important to note that US has a sensitivity of only 84%, which is influenced by various factors, including the operator’s skills and the patient’s anatomy.[13] Therefore, in cases of high clinical suspicion, it is important to not rely on a negative or non-diagnostic US to exclude torsion.
US is particularly sensitive in detecting ovarian edema. In some cases, free fluid may be visible, or the characteristic “whirlpool sign,” which is highly specific, can be demonstrated due to the twisting of the vascular pedicle in cross-section.13 Computed tomography (CT) is an alternative imaging modality and may be slightly more sensitive than US,[14] but US remains the preferred choice due to its widespread accessibility, lack of ionizing radiation, and cost-effectiveness worldwide.8
According to Spinelli et al., when assessing females suspected of adnexal torsion, it is essential to recognize that no clinical or imaging criteria alone are adequate for excluding the diagnosis of adnexal torsion. In cases where there is a clinical suspicion of adnexal torsion, it is recommended that patients receive emergent gynecological consultation for diagnostic laparoscopy.[15]
Although diagnostic laparoscopy is generally recommended when there is strong clinical suspicion (even if US findings do not confirm ovarian torsion), only 44% of diagnostic surgical approaches actually confirm the presence of ovarian torsion. One study found that the time between the initial physical examination and surgery can vary widely, ranging from 0 to 90 days, with a median time of 101 hours.9
The definitive diagnosis of ovarian torsion is achieved through direct visualization of the rotated ovary during surgery. In patients of reproductive age, this allows for the untwisting of the ovary while preserving its function. Even though fertility is not a concern in postmenopausal patients with torsion, unilateral salpingo-oophorectomy is often justified due to the higher risk of malignancy and to prevent recurrence.[16]
Ectopic Pregnancy
Ectopic pregnancy (EP), or extrauterine pregnancy, refers to the implantation of a blastocyst outside the uterine cavity. Approximately 95% of EPs occur in the fallopian tube.[17] Other less frequent implantation sites include the ovaries (3.2%) and the abdominal cavity (1.3%).17 EP represents a major cause of morbidity and death in women worldwide due to the associated risk of tubal rupture and intra-abdominal hemorrhage. It can also adversely affect future fertility.17 As a result, EP requires rapid diagnosis and, in the cases of rupture, surgical intervention.17 In patients with a positive βhCG test, a transvaginal US is recommended for patients with either pelvic discomfort or vaginal bleeding,17 though patients do not always present with both.
EP is a common reason for women with pelvic pain to seek emergency care, and it comprises about 2% of all pregnancies. The risk can be increased in patients with sexually transmitted infection, such as CT or GC, and also by congenital abnormalities, endometriosis, or history of previous surgery.11 The incidence can be as high as 4% among women using assisted reproductive technology (ART), and in total, EP is responsible for about 10% of deaths during the first trimester of pregnancy.[18] Generally, EP can be considered ruled out with a negative urine βhCG. In patients with negative βhCG with significant pelvic pain who also undergo transvaginal US and have no evidence of intra- or extrauterine gravidities present, EP can generally be safely excluded, despite the relatively rare possibility of a false negative urine βhCG test.[19] More importantly, US can rule out ectopic when an intrauterine pregnancy is identified, unless the patient is at high risk for heterotopic pregnancy (ie, receiving fertility treatments). Heterotopic pregnancy—the rare occurrence of an EP co-occurring with an intrauterine pregnancy (IUP)—is an entity that should be considered in women at elevated risk (ie, those undergoing ART) and with presentation concerning for EP.
Outside of a hospital setting, quantitative serum βhCG is not generally immediately available, and qualitative urine tests are usually performed. Nevertheless, the latter is often used in a hospital setting as well. A standard urine test can detect hCG as low as 20 IU/L.6 A negative urine test is generally considered to rule out pregnancy. Unfortunately, this is not always the case as patients with very early or abnormal pregnancies can have serum hCG concentrations under 20 IU/L.6 A 2021 retrospective ED study found that urine pregnancy tests had a 1.6% false negative rate, and 7% of early missed pregnancies were ectopic.[20]
US is the first modality of choice when considering the possibility of EP. Abdominal US is useful, but transvaginal US performs better in confirming an intra- or extrauterine gestation with a sensitivity of 93% and specificity of 97%.[21] Together with US, βhCG, is a valuable tool for assessing pregnancy. A combination of US and βhCG has 95% sensitivity and specificity for EP.18 A practical approach for many UC settings is to use US to “rule in” intrauterine pregnancy. If a urine βhCG is positive, but no IUP is identified on US, immediate referral to an ED is appropriate for further assessment for a possible EP.
Pelvic Inflammatory Disease
Pelvic inflammatory disease is caused by infection of the upper genital tract, primarily due to GC or CT, though other aerobic and anaerobic organisms may also be involved.[22] Common symptoms of PID include fever and purulent vaginal discharge. Diagnosis can be challenging, especially in resource limited settings such as urgent care centers. According to the Centers for Disease Control and Prevention, the diagnosis of PID is based on imprecise clinical findings.[23] Early treatment with antibiotics effective against these causative agents, as well as anaerobic organisms, is crucial to minimize the risk of long-term complications, such as chronic pelvic pain, infertility, intra-abdominal infection, and an increased risk of ectopic pregnancy. PID can be acute, chronic, or subclinical and is often misdiagnosed at the index visit.[24]
Diagnosis is primarily based on clinical suspicion, and therefore, it’s essential to consider PID in sexually active women who experience unexplained lower abdominal or pelvic pain and who exhibit tenderness and/or purulent cervical discharge during pelvic examination.[25] US has a limited role in the diagnosis of PID as it is predominantly a clinical diagnosis. Tubo-ovarian abscess can occasionally be identified on transvaginal ultrasound, however, the sensitivity of US for TOA is only ~50%. Therefore, if TOA is suspected, cross-sectional imaging with CT or magnetic resonance imaging (MRI) is preferred.[26] Since these cases tend to be more ill-appearing and advanced imaging modalities are rarely available in UC, ED referral for such cases is appropriate.
Mild to moderate PID cases can be treated on an outpatient basis with a single intramuscular injection of ceftriaxone, followed by a 14-day course of oral doxycycline. Additionally, metronidazole is recommended for 14 days if bacterial vaginosis, trichomoniasis, or recent uterine instrumentation has occurred. Hospitalization and parenteral antibiotics are advised for pregnant patients, those with severe or febrile illness, cases where outpatient treatment fails, individuals with suspected or confirmed TOA, or when surgical emergencies cannot be excluded. These treatment recommendations are the same for patients with intrauterine devices or those with HIV.25 While there has been a general decline in PID rates, the increase in cases of GC and CT, along with increasing resistance rates GC are concerning trends.25
Ovarian Cysts
During women’s reproductive years, various types of benign adnexal masses, including physiologic cysts, can present with acute pelvic discomfort.[27] Functional or physiologic cysts such as follicular cysts, corpus luteum cysts, and theca lutein cysts are common examples. Large follicular cysts may cause pelvic discomfort and dyspareunia, but most resolve spontaneously without complication.[28]
After regular ovulation, blood can accumulate in the central follicular cavity, leading to the development of a corpus luteum cyst, which can cause pain or discomfort if it persists.[29] Theca lutein cysts, associated with elevated hCG levels, may arise due to conditions like molar pregnancy, choriocarcinoma, or clomiphene therapy, but they typically resolve with appropriate management of the underlying condition (or clomiphene is discontinued, in such cases).[30]
In premenopausal females, ovarian cysts are frequently found, and they typically do not cause intense pain unless there is hemorrhage or rupture. Pelvic ultrasonography can easily identify serous follicular cysts, which have a thin-walled appearance and a diameter of >3 cm. Corpus luteum cysts exhibit a thick irregular wall on US.[31]
During the menstrual cycle’s luteal phase, increased ovarian vascularity can raise the risk of hemorrhage or rupture.[32] Hemorrhagic cysts may show diverse ultrasonographic appearances depending on the stage of blood product evolution. They typically exhibit lace-like internal echoes with peripheral vascularization on color Doppler US, lack internal signals, and may contain fluid-fluid levels.23
Some females may experience varying levels of pelvic pain during ovulation, known as “mittelschmerz.”[33] This type of pain is considered normal and typically resolves spontaneously within a few hours. It manifests as unilateral discomfort or pain in the lower abdomen and may be accompanied by a small amount of free pelvic fluid. Medical attention is generally not required for this condition. In cases where ovarian cysts are suspected to have ruptured (ie, severe, abrupt onset pelvic pain), free fluid in the pelvis may be identified without evidence of cysts. These cases generally are self-limited, but rarely can be associated with large hemoperitoneum and hemorrhagic shock requiring transfusion and emergent operative intervention.[34]
Adhesions
Asherman’s syndrome, also known as intrauterine adhesion (IUA), presents a diverse array of subacute-chronic signs and symptoms, including discomfort and menstrual irregularities, resulting from the presence of intrauterine adhesions. Even in cases where symptoms arise without pregnancy-related adhesions, IUA should be considered.[35] For gynecologists, it is important to differentiate between iatrogenic IUA as a consequence of procedures such as endometrial ablation and primary cases.[36]
IUA is a complex condition with profound effects on reproductive function, leading to menstrual disturbances (amenorrhea), infertility, and recurrent pregnancy loss. Therefore, patients with more indolent pelvic pain can generally await gynecologic specialist decisions about imaging to confirm this diagnosis. US may play a role and show suggestive findings but has a less established role in the diagnosis of IUA.[37] Advanced intrauterine surgeries using modern technology further increases the risk of IUA.[38]
Endometriosis
Endometriosis is a frequently encountered condition characterized by the occurrence of functional endometrial glands and stroma beyond the confines of the uterus.[39] This chronic condition often follows a cyclical pattern that corresponds to the secretory phase of the menstrual cycle. Both US and MRI techniques serve as valuable diagnostic instruments for visualizing ovarian endometriomas. US can identify distinct unilocular cystic formations with a “ground glass” appearance and an absence of vascular patterns, while MRI has a better sensitivity in revealing the deep-seated pelvic variant.32
This condition is estrogen-dependent and is predominantly identified in women during their reproductive years. It stands as one of the most prevalent non-cancerous gynecological disorders. Although the precise prevalence of endometriosis remains unknown, estimates span from 2 to 10% within the overall female population and potentially up to 50% in women dealing with subfertility or persistent pelvic discomfort.[40] The clinical manifestation of this condition can be highly variable. Diagnosis is confirmed through findings from physical examinations and imaging, and ultimately can be confirmed via histological analysis of either biopsied tissue from visibly affected areas or samples collected during laparoscopy.[41]
Given the chronic, recurrent nature of this condition, many patients will not seek care in UC for this pelvic pain, but presence of endometriosis does not exclude the possibility of other, acute gynecologic pathology. Therefore, if there is acute pain outside of the patient’s typical pattern of pelvic pain, US can serve as a useful initial imaging modality to complement a history and physical to determine if other more emergent diagnoses may also be present.
Conclusion
Pelvic pain comes in various forms—acute, chronic, or recurring—and it can also commonly be functional in nature. As with any undifferentiated complaint, UC evaluation begins with an appropriate history and exam. For time sensitive diagnoses, including ectopic pregnancy, ovarian torsion, and tubo-ovarian abscess, immediate US is generally the recommended initial diagnostic imaging study. While not universally available in UC, it can often be completed more rapidly than CT or MRI and has the advantage of usually less expense and no ionizing radiation exposure, while providing valuable data to integrate into the overall diagnostic assessment of pelvic pain in women. Manuscript submitted August 6, 2023; accepted February 20, 2024
- [1]. Hartwick Das KJ, Hood C, Rutenberg A, Lobo VG. Pediatric and Adolescent Obstetric and Gynecologic Encounters in US Emergency Departments: A Cross-Sectional Study. Ann Emerg Med. 2023 Apr;81(4):396-401.
- [2]. Scaglione M. Emergency Radiology of the Abdomen. 1. Springer Heidelberg. New York: Dordrecht London; 2012. Imaging Features and Differential Diagnosis for a Timely Management Approach; pp. 133–164.
- [3]. Niska R, Bhuiya F, Xu J. National Hospital ambulatory medical care survey: 2007 emergency department summary. Natl Health Stat Report. 2010; 26: 1–31.
- [4]. Hecht S, Meissnitzer M, Forstner R. Pelvic pain in women-gynecological causes. Radiologe 2019; 59: 126–32.
- [5]. Bhavsar AK, Gelner EJ, Shorma T. Common questions about the evaluation of acute pelvic pain. Am Fam Physician. 2016; 93: 41–8.
- [6]. Alaya A, Pelikan, H. How useful is ultrasound in diagnosing EUGs? Case report. J Urgent Care Med. 2022 Jan;16(4):23-27.
- [7]. Huchon C,, Fauconnier A. Adnexal torsion: a literature review. Eur J Obstet Gynecol Reprod Biol. 2010;150:8.
- [8]. Ashwal E, Hiersch L, Krissi H, Eitan R, Less S, Wiznitzer A, et al. Characteristics and management of ovarian torsion in premenarchal compared with postmenarchal patients. Obstet Gynecol. 2015;126:514–20.
- [9]. Patil AR, Nandikoor S, Rao A, et al. Multimodality imaging in adnexal torsion. J Med Imaging Radiat Oncol. 2015;59:7.
- [10]. Asfour V, Varma R, Menon P. Clinical risk factors for ovarian torsion. J Obstet Gynaecol. 2015;35(7):721-5.
- [11]. Marion LL, Meeks GR. Ectopic pregnancy: History, incidence, epidemiology, and risk factors. Clin Obstet Gynecol. 2012;55(2):376-86.
- [12]. Yatsenko O, Vlachou PA, Glanc P. Predictive Value of Single or Combined Ultrasound Signs in the Diagnosis of Ovarian Torsion. J Ultrasound Med. 2021;40(6):1163-1172. doi:10.1002/jum.15497
- [13]. Bardin R, Perl N, Mashiach R, Ram E, Orbach-Zinger S, Shmueli A, et al. Prediction of Adnexal Torsion by Ultrasound in Women with Acute Abdominal Pain. Ultraschall Med. 2020;41(6):688-94.
- [14]. Hwang JA, Shin HC, Kim SS, et al. Preoperative CT image-based assessment for estimating risk of ovarian torsion in women with ovarian lesions and pelvic pain. Abdom Radiol (NY). 2021;46(3):1137-1147. doi:10.1007/s00261-020-02761-7
- [15]. Spinelli C, Piscioneri J, Strambi S. Adnexal torsion in adolescents: update and review of the literature. Curr Opin Obstet Gynecol. 2015;27:320–5.
- [16]. Cohen SB, Weisz B, Seidman DS, Mashiach S, Lidor AL, Goldenberg M. Accuracy of the preoperative diagnosis in 100 emergency laparoscopies performed due to acute abdomen in nonpregnant women. J Am Assoc Gynecol Laparosc. 2001;8(1):92-4.
- [17]. Shaw JL,, Dey SK,, Critchley HO,, Horne AW. Current knowledge of the aetiology of human tubal ectopic pregnancy. Hum Reprod Update. 2010;16:432.
- [18]. Alkatout I, Honemeyer U, Strauss A, et al. Clinical diagnosis and treatment of ectopic pregnancy. Obstet Gynecol Surv. 2013;68(8):571-81.
- [19]. Lee Y, Farina G, Lhamon H. Ruptured ectopic pregnancy with a negative urine pregnancy test. J Urgent Care Med. 2007;2(2):26-28.
- [20]. Kleinschmidt S, Dugas JN, Nelson KP, Feldman JA. False negative point-of-care urine pregnancy tests in an urban academic emergency department: a retrospective cohort study. J Am Coll Emerg Physicians Open. 2021;2(3):e12427. Published 2021 May 1. doi:10.1002/emp2.12427
- [21]. Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update. 2014;20(2):250-61.
- [22]. Soper DE. Pelvic inflammatory disease. Obstet Gynecol. 2010;116:419.
- [23]. Schallert EK, Abbas PI, Mehollin-Ray AR, et al. Physiologic ovarian cysts versus other ovarian and adnexal pathologic changes in the preadolescent and adolescent population: US and surgical follow-up. Radiology. 2019; 292: 172–8.
- [24]. Trent M, Bass D, Ness RB, Haggerty C. Recurrent PID, subsequent STI, and reproductive health outcomes: findings from the PID evaluation and clinical health (PEACH) study. Sex Transm Dis. 2011;38:879.
- [25. Centers for Disease Control and Prevention website. STI Treatment Guidelines. 2021. https://www.cdc.gov/std/treatment-guidelines/default.htm. Accessed December 27, 2023
- [26]. Sofic A, Husic-Selimovic A, Katica V, et al. Magnetic Resonance Imaging (MRI) and Transvaginal Ultrasonography (TVU) at Ovarian Pain Caused by Benign Ovarian Lesions. Acta Inform Med. 2018;26(1):15-18. doi:10.5455/aim.2018.26.15-18
- [27]. Hecht S, Meissnitzer M, Forstner R. Acute pelvic pain in women-gynecological causes. Radiologe. 2019;59:126.
- [28]. Olpin JD,, Strachowski L. Imaging of acute pelvic pain: nonpregnant. Radiol Clin North Am. 2020;58:329.
- [29. Waseem S, Raad S, Farooq SM, et al. Sonographic findings in females of reproductive age with acute pelvic pain J Health Med Nurs. 2020;71:116.
- 30]. Fiaschetti V, Ricci A, Scarano AL, et al. Hemoperitoneum from corpus luteal cyst rupture: a practical approach in emergency room. Case Rep Emerg Med. 2014.
- [31]. Sayasneh A, Ekechi C, Ferrara L, et al.. The characteristic ultrasound features of specific types of ovarian pathology review. Int J Oncol. 2015; 46: 445–58.
- [32]. Jha P, Sakala M, Chamie LP, et al.. Endometriosis MRI lexicon: consensus statement from the Society of abdominal radiology endometriosis disease-focused panel. Abdom Radiol. 2020; 45: 1552–68.
- [33]. Härmä K, Vollmar P. Imaging of ovarian disease-related pain. In: Pain imaging: a clinical-radiological approach to pain diagnosis. New York: Springer International Publishing; 2019.
- [34]. Bottomley C, Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):711-724. doi:10.1016/j.bpobgyn.2009.02.001
- [35]. Liu H, Xu Y, Yi N, Yi W. Efficacy and safety of hyaluronic acid gel for the prevention of intrauterine adhesion: a meta-analysis of randomized clinical trials. Gynecol Obstet Invest. 2018;83:227.
- [36]. Deans R, Abbott J. Review of intrauterine adhesions. J Minim Invasive Gynecol. 2010;17:555.
- [37]. Dreisler E, Kjer JJ. Asherman’s syndrome: current perspectives on diagnosis and management. Int J Womens Health. 2019;11:191-198. Published 2019 Mar 20. doi:10.2147/IJWH.S165474
- [38]. Doroftei B. Dabuleanu A.M. Ilie O.D. et al. Mini-review of the new therapeutic possibilities in Asherman syndrome—Where are we after one hundred and twenty-six years? Diagnostics (Basel). 2020;10:706.
- [39]. Foti PV, Farina R, Palmucci S, et al.. Endometriosis: clinical features, MR imaging findings and pathologic correlation. Insights Imaging. 2018; 9: 149–72.
- [40]. Tssot M. L, Faller E. et al. Clinical presentation if endometriosis identified at interval laparoscopic tubal sterilization: Prospective series of 465 cases. J Gynecol Obstet Hum Reprod. 2017;46(8):647-650.
- [41]. WHO Fact Sheet. Endometriosis. 24 March, 2023. https://www.who.int/news-room/fact-sheets/detail/endometriosis. Accessed February 22, 2024.
Author Affiliation: Andrew Alaya MD MSc, HMC in The Hague, The Netherlands. The author has no relevant financial relationships with any ineligible companies.
Read More
- How Useful Is Ultrasound In Abnormal Uterine Bleeding?
- How Useful Is Ultrasound In Diagnosing Ovarian Torsion?
- The Time For Urgent Care Clinicians To Embrace Bedside Ultrasound Is Here
- Pitfalls Of Point Of Care Ultrasound (POCUS)—A Perspective
- How Useful Is Ultrasound In Diagnosing Ovarian Torsion?
- Abdominopelvic Pain, Part 1: Approach To Men In The Urgent Care Setting
- Abdominopelvic Pain, Part 2: Approach To Women In The Urgent Care Setting

