Published on
Urgent message: Treating preverbal children can be challenging under every-day circumstances for pediatricians who know the child and the family. Urgent care providers who may not have the benefit of that history must be especially vigilant for all available signs and symptoms to make diagnoses based on the full scope of the presentation.
Michael Weinstock, MD
Case Presentation
(Please note: The Case Presentation is drawn directly from the treating physician’s notes, without editing or correction, to reflect the conditions at the time of presentation.)
5 month old male with multiple visits for URI in the past with complaint of cough for 4 days associated with clear rhinorrhea and tugging at the ears. Taking fluids and bottle well. There have been 8 wet diapers. Does have diarrhea X 4. Mother complains of easy bruising and there is bruising at the external right ear and left wrist. Had been on an ATB 2-3 weeks ago—does not know name of ATB.
Hx: URI
Meds: None
Social history: Presents with the mother
Immunization history: Immunizations are UTD
Physical Exam
General: No acute distress
Head: Ant. fontanelle is soft and concave
Neck: Soft and supple without meningeal signs
Oral: Mucous membranes are well hydrated
Ears: TM’s pink bilat
Lungs: Coarse breath sounds without wheezing
CV: RRR
Abd: Soft, NT, positive bowel sounds
Skin: Hyperkeratotic areas without petechiae/purpura to right temple area. Positive ecchymosis to superior helix right ear. No petechiae/purpura about torso or extremities or face
Differential Diagnosis
- Pneumonia
- Thyromegaly
- Pneumothorax
- Pulmonary TB
- Cardiomegaly
Diagnosis
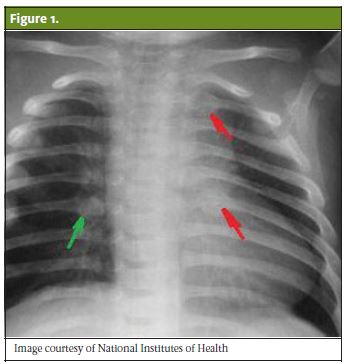
Multiple rib fractures with suspicion for child abuse
On the Front Lines in the Urgent Care Center: Where Do I Go Next?
A discussion of the evaluation and management of child abuse
General
Child maltreatment is divided into four categories:
- Child neglect
- Physical abuse
- Emotional abuse
- Sexual abuse
Child maltreatment is underreported and underdiagnosed due to difficulty with recognition and failure to consider this in the differential diagnosis. Neglect is the most common child maltreatment, with physical abuse second. Physical abuse affects all cultures and socioeconomic groups. The incidence is similar for male and female children. This risk of abuse increases with age, but fatal and serious injuries are most common under the age of 2. The Fourth National Incidence Study of Child Abuse and Neglect (NIS-4) reported that in the U.S. 1.25 million children were maltreated: 61% neglected, 26% physically abused, 12% emotionally abused, and 11% sexually abused (children may fall into more than one category). Each year, there are 1,500 deaths per year from child abuse, with 80% occurring in children <4 years of age.
Risk factors for parents include difficulty bonding with the child, a caregiver who was maltreated as a child, unrealistic developmental expectations, disciplines with physical punishment, physical/mental/cognitive health issues, parental lack of self-control, alcohol/drug abuse, criminal activity, social isolation, depression or low self-esteem, lack of parenting skills due to age or lack of education, and financial difficulties.
Risk factors for the child include being an unwanted baby, high needs (prematurity, disabled, chronic illness), difficult to comfort, mental health issues, multiple birth, many siblings, exhibits violence, criminal behavior, self-abuse, animal abuse, and aggression toward peers.
Obtaining the History
History starts with an exploration of risk factors (as listed above), including prematurity, alcohol/drug abuse in the caregivers, financial difficulties, developmental delay in the child which may lead to poor child-parent bonding, and accidental pregnancy or unwanted children. Additional history incorporates a pediatric history including birth history, immunizations, siblings, milestones; a social history including caregivers, parental substance use, and socioeconomic status; and a family history of any hypocoagulable states or history of siblings or parent with nonaccidental injuries.
Physical Examination
Observe interaction with parent(s) or caregiver, respiratory rate, and general appearance (ie, well-kept vs disheveled). Examine the skin for bruising in concerning locations such as around the ear, face, and areas not likely to be injured with typical pediatric activities. In our case, a 5-month-old would be nonambulatory and not expected to have any bruising. Eyes should be checked for retinal hemorrhages, facial fractures, or bruising. Inspect the chest for pain or swelling, and old vs new fractures. Check the abdomen for pain secondary to internal injury and inspect and palpate the extremities for fractures, bruising, or burns.
Testing
X-ray will be determined based on location of pain. With strong suspicion of abuse in an infant, a skeletal survey may be done. An initial skeletal survey (Kempe series) will assess for occult fractures. Rib fractures and long-bone fractures are more prevalent in children with inflicted traumatic injuries, with rib fractures having the highest probability for abuse at 70%. There is a high correlation between multiple fractures and abuse; 80% of inflicted fractures are seen in children <18 months old.
Advance imaging with CT or MRI will rarely be done, but can be considered if indicated. Noncontrast head CT will evaluate for subdural hematoma, subarachnoid hemorrhage, cerebral contusion, cerebral edema, infarction, and white matter changes. A diffusion-weighted MRI may distinguish between acute and chronic cerebral infarction.
Labs will rarely be indicated, but consideration of clotting abnormalities with bruising can be obtained (typically from the receiving hospital). If a bleeding problem is suspected, a basic bleeding evaluation (platelets, PT, and PTT) may suggest the need for more sophisticated bleeding evaluation and/or hematology consultation.
Indications for Transfer
Most patients with the following will be sent to the ED (if there is a pediatric emergency department, this is preferential):
- Hemodynamic instability
- Altered consciousness
- Shortness of breath
- Retinal hemorrhages
- Concerning symptoms (eg, abdominal pain or headache) with diagnostic uncertainty and suspicion of child maltreatment
- Suspicion of child maltreatment that requires emergent intervention and evaluation
Management
Any suspected child maltreatment must be reported. Mandated reporters, which include physicians, are required to report suspected child maltreatment to the appropriate authorities. Professionals (physician, teacher, nurse, social worker, etc.) reporting in good faith are immune from legal liability arising from the report. However, failure to report can result in both malpractice liability and criminal prosecution. Typically, severely injured children have a history of prior “minor” injuries (as in this case) and/or a history of abuse in siblings. This means there may be an opportunity to prevent significant morbidity and mortality either to the “index” abused child and/or to their siblings.
Summary/Clinical Pearls
- Bruises (or fractures) in a nonambulatory infant is presumed to be child abuse until proven otherwise
- Physicians are mandated to report any suspicion of child abuse. Failure to do so can lead to criminal penalties for the physician, in addition to malpractice claims
- Inflicted bruises typically have a regular uniform appearance, a distinct pattern, occur in protected nonexposed areas, and are of different ages
Citation: Weinstock MB. A 5-month-old with symptoms beyond the presenting complaint. J Urgent Care Med. January 2018. Available at: https://www.jucm.com/5-month-old-symptoms-beyond-presenting-complaint/.

