Urgent message: Initial evaluation of a patient with an arrhythmia in the urgent care setting can be as difficult as it is critical to the patient’s survival—one key concern being sudden cardiac death, which occurs in roughly 328,000 cases annually.
Riaz Fabian, DO
Introduction
Cardiac arrhythmias are a group of conditions in which a patient has an abnormal heart rate or rhythm. They are caused by any disruption of the electrical conduction system of the heart, which impacts the normal activation sequence of the myocardium. Arrhythmias can be broadly classified into four main categories: extra beats, supraventricular tachycardia, ventricular arrhythmias, and bradycardia arrhythmias.
- Extra beats include premature atrial contractions (PACs), premature ventricular contractions (PVCs), and premature junctional contractions (PJCs). Extra beats are very common and usually not associated with long-term complications. Extra beats can occur naturally, but can also be associated with caffeine, excessive exercise, nicotine, or stress.
- Supraventricular tachycardia types include atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia. They are caused by abnormal electrical activity in the upper portion of the heart above the ventricles. These arrhythmias are typically caused either by an abnormality in the AV node or an abnormal pathway that bypasses the normal electrical conduction pathway of the heart.
- Ventricular arrhythmias include ventricular tachycardia and ventricular fibrillation. In these cases, the abnormal electrical activity originates in the ventricles themselves. Ventricular tachycardia can either be sustained or nonsustained. If sustained for a long period of time, ventricular tachycardia is capable of causing hemodynamic compromise, as the ventricles contract too quickly to fill completely. It can also lead to ventricular fibrillation, which results from disorganized electrical activity that causes the myocardium to quiver rather than pump effectively, resulting in cardiac arrest. Ventricular fibrillation is a cardiac emergency, and must be treated quickly to avoid death. Potential causes of ventricular arrhythmias include coronary artery disease, myocardial infarction, and electrolyte imbalances.
- Bradyarrhythmias are defined as a heart rate <60 beats per minute. This may be a normal finding in well-conditioned athletes, but may also be caused by an abnormality in the sinus node or conduction blocks in the heart’s electrical system.
The initial evaluation of a patient presenting with an arrhythmia can be difficult, as many of the signs and symptoms present are nonspecific. One common presentation is the sensation of a rapid or irregular heartbeat, also known as palpitations. If the arrhythmia is severe enough to impede cardiac output, the patient may also complain of chest pain, lightheadedness, or syncope. One of the biggest concerns regarding arrhythmias in the urgent care setting is the development of sudden cardiac death. Sudden cardiac death occurs in arrhythmias.1,2
In a suspected arrhythmia, the most important steps for the urgent care provider include confirmation of hemodynamic stability and, if present, to obtain a 12-lead EKG or rhythm strip. The following discussion will focus on arrhythmias which may present to the urgent care, with a discussion of etiology, urgent care management, and considerations for transfer.
Case Presentations
Case 1
A 74-year-old man presents to urgent care with a chief complaint of racing heart and generalized weakness of 2 days’ duration.
Case 2
A 73-year-old male presents to urgent care with a chief complaint of intermittent palpitations of 2 weeks duration. He is a smoker and uses 2 L/min of home oxygen, but denies any new shortness of breath.
Case 3
A 42-year old female presents to urgent care with a chief complaint of intermittent palpitations of 2 weeks duration. She has previously been diagnosed with anxiety. Her EKG shows the following:
Case 4
A 26-year-old male presents to urgent care with a chief complaint of palpitations of 3 days duration.
History of Present Illness
The first step in evaluating a complaint of palpitations or a clinical finding of an irregular, rapid, or slow heart rate is to obtain a history directed toward life-threatening etiologies, including acute coronary syndrome. This would include assessing for the following:
- Chest pain, tightness, pressure, or discomfort
- Shortness of breath
- Diaphoresis
- Dizziness
- Fatigue
If any of the above are present and there is concern for acute coronary syndrome, pulmonary embolism, aortic dissection, or other life-threatening condition, initiate emergent transfer.
Next, evaluate the complaint of palpitations further. For the patient with suspected arrhythmia, focus on:
- Timing and duration of symptoms
- Constant or intermittent
- Onset; abrupt onset is suggestive of supraventricular tachycardia (SVT) or ventricular tachycardia (VT)
- Associated symptoms (eg, dizziness, chest pain, shortness of breath) which occur during the sensation of palpitations
- Known history of arrhythmias, structural heart disease, endocrine disorders such as hyperthyroidism, or psychiatric disorders such as anxiety, all of which are potential risk factors for the development of an arrhythmia3,4
- Assess for sympathomimetic drugs, vasodilators, anticholinergics, diuretics which may cause electrolyte abnormalities, or beta blocker withdrawal
- Substance abuse, especially stimulants such as cocaine and amphetamines
- Previous therapies
- History of cardiovascular disease, recent surgical or invasive procedures, or any new medications5
Note that younger patients or patients with a history of palpitations are more likely to have an arrhythmia such as SVT. Atrial fibrillation is more commonly seen as patients become older.
Physical Examination
Physical examination begins with an assessment of the vital signs. If there are signs of hemodynamic instability, including hypotension, tachypnea, hypoxemia, or confusion, transfer should be initiated.
The most important parts of the physical exam include the following:
- General appearance – Pale or grey in appearance, diaphoretic, confused
- Neck – JVD, which may occur from heart failure or cardiac tamponade
- Respiratory – Bibasilar crackles may be present with heart failure, wheezing may be present in COPD (which may occur with multifocal atrial tachycardia)
- Cardiovascular – Assess heart rate and rhythm (regular or irregular). Arrhythmias may be associated with certain heart murmurs (eg, supraventricular arrhythmias and nonsustained VT are commonly associated with a mitral valve prolapse6; hypertrophic cardiomyopathy (HCM) has been associated with Afib and VT.7 This condition is characterized by a harsh holosystolic murmur that increases with Valsalva maneuver and standing from a squatting position)
- Peripheral pulses – Regularity and character of patient’s pulses should be noted; an irregular rhythm may be suggestive of atrial fibrillation
- Extremities – Check for edema, temperature, mottling, and pallor
Diagnostic Workup
Often, it is useful to follow a step-wise process for EKG interpretation:
- Rate
- Normal rate
- Bradycardic or tachycardic
- Rhythm: Determine rhythm; regular vs irregular
- Examine P waves
- Are p waves present?
- Are the p waves uniform?
- Do p waves have 1:1 relationship with QRS complex?
- Atrial flutter may have a P to QRS ratio of 2:1, 3:1, 4:1 or more
- In 2nd degree heart block (Mobitz Type I), the PR interval progressively lengthens until a QRS is dropped.
- In 2nd degree heart block (Mobitz Type II), the QRS beats are intermittently dropped without PR prolongation.
- In 3rd degree block, there is a complete dissociation between P waves and QRS complex. This indicates that the atria and ventricles beat independently of one another.
- Is P-R interval normal? (0.12-0.20s)
- In first degree AV block, PR interval exceeds 0.20 seconds
- Is P-R interval constant?
- Examine QRS Complex
- Normal duration? (0.08-0.12s)
- Is QRS wide? (>120 ms)
- Does QRS complex occur at regular intervals? If not, this may suggest an irregular rhythm like atrial fibrillation
- Look for signs of infarcts/ischemia. Myocardial ischemia may cause an increase in the activation of the sympathetic nervous system, primarily due to pain. This predisposes a patient to the development of ventricular and supraventricular tachyarrhythmias.
- Q waves (sign of prior infarct)
- ST Elevation (sign of infarction)
- ST Depression (sign of ischemia)
- T wave inversion (sign of ischemia)
Laboratory testing
Typically, laboratory testing is not necessary for an asymptomatic benign arrhythmia; however, if an abnormality is suspected in a stable patient, consider checking electrolytes or thyroid studies. If the patient is unstable, with symptoms concerning for myocardial infarction or pulmonary embolism, or with a life-threatening arrhythmia, emergent transfer is indicated.
Management of Specific Arrhythmias
The treatment of a cardiac arrhythmia depends primarily on whether or not the patient is hemodynamically stable. If the patient is unstable, initiate ACLS/BLS; cardioversion if applicable.
Patients with hemodynamic instability (ie, low blood pressure, altered mental status, and other signs of hemodynamic compromise) or who have cardiac arrhythmias accompanied by chest pain (which may be a sign of myocardial ischemia) must be transferred to a hospital.
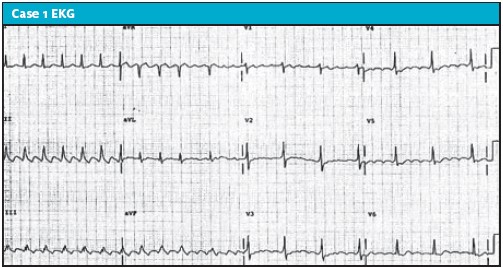
Case 1 Diagnosis: Atrial Flutter
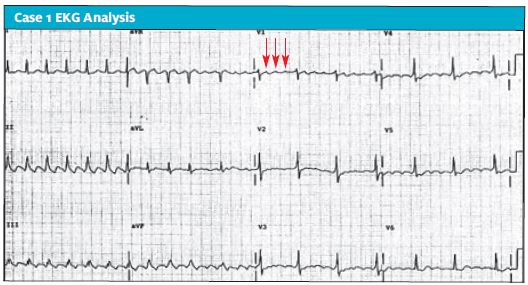
In case 1, a 74-year-old man presented with the complaint of racing heart and generalized weakness of 2 days’ duration.
EKG analysis
This EKG demonstrates the classic “saw-tooth” pattern of atrial flutter. This arrhythmia is characterized by a ventricular rate of approximately 150, and multiple p waves preceding a QRS pattern in a 2:1, 3:1, or a 4:1 pattern. The ventricular rate will vary according to this pattern. A 2:1 atrial flutter, for example, with an atrial rate of 300 beats per minute will produce a ventricular rate of 150.
The presence of p waves in this EKG rules out SVT and ventricular tachycardia. The presence of uniform p waves rules out multifocal atrial tachycardia. The presence of multiple p waves preceding the QRS complex rules out sinus tachycardia.
Key points for atrial flutter
- Keep in mind that atrial flutter can be a regular or irregular rhythm, and may be difficult to distinguish from sinus tachycardia. Differentiation between the two can be made with an EKG
- Classic “saw tooth” pattern best seen in leads II and VI
- As with atrial fibrillation, patient may be at risk for subsequent CVA; anticoagulation must therefore be considered.
- A thorough H&P is of utmost importance in assessing the patient for signs and symptoms of hemodynamic compromise and ischemia
Pearls for urgent care management/considerations for transfer
- A 12-lead ECG should be done to evaluate for other causes of tachycardia that may not be seen on a simple cardiac monitor (eg, Wolff-Parkinson-White syndrome, ischemia, and SVT)
- Distinguish between first episode and subsequent episode, duration of palpitations, and whether the patient is anticoagulated, as this may have implications for rate vs rhythm control
- Almost all such patients require transfer to the emergency department, unless there is a history of atrial fibrillation/flutter and the rate spontaneously returns to normal; the patient should be placed on a monitor and observed in the urgent care center while waiting for transport
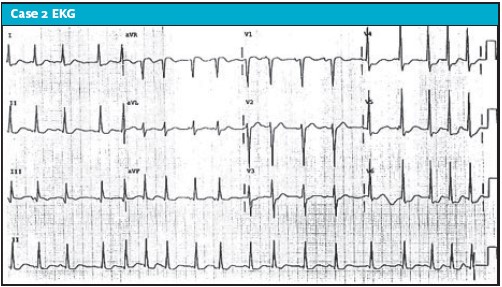
Case 2 Diagnosis: Multifocal Tachycardia (MAT)
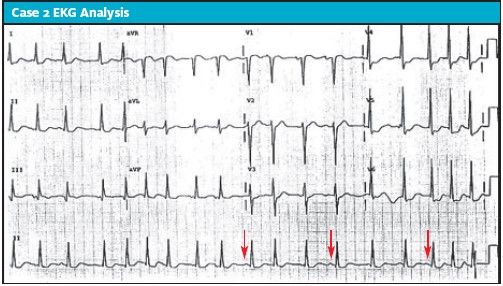
In case 2, a 73-year-old male presented to urgent care complaining of intermittent palpitations of 2 weeks’ duration. He is a smoker on 2 L of home oxygen.
EKG analysis
This patient’s EKG reveals the presence of an irregular rhythm, but it is sinus. Notice the different p wave morphology. There are some nonspecific ST changes, but no ST elevation concerning for an acute MI. There are prominent r waves consistent with left ventricular hypertrophy (LVH). The arrows point to the “multifocal” p waves.
Learnings/what to look for:
- MAT is an atrial rhythm, and not ventricular
- Complexes are narrow and irregular, but p waves are present, ruling out atrial fibrillation
- The ST segments are decreased in the anterior lateral leads (V4-6), but this is a nonspecific finding. Comparison to past EKGs and correlation with the patient’s symptoms are important
- MAT occurs commonly in patients with COPD, likely present in our patient with his history of smoking and the scattered wheezing heard on lung auscultation
Pearls for urgent care management and considerations for transfer
- Although the rhythm is benign, the underlying cause may require further evaluation and management (eg, with sepsis, pulmonary embolism, or ischemia)
- Return to the bedside and use the history and exam to risk stratify for serious underlying causes of the MAT. Inquire about chest pain, shortness of breath, syncope, dizziness, diaphoresis, fever, medication, or drug use
- If the rhythm is found incidentally and the patient is asymptomatic/without new symptoms, further evaluation and management can be done on an outpatient basis
- Compare the EKG with previous EKGs if available
- Indications for transfer include suspicion of sepsis, respiratory failure, myocardial ischemia, pulmonary embolism, theophylline toxicity, or consideration of other life-threatening etiology
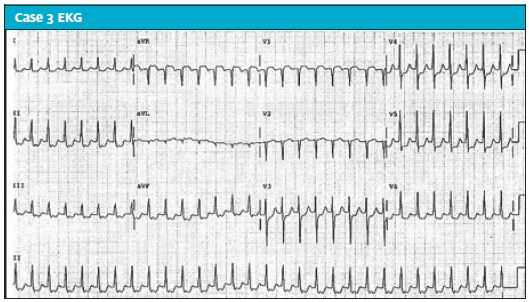
Case 3 Diagnosis: Supraventricular Tachycardia
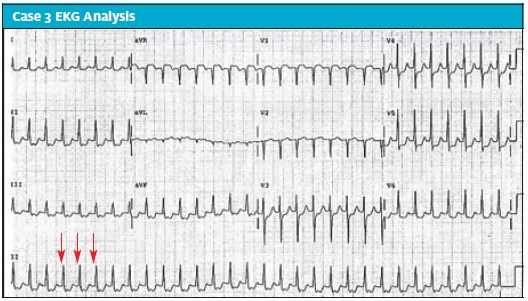
In case 3, a 42-year-old female with a known history of anxiety presented with intermittent palpitations of 2 weeks duration.
EKG analysis
The EKG reveals a tachycardic rate with regular rhythm, which excludes both atrial fibrillation and multifocal atrial tachycardia. There are no flutter waves, making the diagnosis of atrial flutter unlikely (also, the atrial flutter rate is typically 150). The QRS complexes are narrow, excluding ventricular tachycardia. P waves are not seen. The tracing is most consistent with supraventricular tachycardia. There are some ST depressions which could be a rate-related ischemia; these generally resolve with the management of the SVT.
Learnings/what to look for
- SVT is a regular, narrow complex and tachycardic rhythm
- The mechanism is a re-entrant tachycardia
- Distinguish from atrial fibrillation (irregular, irregular rhythm), atrial flutter (flutter waves and typical rate of 150), ventricular tachycardia (wide complex QRS), and sinus tachycardia (presence of p waves)
- Symptoms may include sensation of palpitations, lightheadedness, shortness of breath, chest pain, or weakness
Pearls for urgent care management and considerations for transfer
- Unstable patients displaying hypotension, confusion, diaphoresis, or chest pain should have an IV placed and be put on the monitor (if time allows) and be transferred to an emergency department
- Stable patients may attempt the Valsalva maneuver by “bearing down.” Postural modification, by having the patient Valsalva and the clinician perform a passive leg raise (per the recently published REVERT trial9) may also be effective
- ED management will initially proceed with adenosine administration, while unstable patients may require cardioversion
With SVT, consider Valsalva maneuver or postural modifications at the bedside.
- During the straining phase: Patient is placed on the bed in high Fowler’s position (head elevated to 80⁰─90⁰). Patients are then given a 10 mL syringe and told to blow continuously into the syringe for 15 seconds, displacing the plunger in the process. This is an effective way of generating the recommended 40 mmHg of intrathoracic pressure needed for the Valsalva maneuver8
- Relaxation phase: lay patient supine and manually elevate their legs
- In the REVERT trial, 43% of patients returned to normal sinus rhythm after the application of this method9,10
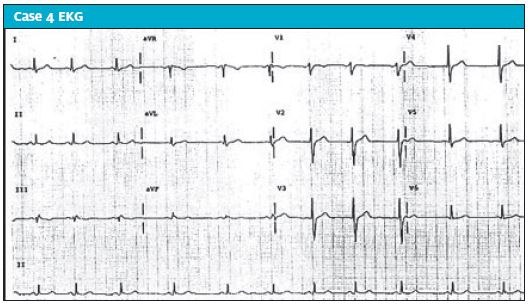
Case 4 Diagnosis: Sinus Arrhythmia
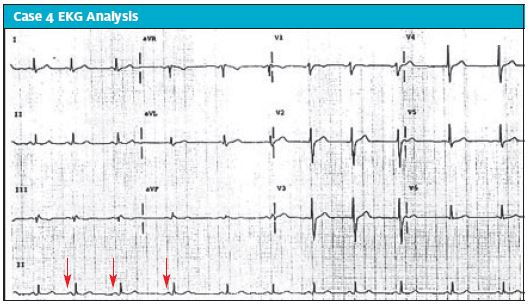
In case 4, a 26-year-old male presented complaining of palpitations of 3 days’ duration.
EKG analysis
The EKG revels a sinus rhythm, with p waves preceding each QRS, excluding atrial fibrillation. This is not a tachycardic rhythm (excluding MAT, SVT, or sinus tachycardia). The QRS interval is normal, ruling out a bundle branch block or a ventricular rhythm. There are no ischemic changes suggestion of ACS (no ischemic ST changes or abnormal T wave inversions). This EKG shows sinus arrhythmia.
Learnings/what to look for
- Sinus arrhythmia is common in young patients and is a normal physiologic response, typically due to increased or decreased vagal tone during breathing (inspiration increases the vagal tone causing an decrease in the heart rate)
- It is a benign rhythm and sometimes will be appreciated by the patient, and other times may be asymptomatic
Pearls for urgent care management and considerations for transfer
- Sinus arrhythmia is a benign rhythm.
- If the rhythm is found incidentally and the patient is asymptomatic/without new symptoms, no further testing is necessary
- Compare the EKG to previous EKGs if available
- Indications for transfer include suspicion of ischemia, cerebral hypoperfusion (dizziness, altered consciousness, hypotension), sepsis, respiratory distress, pulmonary embolism, drug toxicity, or consideration of other life-threatening etiology
Conclusion
Cardiac arrhythmias are a common cause of morbidity and mortality and are important to recognize in the urgent care setting. An arrhythmia must be addressed in a timely fashion to prevent further morbidity (and mortality). A focused HPI and PE are of utmost importance in arriving at the correct diagnosis. A 12-lead EKG is necessary to determine the precise arrhythmia present. Based on the results of the EKG, treatment can be geared toward preventing hemodynamic compromise, and possibly restoring the patient to sinus rhythm. In certain cases, patients may need to be placed on long-term anticoagulation. In addition, certain lifestyle modifications (eg, smoking cessation, reducing or eliminating caffeine, regular exercise) may help reduce the risk of further arrhythmias in the future.
Citation: Fabian R, Coats LW. Urgent care evaluation of arrhythmias. J Urgent Care Med. January 2018. Available at: https://www.jucm.com/urgent-care-evaluation-arrhythmias/.
References
- Kronick SL, Kurz MC, Lin S, et al. Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 132;(18 Suppl 2):S397–413.
- Mehra R. Global public health problem of sudden cardiac death. J Electrocardiol. 2007;40(6 Suppl):S118–122.
- Klein I, Danzi S. Thyroid disease and the heart. Circulation. 2007;116(15):1725-1735.
- Ehlers A, Mayou RA, Sprigings DC, Birkhead J. Psychological and perceptual factors associated with arrhythmias and benign palpitations. Psychosomatic Med. 2000;62(5):693-702.
- Weber BE, Kapoor WN. Evaluation and outcomes of patients with palpitations. Am J Med. 1996;100(2):138-148.
- Turker Y, Ozaydin M, Acar G, et al. Predictors of ventricular arrhythmias in patients with mitral valve prolapse. Int J Cardiovasc Imaging. 2010;26(2):139-145.
- Adabag AS, Casey SA, Kuskowski MA, et al. Spectrum and prognostic significance of arrhythmias on ambulatory Holter electrocardiogram in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2005;45(5):697-704.
- Smith G, Boyle M. The 10 mL syringe is useful in generating the recommended standard of 40 mmHg intrathoracic pressure for the Valsalva manoeuvre. Emerg Med Australas. 2009;21(6):449-454.
- Appelboam A, Reuben A, Mann C, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet. 2015;386(10005):1747-1753.
- Baker A, Whitbread M, Richmond L, et al. Safety and efficacy of paramedic treatment of regular supraventricular tachycardia. Heart. 2013;99 (suppl 2):A46.1-A46.


