Urgent message: Though epididymitis is clinically non-urgent, its symptoms are driving more and more men to urgent care, making it imperative that providers are familiar with its epidemiology, etiology, evaluation, and treatment.
Introduction
Epididymitis is among the most frequently diagnosed and treated conditions in men. Typically, men present to, and are diagnosed and treated by, their primary care physicians or their urologist.
Treatment is with antibiotics on an outpatient basis. Epididymitis is, in general, non-life threatening and non-urgent. However, afflicted patients experience significant distress from the symptoms and tend to seek treatment early.
Urgent care medicine is emerging as a distinct specialty, separate from both emergency medicine and primary care. From a patient’s perspective, an urgent care office visit would be an attractive alternative to an emergency room visit for a variety of reasons, especially if the patient perceives his symptoms to be non-life threatening, but is concerned nonetheless to the point of wanting immediate medical attention without long waits and other unpleasantries associated with an emergency department visit.
Epididymitis, for the most part, fits this description well and has become commonplace in urgent care centers. Therefore, it is imperative that urgent care physicians understand the epidemiology, etiology, evaluation, and therapy of epididymitis.
Etiology and Epidemiology
Sperm is produced in the testicle and matures in the epididymis, a long convoluted tube that sits adjacent to the testicle. From the epididymes, the sperm is transported via the vas deferens to the ejaculatory duct, in the prostatic urethra. It is at this location that infected urethral urine may access the male reproductive tract, ascend to the epididymis, and cause epididymitis. Sterile urine can also reflux up these ducts and cause a reactive, chemical epididymitis.
Epididymitis connotes inflammation of the epididymis, an accessory gland in the male reproductive tract. Classically, the inflammatory process is the result of bacterial infection, but it can be caused by viruses or reflux of sterile urine up the reproductive tract.
In men less than 35-years-old, Chlamydia is the likely agent, thus making epididymitis in this group a sexually transmitted disease.1,2 In men greater than 35-years-old, E coli is the most commonly isolated pathogen.
3
Hematogenous spread of bacteria is rare, but can occur with tuberculosis. True bacterial epididymitis in older men or children is typically associated with an anatomic abnormality, such as bladder outlet obstruction or a congenital urologic anomaly, such as an ectopic ureter.
Viral infection (e.g., mumps) may also cause epididymitis. Mumps epididymal orchitis is more common in the post-pubertal, pediatric population but has become uncommon due to the routine use of the mumps vaccine.
Fungal infections may also cause epididymitis, most notably in the immunocompromised.4-6 Other causes of epididymitis include medications (amiodarone), vasculitis ulititis (Henoch-Schönlein purpura), and parasites.
7-9
Epididymitis affects one in 350 U.S. men annually and has no race predilection.10
Diagnosis
History and Physical Examination
Men with epididymitis present with scrotal or testicular pain that can range from a mild, achy discomfort to severe pain with associated high fever and a leukocytosis. Men with the latter will most commonly present to an emergency department due to the severity of their symptoms and will occasionally require admission for intravenous antibiotics.
In an ambulatory setting, men more commonly present with milder complaints of testicular or scrotal pain. Occasionally, they will have dysuria or urinary frequency suggestive of a urinary tract infection (UTI), though often voiding symptoms will be absent.
A comprehensive medical history should be performed and specifically include a urologic history. The physician needs to inquire about any history of urinary tract surgery or instrumentation, voiding complaints, prior infections, and prior episodes of scrotal pain in the patient.
Finally, a sexual history, including prior sexually transmitted diseases, should be elicited and needs to include the patient’s use of safe sex practices, or lack thereof. A physical examination of the scrotum, testicles, and epididymis is to be done and will likely demonstrate tenderness over the involved epididymis. In severe cases, fluctulance is present. Occasionally, epididymitis will cause a reactive hydrocele to form and when large enough, the hydrocele will impair physical examination and prevent accurate diagnosis.
In this case, a scrotal sonogram is indicated. It is important to exam the testicles, as well, and to determine whether or not the acute scrotal pain is caused by testicular torsion or tumors, the two most serious diagnoses in the differential. The involved testicle in men with torsion will be very tender and have an abnormal transverse lie within the scrotum and the ipsilateral cremaster reflex will be absent, in general.
When testis torsion is suspected, the patient should be sent to an emergency department for immediate urologic consultation and, if need be, surgical detorsion.
Adjunctive Tests
Readily available adjunctive tests, when added to a comprehensive history and physical, can suggest or rule out the more serious conditions in the differential diagnosis. The urine analysis should be the first adjunctive test performed, and in severe cases of epididymitis will show pyuria. While the presence of pyuria suggests the diagnosis of epididymitis, it is not diagnostic and its absence does not rule out the diagnosis since patients can have fairly severe cases of epididymitis without urinary findings.
A urine culture should be performed, as well. The clean-catch method is the preferred technique, especially in the uncircumcised male, in whom preputial microbes can contaminate a urine specimen. The clean-catch technique involves instructing the man to retract his foreskin (if present) and clean the glans penis with an aseptic towelette, and then void midstream into the sterile collection cup. This technique should be used routinely in the urgent care setting and provides accurate urine culture results in men with minimal specimen contamination risk.
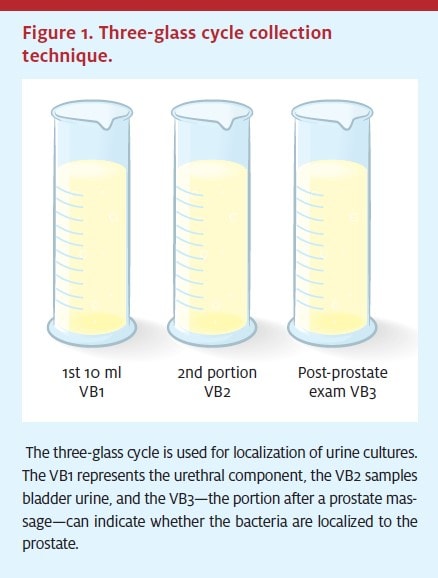
Alternatively, the three-glass cycle collection technique is optimal (Figure 1).11 In the three-glass cycle, the patient is asked to clean as above, and then to void the first 10 cc of urine into cup A, and the rest into cup B. The third specimen is collected into a sterile cup after the physician performs a prostate examination. This method can enable the physician to localize the source of the infection to the urethra (glass A), the bladder, (glass B), or the prostate (glass C). While the three-glass cycle is optimal, it is somewhat cumbersome to perform and is not routinely used nor mandatory in the urgent care setting.
A relatively new urine test that can detect Neisseria gonorrhea (GC) and Chlamydia in the urine via DNA amplification, the BD ProbeTec™ (Quest Diagnostics), is also available. It uses polymerase chain reaction (PCR) technology to detect GC and chlamydial DNA fragments in the urine of patients with suspected STDs.12-14
Other highly sensitive and specific PCR-based tests are also available. Men are simply asked to void into a sterile collection cup, and the urine is transferred to the preservative-containing transport tube with a pipette. No urethral swab is needed. Since epididymitis in young men is considered an STD and most commonly caused by chlamydial infection, the DNA urine probe has become a useful adjunct in the diagnosis and treatment of epididymitis.
Scrotal Sonogram
Perhaps the single most important adjunctive test is the scrotal sonogram.15-17 The scrotal sonogram is abundantly available, safe, painless to perform, and inexpensive and provides the most accurate diagnostic information relating to scrotal pathology. Sonograms will readily detect testicular tumors, even small, non-palpable ones, can visualize the testicle within a hydrocele, and has echo-features that are characteristic for epididymitis and orchitis. Most sonogram units today, even portable office-based units, have Doppler flow capabilities and are useful in ruling out the presence of testicular torsion.
However, if testicular torsion is even suspected, it is prudent for the evaluating physician to obtain a prompt urology consult or to send the patient immediately to the emergency room at a hospital that is equipped to handle this type of emergency.
Sonographically, epididymitis has findings that are suggestive, though not diagnostic, of the condition. These findings include hyperemia of the epididymes and surrounding testicle or epididymal engorgement. Often, a reactive hydrocele is present and can be seen on the sonogram. However, the most important sonographic findings are the absence of a testis mass and the presence of testicular blood flow on Doppler.16-17
Cautionary Notes
The clinician should bear the following cautions in mind at all times:
- The presence of Doppler flow in the testicle does not completely rule out testis torsion. In cases of suspected torsion, urologic consultation is mandatory.
- Epididymitis is uncommon in prepubertal boys. Acute scrotal pain in this population should be considered torsion until proven otherwise.
- Bacterial epididymitis in the pediatric population represents a urinary tract infection and needs to be evaluated appropriately.
Therapy
The treatment of epididymitis depends on a variety of factors that include the age of the patient, the severity of the presentation, and the patient’s medical history.
In young adults or in patients at risk for an STD, ceftriaxone sodium and doxycycline are the preferred agents due to their efficacy against Neisseria gonorrhea and Chlamydia. Ceftriaxone is given as a one-time dose, but doxycycline must be given for seven to 14 days, which can adversely affect compliance.
Alternatively, the treating physician may prescribe azithromycin, which is advantageous over ceftriaxone sodium and doxycycline with regard to both its antimicrobial spectrum of activity and for patient compliance.
Affected men should be counseled regarding the sexual transmissibility of the disease and their partners should be evaluated. In addition, it is prudent for the treating physician to discuss safe sex practices and barrier protection with the patient and to document the discussion in the medical record. Resumption of unprotected sexual intercourse with untreated partners is a vehicle for reinfection.
In older men, among whom E coli from either cystitis or a bacterial prostatitis source is the most common uropathogen, treatment with a fluoroquinolone antibiotic is preferred. The fluoroquinolone class of antibiotics is optimal due to the pharmacological properties of these agents, which allow them to penetrate the male reproductive tract, specifically the prostate, in high bacteriocidal levels.
The quinolones are also effective in the presence of bacterial pseudomembranes and even biofilms. Other antibiotic classes, such as the penicillins, lack these important pharmaco-qualities and their usage, while acceptable, is associated with higher treatment failure rates and disease recurrence rates. The duration of therapy can range from 14 days to six weeks, depending upon the underlying etiology of the epididymitis, its severity, and its responsiveness to treatment. For example, in men whose epididymitis was caused by an underlying bacterial prostatitis, an extended four-to six-week treatment period is indicated.18-22
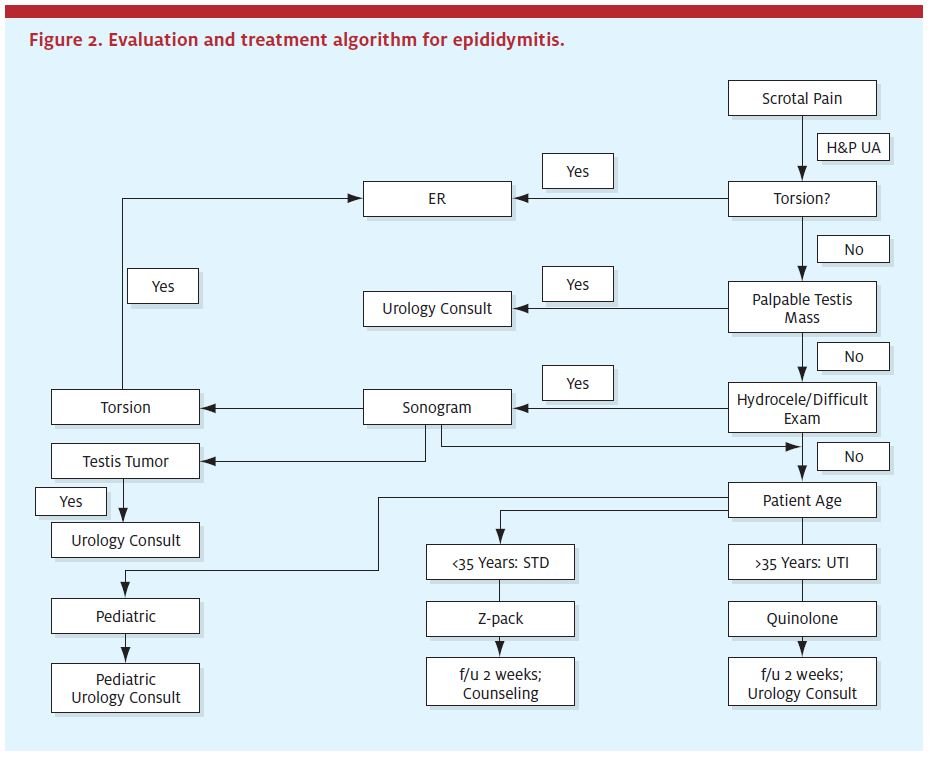
In the pediatric population, epididymitis is considered a UTI and is treated as appropriate. In general, a course of an antibiotic such as sulfamethoxazole/trimethoprim, nitrofurantoin, or amoxicillin can be given with a patient referral to a urologist or pediatric urologist. Quinolones are contraindicated for use in children in the United States due to perceived issues relating to cartilage growth. In addition, doxycycline can cause permanent teeth staining and must not be used in the pediatric population. See Figure 2 for an algorithm regarding optimal evaluation and management of acute scrotal pain and epididymitis in the urgent care setting.
Follow-up
Patients with acute epididymitis do well and the condition typically resolves without sequelae when treated appropriately. Young men with the STD variant of epididymitis can expect rapid improvement in their symptoms in a matter of one to two days, though this rapid improvement occasionally results in treatment non-compliance and recurrences. Rarely, men with inadequately treated epididymitis can develop infertility due to epididymal obstruction as a late complication.This process is analogous to pelvic inflammatory disease in women.
Patients should be seen back in the office in two weeks, at which time compliance is assessed and follow-up cultures are performed. After this, patients can be seen on a PRN basis.
Pediatric patients with epididymitis should be referred to a urologist or, if available, a pediatric urologist for follow-up.
Older men with the E coli-induced epididymitis, likewise, do very well after antimicrobial therapy. Patients should be followed up in two to three weeks to see if their pain has resolved. In addition, patients are instructed to call sooner if their symptoms do not improve or get worse. Some cases of epididymitis are associated with reactive hydroceles, as previously mentioned; the hydroceles often take several weeks to months to resolve, if they resolve at all. Men with large persistent reactive hydroceles can be referred to a urologist for counseling and, if the hydrocele causes the man bother, surgical correction.
Lastly, some men develop a persistent nonspecific scrotal or epididymal pain after an episode of epididymitis. The etiology of this pain is unclear, but infection with standard uropathogens is unlikely. Men who complain of this type of complication are best referred to a urologist for evaluation and management that can include trials of NSAIDs, low-dose tricyclic antidepressants, and alpha-blocker therapy, among others.
Summary
Epididymitis is common and affects all ages without race predilection. Affected patients will have scrotal pain of varying severity and associated findings. After a thorough history and physical exam, adjunctive tests such as the UA and the scrotal sonogram may aid in the diagnosis. In young men, epididymitis is generally caused by GC or Chlamydia and is thus an STD. In older men, epididymitis is typically caused by E coli and is thus a UTI. Boys with epididymitis are also viewed as having UTIs and are to be managed as such. When treated appropriately, epididymitis resolves without sequelae in the majority of men.
REFERENCES
1. Berger RE, Alexander ER, Harnisch JP, et al. Etiology, manifestations, and therapy of acute epididymitis: prospective study of 50 cases. J Urol. 1979;121:750-754.
2. Hoosen AA, O’Farrell N, van den Ende J. Microbiology of acute epididymitis in developing communities. Genitourin Med. 1993;69:361-363.
3. Allen FJ, de Kock ML. Genito-urinary tuberculosis—experience with 52 urology inpatients. A Afr Med J. 1993;83:903-907.
4. Docimo SG, Rukstalis DB, Rukstalis MR, et al. Candida epididymitis: newly recognized opportunistic epididymal infection. Urology. 1993;41:280-282.
5. Hood SV, Bell D, McVey R, et al. Prostatitis and epididymo-orchitis due to Aspergillus fumigatus in a patient with AIDS. Clin Infect Dis. 1998;26:229-231.
6. Sohail MR, Andrews PE, Blair JE. Coccidioidomycosis of the male genital tract. J Urol. 2005;173:1978-1982.
7. Choong CS, Liew KL, Liu PN, et al. Acute scrotum in Henoch-Schönlein purpura. Zhonghua Yi Xue Za Zhi (Taipei). 2000;63:577-580.
8. Gabal-Shehab LL, Monga M. Recurrent bilateral amiodarone induced epididymitis. J Urol. 1999;161:921.
9. Alves LS, Assis BP, Rezende MM. Schistosomal epididymitis. Int Braz J Urol. 2004;30:413-415.
10. Luzzi GA, O’Brian TS. Acute epididymitis. BJU International. 2001;87:747-755.
11. Nickel JC, Shoskes D, Wang Y, et al. How does the pre-massage and post-massage 2-glass test compare to the Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006;176:119-124.
12. Noguchi Y, Kanyama A, Fujita M, et al. [Evaluation of the new nucleic acid amplification system for direct detection of Chlamydia trachomatis and Neisseria gonorrhoeae in women.] Kansenshogaku Zasshi. 2006;80:251-256.
13. Koenig MG, Kosha SL, Doty BL, et al. Direct comparison of the BD ProbeTec ET system with in-house LightCycler PCR assays for detection of Chlamydia trachomatis and Neisseria gonorrhoeae from clinical specimens. J Clin Microbiol. 2004;42:5751-5756.
14. Gaydos CA, Theodore M, Dalesio N, et al. Comparison of three nucleic acid amplification tests for detection of Chlamydia trachomatis in urine specimens. J Clin Microbiol.
2004;42:3041-3045.
15. Connolly SS, D’Arcy FT, Gough N, et al. Carefully selected intratesticular lesions can be safely managed with serial ultrasonography. BJU Int. 2006;98:1005-1007.
16. Akin EA, Khati NJ, Hill MC. Ultrasound of the scrotum. Ultrasound Q. 2004;20:181-200.
17. Lerner RM, Mevorach RA, Hulbert WC, et al. Color Doppler US in the evaluation of acute
scrotal disease. Radiology. 1990;176:355-358.
18. Takahashi N, Ishihara K, Kimizuka R, et al. The effects of tetracycline, minocycline, doxycycline and ofloxacin on Prevotella intermedia biofilm. Oral Microbiol Immunol. 2006;21:366-371.
19. Murillo O, Domenech A, Garcia A, et al. Efficacy of high doses of levofloxacin in experimental foreign-body infection by methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother. 2006;50:4011-4017. Epub 2006 Oct 2.
20.Saito I, Suzuki A, Saiko Y, et al. Acute nongonococcal epididymitis—pharmacological and therapeutic aspects of levofloxacin. Hinyokika Kiyo. 1992;38:623-628.
21. Blondin C, Costa P, Bressolle F, et al. [Diffusion of norfloxacin in epididymal tissue] Pathol Biol. 1991;39:520-523.
22. Melekos MD, Asbach HW. Epididymitis: aspects concerning etiology and treatment. J Urol. 1987;138:83-86.