Published on
Download the article PDF: Ruptured Baker Cyst Is An Uncommon Complication Of A Common Diagnosis A Case Report
Urgent Message: Rupture of a Baker cyst is a rare complication and may manifest with the classic crescent sign of ecchymosis and swelling over the medial malleolus. Given the similarities in presentation to acute deep vein thrombosis, it is essential for urgent care clinicians to be able to differentiate between these diagnoses.
Caroline S. Mifsud, DO, MS; Jennifer Ganzhorn, MD; Michael B. Weinstock, MD; Gregory M. Garrison, MD, MS, FAAFP; Elizabeth Westby, MD
Keywords: Baker Cyst, Ruptured Baker Cyst, Pseudothrombophlebitis, Deep Vein Thrombosis
Abstract
Introduction: Unilateral leg swelling is commonly observed in clinical practice and can arise from various conditions. While some causes may be benign and self-limiting, others can pose significant health risks and may require urgent evaluation and management.
Clinical Presentation: A 69-year-old male presented with 5 days of unilateral leg swelling with associated pain, warmth, and erythema. His past medical history was notable for osteoarthritis and osteoporosis.
Physical Exam: The physical examination revealed significant calf swelling, ecchymosis and tenderness, as well as a palpable mass in the posterior knee.
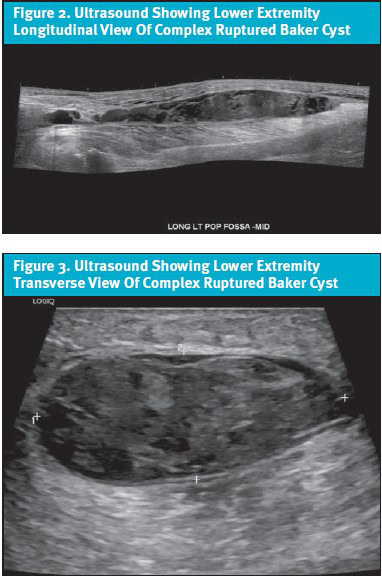
Diagnosis: An ultrasound revealed a 23 x 2 x 5 cm fluid collection in the medial posterior calf, consistent with a large, complex, ruptured Baker cyst, and was negative for acute deep vein thrombosis (DVT).
Case Resolution: The patient was treated with conservative management including rest, ice, elevation, and over-the-counter analgesics and was referred to an orthopedic surgeon for evaluation of surgical management of his osteoarthritis. The patient went on to recover without any further complications.
Conclusion: Unilateral leg swelling requires a broad differential diagnosis. Ultrasound can help distinguish between a ruptured Baker cyst and DVT.
Introduction
Unilateral leg swelling is a frequently encountered complaint among healthcare providers. Quickly distinguishing non-urgent causes, such as Baker cyst, from potentially life-threatening causes, such as deep vein thrombosis (DVT), can be challenging, especially in the ambulatory setting. In this case, our patient presented with unilateral leg swelling, warmth, pain, and erythema and was found to have a ruptured Baker cyst, an uncommon complication of a common diagnosis.
Clinical Scenario
A 69-year-old male presented with 5 days of left-sided unilateral leg swelling with associated warmth, erythema, pain, and difficulty with ambulation. He also endorsed left ankle tenderness and swelling, which developed shortly after the unilateral leg pain. He denied any recent injury, trauma, dyspnea, hemoptysis, or history of blood clots. He denied concerns for fever, cuts, or breaks in the skin. He was not on anticoagulation therapy. His past medical history was notable for osteoarthritis of the bilateral knees and osteoporosis.
Physical Exam Findings
Vital signs on presentation included a blood pressure of 124/72 mm Hg and a pulse of 73 beats per minute. He was generally well-appearing. Physical exam of the left lower extremity was significant for a swollen, erythematous calf extending to the Achilles tendon that was painful to palpation with 3+ pitting edema to the patella, and ecchymosis of the popliteal region. There was also swelling, ecchymoses, and pain to palpation of the lateral and medial malleoli on exam. A palpable mass was appreciated in the posterior knee. Dorsalis pedis pulses were 2+ bilaterally. The skin appeared well perfused without evidence of cyanosis or ischemia. Strength and sensation were intact. Homans sign was positive.
Medical Decision Making And Outcome
The patient’s symptoms were initially suspicious for a DVT, although other differential diagnoses included tendon rupture, thrombophlebitis, cellulitis, necrotizing soft tissue infection (NSTI), seroma, hematoma, venous insufficiency, fracture, and Baker cyst. Given the patient was afebrile and had no visible wounds or breaks in the skin, cellulitis and NSTI were lower in consideration on the differential.
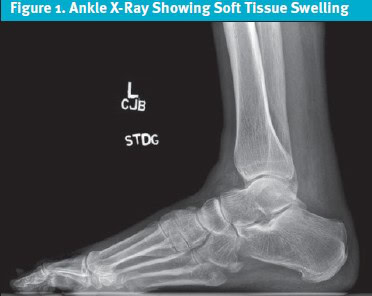
Due to the pain and swelling of the ankle, an ankle x-ray was immediately obtained to rule out fracture or other underlying osseous abnormality. The x-ray showed significant soft tissue swelling but was negative for fracture (Figure 1). The ecchymosis and swelling over the medial malleolus seen on physical exam was consistent with the crescent sign that is characteristic of a ruptured Baker cyst.1-2
Due to concern for DVT, an urgent lower extremity ultrasound was completed, which was negative for acute DVT but did show a 23 x 2 x 5 cm fluid collection in the medial posterior calf consistent with a large, complex, ruptured Baker cyst (Figures 2 and 3). This ultrasound effectively ruled out DVT. Lab studies were not obtained as this would not have changed our management.
Evaluation and Management of Baker Cysts
Baker cysts, also known as popliteal synovial cysts, most commonly form secondary to swelling of the gastrocnemius-semimembranosus bursa in the medial aspect of the popliteal fossa.1-2 This bursa is located between the tendons of the gastrocnemius and semimembranosus muscles, and it communicates with the knee joint capsule. This communication allows for the flow of synovial fluid between these 2 spaces in a valve-like manner.
As age increases, the integrity of the joint capsule decreases, making it more likely for a popliteal cyst to develop. Popliteal cysts rarely occur in isolation and tend to form when an effusion is present, such as in osteoarthritis, rheumatoid arthritis, or knee joint derangements like meniscus or anterior cruciate ligament tears.3 Ruptured Baker cysts are more common in patients with inflammatory conditions, such as rheumatoid arthritis, than degenerative conditions, such as osteoarthritis.3 Popliteal cysts are most commonly asymptomatic but can rupture on rare occasions, resulting in a clinical presentation that is difficult to distinguish from DVT, leading to pseudothrombophlebitis syndrome.1-2 Pseudothrombophlebitis syndrome is a clinical syndrome that mimics the presentation of DVT but is caused by a different underlying condition, most commonly a ruptured Baker cyst. The incidence of Baker cysts ranges from 5-38%; however, the incidence of Baker cyst rupture in particular is not well characterized in the literature.2 Volteas et al. noted that the incidence of Baker cyst rupture is rare in patients with suspected DVT—only 3-4%.4-5
History
Given the similarities in presentation between a ruptured Baker cyst and DVT, it is essential to differentiate between these 2 diagnoses. Inquire about recent injuries or trauma because patients with recent trauma are more likely to have a ruptured Baker cyst as opposed to a DVT. Inquire whether the patient has a history of blood clots or clotting disorders, and whether they are on anticoagulation therapy.
Patients with pulmonary embolism (PE) secondary to a DVT are more likely to present with dyspnea or pleuritic chest pain, whereas patients with a ruptured Baker cyst are unlikely to have these symptoms. Calculating the Wells Criteria for DVT can be particularly useful. For patients with a low pretest probability of DVT, a normal high-sensitivity D-dimer safely excludes DVT, and no further imaging is required. For patients with a high pretest probability of DVT, there is little utility in obtaining a D-dimer, and the clinician should proceed directly to ultrasound.6-8 Patients with a ruptured Baker cyst are more likely to report a history of arthritis, whether degenerative or inflammatory, as well as a possible history of knee injury on the affected side.
Physical Exam
One of the classic findings of a ruptured Baker cyst is the crescent sign, characterized by ecchymosis and swelling over the medial malleolus, which results from fluid in the calf gravitating toward the ankle. In fact, the crescent sign is one of the only ways a ruptured Baker cyst can be distinguished from a DVT.1 Homans sign, or calf pain with passive dorsiflexion of the foot, can be positive in both ruptured Baker cyst and DVT, and is a nonspecific finding.2 Inspection for cuts or breaks in the skin helps to increase suspicion for an underlying infection. Assessment of distal pulses ensures there is no arterial embolism.
Imaging
The most useful imaging modalities for diagnosing a Baker cyst are ultrasound or magnetic resonance imaging (MRI).1,3,5 However, ultrasound is preferred over MRI due to its cost-effectiveness, ease of use, absence of radiation exposure, and greater availability. The main disadvantage of ultrasound is its user-dependence.9 On ultrasound, a Baker cyst can be visualized as a well-defined, unilocular collection of fluid located between the tendons of the medial head of the gastrocnemius and the semimembranosus muscles.3 Evidence of fluid collection along the intermuscular fascia layers is suggestive of a ruptured Baker cyst in particular.1-2 It should be noted that although ultrasound is not necessary for a diagnosis of Baker cyst, the utility of imaging lies in its ability to rule out more serious diagnoses such as DVT.
While plain radiographs are easy to obtain and readily available, they do not offer significant diagnostic value in the evaluation of Baker cysts. However, they can provide information about conditions that may predispose someone to a ruptured Baker cyst, including osteoarthritis, inflammatory arthritis, or loose bodies.3,9 Previously, arthrography was commonly used to assess Baker cysts; however, this method has fallen out of favor due to its invasiveness and use of ionizing radiation.3,9
Management
The mainstay of treatment for uncomplicated Baker cysts typically includes conservative management for at least 6 weeks, which involves rest, ice, physical therapy focusing on flexibility, and over-the-counter analgesics.9 Intra-articular or intracystic aspiration and corticosteroid injections can be considered to help decrease the size and pain associated with the cyst; however, recurrence remains a possibility. Surgical excision can also be considered, but recurrence rates are notably high. In a paper by Rauschning and Lindgren, they reported that of 46 popliteal cyst excisions performed, cyst recurrence occurred in 63% of cases. Given such high rates of recurrence, they recommended that cyst excision be attempted only in cases where the knee derangement is incurable.10 It is believed that the high level of recurrence stems from the persistence of the original intra-articular pathology that predisposed the individual to develop the cyst in the first place. Thus, the primary goal of surgical intervention should be to address the underlying intra-articular pathology, which should theoretically decrease the recurrence of the Baker cyst.3,9-10 For patients with Baker cyst, monitor and inform the patient about potential complications, such as bleeding and compartment syndrome, especially in those with coagulopathies or those on anticoagulation.
Complications
A handful of cases in the literature have noted rare, life-threatening complications of a ruptured Baker cyst, including compartment syndrome.11-13 Other complications include infection, mass effect, or compression of nearby structures.13 Additional case reports have noted the development of compartment syndrome secondary to bleeding when a ruptured Baker cyst was misdiagnosed as DVT and empirically treated with anticoagulation.14 It is possible to have DVT and pseudothrombophlebitis syndrome simultaneously; however, this is incredibly rare.3 In summary, complications are uncommon; however, patients should receive clear discharge instructions and return precautions, including experiencing fever, worsening pain or swelling, paresthesias, dyspnea, or chest pain.
Discussion
The differential diagnosis for acute unilateral leg swelling is broad, ranging from benign to life-threatening. Baker cyst is a common diagnosis, but rupture is an uncommon complication that may mimic a DVT, causing pseudothrombophlebitis syndrome. Although the initial presentation of this patient raised suspicion for DVT, misdiagnosis can lead to ineffective treatment and expose the patient to unnecessary risks. A ruptured Baker cyst mimics DVT and should be distinguished using imaging techniques like ultrasound or MRI.5 Ultrasound is preferred due to its lower cost and availability. Baker cysts, whether ruptured or not, should initially be managed conservatively. Surgical intervention may be considered if the patient shows no improvement after about 6 weeks, or sooner if neurovascular compromise is evident.9
Clinical Scenario Conclusion
This patient presented with the classic finding of crescent sign, which guided us toward a diagnosis of ruptured Baker cyst. Other clinical findings that favor a diagnosis of Baker cyst rather than DVT include knee pain and swelling, and co-existing degenerative arthritis, such as osteoarthritis. Homans sign, or calf pain with passive dorsiflexion of the foot, can be positive in both ruptured Baker cyst and DVT and therefore is a nonspecific finding.2
The patient was treated with conservative management, including rest, ice, elevation, and over-the-counter analgesics. A sports medicine specialist was consulted, who recommended against aspiration and corticosteroid injection due to the increased risk of infection and high recurrence rates. Given the patient’s concurrent osteoarthritis, he was referred to an orthopedic surgeon for evaluation of surgical management. The patient went on to recover without any further complications.
Ethics Statement
The patient provided written consent for the publication of this case and associated figures. Some details of the case were changed to protect patient anonymity and confidentiality.
Takeaway Points
- Consider a broad differential diagnosis in the patient presenting with unilateral leg swelling.
- Rupture is a rare complication of Baker cyst and may manifest with the classic crescent sign of ecchymosis and swelling over the medial malleolus.
- Ruptured Baker cyst should be distinguished from DVT by imaging with ultrasound.
- Baker cysts should initially be managed conservatively for at least 6 weeks. If there is no improvement, surgical intervention may be considered.
Manuscript submitted May 2, 2025; accepted May 27, 2025.
References
- Mizumoto J. The Crescent Sign of Ruptured Baker’s Cyst. J Gen Family Med. 2019;20(5):215-216. doi:10.1002/jgf2.261
- Bansal K, Gupta A. Ruptured Baker’s Cyst: A Diagnostic Dilemma. Cureus. Published online October 5, 2021. doi:10.7759/cureus.18501
- Herman AM, Marzo JM. Popliteal cysts: a current review. Orthopedics. 2014;37(8):e678-684. doi:10.3928/01477447-20140728-52
- Volteas SK, Labropoulos N, Leon M, Kalodiki E, Nicolaides AN. Incidence of ruptured Baker’s cyst among patients with symptoms of deep vein thrombosis. Br J Surg. 1997;84(3):342. doi:10.1046/j.1365-2168.1997.02423.x
- Kim JS, Lim SH, Hong BY, Park SY. Ruptured Popliteal Cyst Diagnosed by Ultrasound Before Evaluation for Deep Vein Thrombosis. Ann Rehabil Med. 2014;38(6):843-846. doi:10.5535/arm.2014.38.6.843
- Wells PS, Hirsh J, Anderson DR, et al. Accuracy of clinical assessment of deep-vein thrombosis. The Lancet. 1995;345(8961):1326-1330. doi:10.1016/S0140-6736(95)92535-X
- Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. The Lancet. 1997;350(9094):1795-1798. doi:10.1016/S0140-6736(97)08140-3
- Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-Dimer in the Diagnosis of Suspected Deep-Vein Thrombosis. N Engl J Med. 2003;349(13):1227-1235. doi:10.1056/NEJMoa023153
- Frush TJ, Noyes FR. Baker’s Cyst: Diagnostic and Surgical Considerations: A Multidisciplinary Approach. Sports Health. 2015;7(4):359-365. doi:10.1177/1941738113520130
- Rauschning W, Lindgren PG. Popliteal cysts (Baker’s Cysts) in adults: I. Clinical and Roentgenological Results of Operative Excision. Acta Orthop Scand. 1979;50(5):583-591. doi:10.3109/17453677908989808
- Schimizzi AL, Jamali AA, Herbst KD, Pedowitz RA. Acute Compartment Syndrome Due to Ruptured Baker Cyst after Nonsurgical Management of an Anterior Cruciate Ligament Tear: A Case Report. Am J Sports Med. 2006;34(4):657-660. doi:10.1177/0363546505284184
- Hamlet M, Galanopoulos I, Mahale A, Ashwood N. Ruptured Baker’s cyst with compartment syndrome: an extremely unusual complication. BMJ Case Reports. Published online December 20, 2012:bcr2012007901. doi:10.1136/bcr-2012-007901
- Erkus S, Soyarslan M, Kose O, Kalenderer O. Compartment syndrome secondary to Baker’s cyst rupture: A case report and up-to-date review. Int J Crit Illn Inj Sci. 2019;9(2):82. doi:10.4103/IJCIIS.IJCIIS_84_18
- Dunlop D, Parker PJ, Keating JF. Ruptured Baker’s cyst causing posterior compartment syndrome. Injury. 1997;28(8):561-562. doi:10.1016/S0020-1383(97)00105-8
Author Affiliations: Caroline S. Mifsud, DO, MS, Mayo Clinic, Rochester, Minnesota. Jennifer Ganzhorn, MD, Adena Health System. Michael B. Weinstock, MD, Adena Health System; Wexner Medical Center at The Ohio State University, The Journal of Urgent Care Medicine. Gregory M. Garrison, MD, Mayo Clinic, Rochester, Minnesota. Elizabeth Westby, MD, Mayo Clinic, Rochester, Minnesota. Authors have no relevant financial relationships with any ineligible companies.
Read More JUCM Articles Pertaining to this Subject
- Urgent Care Diagnosis and Management of Deep Vein Thrombosis
- Utility of POCUS in Skin and Soft Tissue Infection
- Evaluation of Knee Pain: An Urgent Care Approach

