Urgent message: Ultrasound can provide essential data in the urgent care evaluation of abdominal pain, aiding in the diagnosis of intestinal abnormalities, urinary tract infection, and obstetrical and gynecological problems such as suspected ovarian torsion.
Andrew Alaya, MD, MSc
Introduction
Abdominal pain is one of the most common complaints among women of childbearing age who visit urgent centers. Urinary tract infection, diarrhea, constipation, acute viral gastroenteritis (AGE), pelvic inflammatory disease (PID), and dysmenorrhea are the most common etiologies; less common are appendicitis, incarcerated hernias, and small bowel obstruction. Other causes include corpus luteum rupture with hemorrhage, a malpositioned intrauterine device (IUD), and degenerating fibroids.1
Ovarian torsion occurs when the adnexa is partially or completely rotated around its vascular axis, which may cause an interruption in the ovarian blood and lymphatic flow. The severity of the vascular impairment depends on the number of twists and the tightness. While both the ovary and the fallopian tube are often twisted, sometimes only the ovary or the fallopian is involved. This condition causes venous congestion, edema, compression of arteries, and eventually loss of blood supply to the ovary.1
The incidence of torsion is greatest (70%) in women of reproductive age. However, it can occur from prepuberty to postmenopause. Ovarian torsion is said to be the fifth most common surgical emergency among women younger than 20 years of age, accounting for 2.7% in this population.2 Prompt diagnosis is essential, as this requires emergency surgical intervention.
If not treated, ovarian torsion may lead to congestion and ischemia which result in infertility and progressive necrosis, possibly leading to loss of the ovary. The majority of patients with ovarian torsion have delayed diagnosis.2
This case report illustrates how ultrasound can aid in improving clinical findings to diagnose ovarian torsion and reduce time to emergency surgical intervention.
CASE PRESENTATION
A 39-year-old female presented to the urgent care clinic a day after developing acute periumbilical abdominal pain, unimproved with oral analgesic medication. She was nauseated but did not vomit. Defecation and micturition were normal. PMH/PSH revealed asthma and gastric bypass, gastric band removal, C section X 4, and appendectomy. Vital signs were:
- Pulse 58
- Blood pressure 135/58
- Temperature 37.8 oC
- Respiration 15 p/min
- SpO2 100%
Physical examination revealed laparoscopic scars. There was significant lower left quadrant pain on palpation.
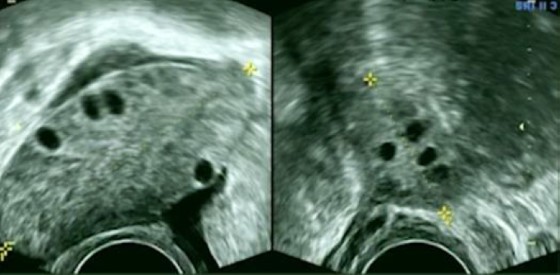
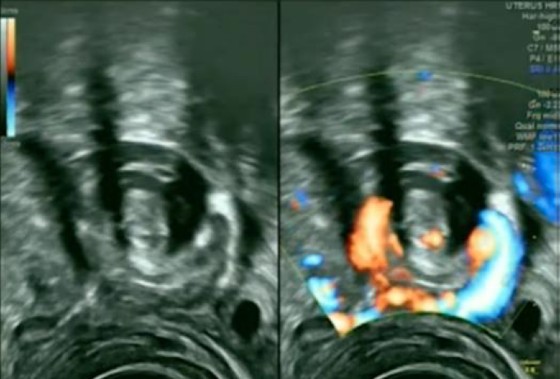
Due to diagnostic uncertainty, she was emergently referred. A CT scan with contrast of the abdomen and pelvis was normal except for some fluid in the pelvis. The left ovary measured 4.9 cm, slightly bigger than the right at 3.9 cm. Further study with a transvaginal US examination revealed an enlarged left ovary of 6.5 cm in size with stromal edema and peripheral displacement of antral follicles (Figure 1). Next to the left ovary there was a twisted fallopian tube and vascular pedicle (Figure 2), consistent with a left-sided ovarian torsion. Diagnosis was confirmed at laparoscopy.
DISCUSSION
Lower Abdominal Pain in Women
In urgent care medicine, diagnosis of ovarian torsion is made based on clinical findings and confirmed with objective testing. Most patients (94% to 100%) have acute pelvic pain, which can be constant or intermittent as the adnexa can twist and untwist. Due to vagal reflex, 70% have nausea and vomiting. Fever is seen in rare cases.2
In women of childbearing age, an ectopic pregnancy must be first ruled out with a negative beta hCG.3 Like ovarian torsion, a ruptured ovarian cyst may have free fluid in the pelvis. A gradual onset of lower pelvic pain with fever may be the cause of a tubo-ovarian abscess. Appendicitis results in a lower right-sided pain with nausea, vomiting, and fever.
Laboratory Testing
Laboratory test abnormalities are nonspecific because lab results are often normal in ovarian torsion. Abnormal lab findings may indicate leukocytosis or anemia if there is hemorrhage.4 Other causes include pyelonephritis, diverticulitis, and pelvic inflammatory disease.
Risk Factors
One of the main risk factors for ovarian torsion is previous adnexal torsion, seen in 11% to 19% of patients with ovarian torsion. The recurrency is higher in patients who have had torsion of a normal ovary than that of ovary with cyst.4 The right ovary is more commonly seen affected than the left ovary, which is thought to be due to the increased space in the right side and due to the location of the sigmoid colon on the left.4
In 46% of patients with ovarian torsion, there was an association with neoplasm; in 48% there was an association with cysts (of which 89% were benign). The risk of torsion increases when an ovarian mass is >5 cm; however, it is reduced in patients with endometriosis and malignant lesions because the mass is fixed due to adhesions and local inflammation.6 Torsion can still occur in 20% of normal ovaries, especially in the pediatric population.4 Patients undergoing fertility treatment are at high risk due to enlarged follicles on the ovaries.4
Imaging
The imaging of choice is US with color flow Doppler. Both transabdominal and transvaginal ultrasound should be performed. The sensitivity of US is 84%, but this is dependent on many factors including the skills of the operator and the patient’s anatomy.5 Free fluid may be visible, or the demonstration of the whirlpool sign due to the twisting of the vascular pedicle in cross-section.5
MRI and CT have been attempted as an alternative imaging modality; however, US remains more accessible and most cost-effective worldwide.5
The definitive diagnosis of ovarian torsion is made by direct visualization of the rotated ovary during surgery. Diagnostic laparoscopy should be performed when there is strong clinical suspicion, even with a negative US; ovarian torsion was confirmed in 44% of such patients.6 Asfour, et al found a median time of 101 hours between first physical examination and surgery.4 In patients of reproductive age, laparoscopy is always preferable, when possible, to untwist the ovary. In 88% to 100% of surgeries, laparoscopy has been reported to preserve ovarian function. In postmenopausal patients, unilateral salpingo-oophorectomy is justified due to the higher risk of malignancy and for prevention of recurrence.6
CONCLUSION
Ovarian torsion may be found in patients presenting to urgent care. Due to vague and nonspecific clinical presentation, diagnosis is challenging and there is high risk for misdiagnosis. Early suspicion is crucial to preserve ovarian and fallopian tube functions. US can aid in diagnosing ovarian torsion and shorten the time to intervention.
REFERENCES
- Melcer Y, Sarig-Meth T, Maymon R, et al. Similar but different: a comparison of adnexal torsion in pediatric, adolescent, and pregnant and reproductive-age women. J Womens Health. 2016;25(4):391-396.
- Rey-Bellet Gasser C, Gehri M, Joseph JM, Pauchard JY. Is it ovarian torsion? A systematic literature review and evaluation of prediction signs. Pediatr Emerg Care. 2016;32(4):256-261.
- Alaya A, Pelikan, H. How useful is ultrasound in diagnosing EUGs? Case report. J Urgent Care Med. 2022;16(4):23-27.
- Asfour V, Varma R, Menon P. Clinical risk factors for ovarian torsion. J Obstet Gynaecol. 2015;35(7):721-725.
- Bardin R, Perl N, Mashiach R, et al. Prediction of adnexal torsion by ultrasound in women with acute abdominal pain. Ultraschall Med. 2020;41(6):688-694.
- Cohen SB, Weisz B, Seidman DS, et al. Accuracy of the preoperative diagnosis in 100 emergency laparoscopies performed due to acute abdomen in nonpregnant women. J Am Assoc Gynecol Laparosc. 2001;8(1):92-94.
Published online ahead of print March 8, 2022.
Author affiliations: Andrew Alaya, MD, MSC, Bronovo Hospital, The Hague, Netherlands. The author has no relevant financial relationships with any commercial interests.

