Urgent message: The differential diagnosis for unilateral testicular pain includes testicular torsion; this is a ”must not miss” diagnosis, as delayed diagnosis can cause significant morbidity both physically and psychologically.
Jeannette Vaughn-Dotterer, PA-C
CASE PRESENTATION
ML is a 47-year-old male who developed left-sided testicular pain after getting out of bed 2 hours prior. He states that his left testicle appears to be “dancing” and seems to be riding higher than his right testicle. ML states that the pain has been constant and that nothing seems to make it better; conversely, sitting or walking seems to increase the pain. He denies trauma, recent infection, fever, or previous surgery to his testicles. He also denies history of sexually transmitted infections, pain with intercourse, dysuria, penile discharge, or hernias. He states that he felt fine when he went to bed last night. His past medical history includes anxiety and glomerulonephritis. Currently he is taking alprazolam (Xanax), clonazepam (Klonopin), and venlafaxine (Effexor). ML has an allergy to cefuroxime, which causes a rash. He denies illicit drug use or smoking. Previous surgical history includes sinus surgery, appendectomy, and knee arthroscopy.
Observations and Findings
Evaluation of the patient reveals the following:
- Temp: 98.4°F
- Pulse: 78
- Respiration: 16
- BP: 114/88
- O2Sat: 98% RA
- CV: Normal RRR, no murmurs, gallops, or rubs
- Lungs: Clear to auscultation
- Abdomen: Nontender, no guarding, no distention, well-healed surgical scar noted in RLQ, no suprapubic tenderness or masses noted
- Genitourinary: Left testicle is swollen and sitting in a horizontal orientation; it is higher than the right testicle; significant tenderness to palpation is noted to the left testicle
Differential diagnoses were testicular torsion, epididymitis, sexually transmitted infection, symptomatic hydrocele, scrotal hematoma, inguinal hernia, orchitis, and malignancy.
Course and Treatment
The patient was referred to the emergency department for further evaluation and to rule out testicular torsion. Scrotal ultrasound confirmed that the patient had a left-sided testicular torsion. The patient opted not to have emergent orchidopexy (fixation of the testicle) so the treating physician manually detorsed the left testicle, providing immediate relief of the patient’s pain. Precautions for return to the hospital included return of pain, redness, swelling, and vomiting. He was discharged home with a referral to urology.
DISCUSSION
Testicular torsion is a condition characterized by the rotation of the testicle around the spermatic cord, causing decreased blood flow to the testicle and possibly resulting in testicular ischemia, infertility, and loss of the testis. Typical presentation includes acute unilateral scrotal pain, with nausea and vomiting, scrotal swelling, a horizontal high-riding testicle, and loss of cremasteric reflex on physical exam.1
This is a medical emergency and requires prompt diagnosis and intervention. The urgent care clinician needs to include testicular torsion in the differential any time a patient presents with acute onset of unilateral scrotal pain.
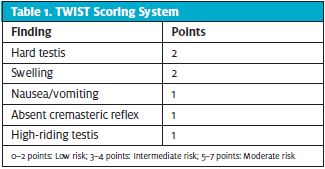
A clinical scoring system can be used in conjunction with a thorough physical exam by the urgent care provider to identify patients at higher risk for a testicular torsion vs those with testicular pain with a different underlying etiology. TWIST (Testicular Work-up for Ischemia and Suspected Torsion) is utilized to determine if the patient is low, intermediate, or high risk for torsion (Table 1).2 TWIST has been validated only in children, but can be useful in adults; a high TWIST score should prompt a call to the urologist and consideration of taking the patient to the operating room without imaging. The Prehn sign, relief of scrotal pain with elevation, should not be solely used as a predictor for testicular torsion.3
Testicular torsion can be caused by genetic predisposition, environmental factors such as cold weather, trauma, and the “bell clapper deformity” where the tunica vaginalis is attached high, allowing the spermatic cord to twist inside causing torsion of the testicle.4
Patients who have a low score on the TWIST assessment should have ultrasound performed. Those with a high score, placing them in the moderate risk category, can forgo the ultrasound and go straight to surgery.3 Doppler ultrasound is the diagnostic imaging study of choice to assess both arterial and venous blood flow and should be performed on both the unaffected and affected testis. Findings will show decreased color or flow in a patient with a testicular torsion.
Testicular torsion is a time-sensitive surgical emergency. Surgical exploration of the scrotum with orchidopexy is the gold standard treatment. A timeframe from testicular torsion to surgical exploration of less than 6 hours of pain has a higher organ salvage rate when compared with a time frame greater than 12 hours of pain.1,5
Manual detorsion should be considered when the timeframe for exploration is going to be prolonged. Manual detorsion is performed by grasping the affected testicle by the thumb and middle finger and rotating the testicle medial to lateral. This maneuver may take up to four tries before the patient gets relief. After manual detorsion the patient should have an ultrasound performed to verify adequate blood flow to the testicle. Manual detorsion should be followed by surgical exploration and orchidopexy (fixation of the testicle).1 Surgical exploration should still be performed followed by orchidopexy or orchiotomy if the testis is necrosed.
CONCLUSION
Testicular torsion is a medical emergency affecting approximately a quarter of patients presenting to the emergency room complaining of scrotal pain.4 Door to detorsion time should be less than 6 hours from onset of pain in scrotum, increasing the odds of a favorable outcome. Recognition of patients with a testicular torsion requires a thorough physical exam as well as close attention to presenting symptoms of hard testis, high-riding testis, testicular swelling, nausea/vomiting, and absence of a cremasteric reflex.
REFERENCES
- 1. Howe A, Vasudevan V, Kongnyuy M et al. Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion. Transl Androl Urol. 2017;6:1159-1166.
- 2. Barbosa JA, Tiseo BC, Barayan GA, et al. Development and initial validation of a scoring system to diagnose testicular torsion in children. J Urol. 2013;189(5):1859-1864.
- 3. Schick M. Testicular Torsion. Stat Pearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448199/. Updated November 20, 2020. Accessed April 24, 2021.
- 4. Laher A, Ragavan S, Mehta P, Adam A. Testicular torsion in the emergency room: a review of detection and management strategies. Emerg Med. 2020;12:237-246. 5. Gold D, Lorber A, Levine H, et al. Door to detorsion time determines testicular survival. Urol. 2019;133:211-215.
Read Similar Articles
- Evaluation Of Scrotal Pain In The Urgent Care Setting
- Assessment And Management Of Scrotal Disorders
- Epididymitis-The Optimal Urologic Evaluation Management Approach In The Urgent Care Setting

