Urgent message: Hypogonadism not only impedes biological development, but also negatively impacts a patient’s sense of identity and well-being. Prompt diagnosis is achievable through strategic utilization of hormone level testing in conjunction with a patient’s stated symptoms and medical history.
Lisa O. Iyeke, BS and Mark J. Richman, MD, MPH
Citation: Iyeke LO, Richman MJ. Evaluating decreased libido: the lowdown on low T. J Urgent Care Med. 2021;16(6):33-34.
CASE PRESENTATION
A 46-year-old male with benign prostatic hypertrophy (BPH) presents with complaints of low libido, depression, erectile dysfunction, and no morning erections. He denied other hypogonadism symptoms such as weight gain or diminished energy, cognitive function, or muscle mass; nor did he have other conditions associated with hypogonadism (eg, cardiovascular disease, osteoporosis/low-trauma fractures, or infertility).1 His medications were finasteride and terazosin. Physical examination revealed a euvolemic patient with body mass index (BMI) of 33.8, clear lungs, normal cardiac examination, no pallor, no palpable thyroid nodules or rash, and normal-size testes.
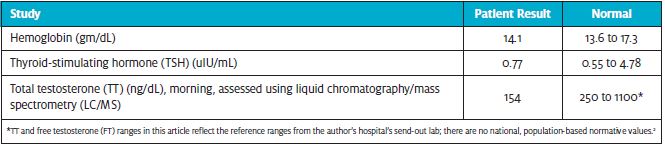
Laboratory Results
Next Steps (?)
- Which of the following would be your next step(s) in the diagnosis of hypogonadism? Measure morning free testosterone (FT)
- Repeat morning total testosterone (TT)
- Measure sex hormone binding globulin (SHBG) alone
- No additional testing is required
The answer is 1, measure morning free testosterone (FT).
TESTOSTERONE: PHYSIOLOGICAL EFFECTS AND TEST CHARACTERISTICS
Testosterone is important for physical, mental, and emotional health and secondary sex characteristic development. It is commonly measured to investigate declines in sexual interest/function, strength, mood, concentration, and memory. However, symptoms/signs do not predict testosterone levels, and vice versa3; not all symptomatic men have low levels, and many with low levels are asymptomatic.4 Considering response to therapy as diagnostic of hypogonadism, one study found 63% sensitivity.5 Therefore, hypogonadism should be diagnosed by compatible symptoms/signs plus repeatedly low testosterone levels.11
Testosterone as a diagnostic test for hypogonadism is complicated by its requirement to be measured at 8-10 am (outside acute/subacute illness), an incomplete correlation with symptoms/signs, an increasing prevalence of conditions affecting sex hormone-binding globulin (SHBG), and a lack of population-based reference ranges or standardized lab assays and reference values.2 Accordingly, TT, the recommended screening test,2 is suboptimal. TT assays vary, though the Centers for Disease Control and Prevention is coordinating standardization via its Hormone Standardization project.6 Extraction and liquid chromatography/mass spectrometry (LC/MS) assays are more sensitive/specific than immunoassays.7
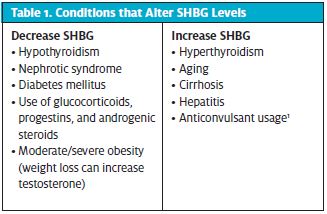
Patients with low initial TT should have a repeat TT; if altered SHBG levels are suspected, FT or bioavailable testosterone should be measured. Of note, there are conditions that decrease SHBG and increase SHBG (Table 1). Consequently, conditions that increase SHBG are also associated with less bioavailable testosterone. Medicare reimburses ~$35 for measuring FT, TT, and SHBG8; laboratories charge $80/test (~$200/bundle) or more.
Next Steps (?) Round 2
Given what you now know about this patient, which of the following would be your next step(s) in the diagnosis of hypogonadism?
- Measure morning free testosterone (FT)
- Repeat morning total testosterone (TT)
- Measure sex hormone binding globulin (SHBG) alone
- No additional testing is required
Option 1 is correct, and 2 is incorrect. FT should be measured. TT is inaccurate when SHBG
levels are altered, which can occur in obesity(as in this patient with BMI = 33.8). Testosterone is loosely bound to SHBG (60%) and tightly bound to albumin (37%). Albumin-bound and free testosterone are bioavailable; however, only the 2% to 3% circulating as FT is bioactive.1 Because TT consists of SHBG-bound testosterone, albumin-bound testosterone, and FT, conditions altering SHBG produce inaccurate measurements of effective testosterone levels.
Option 3 is incorrect. While a normal SHBG level increases the likelihood that TT is accurate, TT must be measured concurrently; FT and bioavailable testosterone can be calculated using TT and SHBG.
Option 4 is incorrect. Owing to daily variation, two testosterone measurements, on separate mornings, outside acute/subacute illness, are required; 30% of men with initially abnormal levels have normal repeat values.9
What Are Alternative Diagnostic Testing Approaches?
Given the above-mentioned challenges in diagnosing hypogonadism, the Endocrine Society has published standard guidelines.1 Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels should have been measured to differentiate primary (high FSH and LH) from secondary (low or normal FSH and LH) hypogonadism. Primary hypogonadism in patients with small testes should be investigated using a karyotype to evaluate for Klinefelter syndrome; secondary hypogonadism should be investigated via pituitary MRI. Asymptomatic patients seeking screening for low T should be informed screening is recommended only for patients at risk for hypogonadism: sellar disease, glucocorticoid or opioid therapy, HIV-associated weight loss, chronic hemodialysis, infertility, or osteoporosis/low-trauma fracture.
Patient Outcome
Morning FT, assessed using equilibrium dialysis at a reference laboratory (as commercial assays for FT are inaccurate)10 returned 31.4 pg/mL (normal 35.0 to 155.0 pg/mL), confirming hypogonadism. Given symptoms and repeatedly low levels, hormone replacement therapy was started. Although hypogonadism is associated with cardiovascular events,11 this patient was relatively young and without cardiovascular risk factors. After initiating therapy, the patient reported improved energy, mood, libido, and erectile function. Repeat testosterone levels had not yet been drawn. The patient’s physicians considered that finasteride and terazosin are associated with hypogonadal symptoms. However, finasteride is not associated with low testosterone, making it unlikely his symptoms and laboratory findings were due to this medication. Finasteride and terazosin were continued, as discontinuation would have adversely affected his quality of life through untreated BPH.
Clinical Bottom Line
- Testosterone is best measured between 8 am and 10 am, outside acute/subacute illness. Given circadian and circannual variation in testosterone level, and test inaccuracy, hypogonadism cannot be confirmed with a single testosterone measurement.
- If initial TT (by LC/MS) is low, patients with suspected or confirmed altered SHBG levels should have bioavailable testosterone or FT (by equilibrium dialysis) measured, rather than repeat TT.
- Hypogonadism may be primary (testicular failure) or secondary (hypothalamic/pituitary failure, eating disorders, excessive exercise, chronic opiates, obstructive sleep apnea, glucocorticoids, GnRH analogs, anti-androgens).1 FSH and LH levels should be included in initial hypogonadism evaluation to distinguish between primary and secondary hypogonadism.
Take-Home Points
- Testosterone as a diagnostic test for hypogonadism is complicated by:
- Its requirement to be measured at 8-10 AM (outside acute/subacute illness)
- An incomplete correlation with symptoms/signs
- An increasing prevalence of conditions affecting sex hormone-binding globulin (SHBG)
- A lack of population-based reference ranges or standardized lab assays and reference values
- Extraction and liquid chromatography/mass spectrometry (LC/MS) assays are more sensitive/specific than immunoassays.
- Primary hypogonadism in patients with small testes should be investigated using a karyotype to evaluate for Klinefelter syndrome.
- Secondary hypogonadism should be investigated via pituitary MRI.
REFERENCES
- 1. Bhasian S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline.J Clin Endocrinol Metab. 2010;95(6):2536-2559.
- 2. Rosner W, Auchus RJ, Azziz R, et al .Position statement: utility, limitations, and pitfalls in measuring testosterone: an Endocrine Society position statement. J Clin Endocrinol Metab, 2007;92(2):405–413.
- 3. Ansong KS, Punwaney RB. An assessment of the clinical relevance of serum testosterone level determination in the evaluation of men with low sexual drive. J Urol. 1999;162(3 Pt 1):719-721.
- 4. Araujo AB, O’Donnel AB, Brambilla D, et al. Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the Massachusetts Male Aging Study. J Clin Endocrinol Metab.2004;89(12):5920-5926.
- 5. Buvat J, Lemaire A. Endocrine screening in 1,022 men with erectile dysfunction: clinical significance and cost-effective strategy. J Urol. 1997;158(5):1764-1767.
- 6. CDC Hormone Standardization Project (CDC-HOST Project): Standardization of Serum Total Testosterone Measurements. Available at: https://www.cdc.gov/labstandards/pdf/hs/Testosterone_Protocol.pdf Accessed September 17, 2021.
- 7. Bhasin S, Zhang A, Coviello A, et al. The impact of assay quality and reference ranges on clinical decision making in the diagnosis of androgen disorders. Steroids. 2008;73(13):1311–1317.
- 8. Medicare Clinical Laboratory Fee Schedule. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/index.html. Accessed September 17, 2021.
- 9. Brambilla DJ, O’Donnell AB, Matsumoto AM, McKinlay JB. Intraindividual variation in levels of serum testosterone and other reproductive and adrenal hormones in men. Clin Endocrinol. 2007;67(6):853-862.
- 10. Ly LP, Handelsman DJ. Empirical estimation of free testosterone from testosterone and sex hormone hormone-binding globulin immunoassays. Eur J Endocrinol. 2005;152(3):471-478.
Author affiliations: Lisa O. Iyeke, BS, Long Island Jewish Medical Center Department of Emergency Medicine. Mark J. Richman, MD, MPH, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell; Long Island Jewish Medical Center Department of Emergency Medicine. The authors have no relevant financial relationships with any commercial interests.
