Urgent message: Knee pain is a diagnostic challenge for urgent care providers, but a strong understanding of the anatomy and potential etiologies will prepare them for success.
CHRISTOPHER TANGEN, DO
Approximately 10% of all urgent care visits are for musculoskeletal complaints and knee pain is a common such presentation. An urgent care provider’s approach is different than that of specialists because patients present with more acute cases, and therefore, the physician needs to consider a vast differential and rule out limb threatening conditions. These encounters often yield suboptimal exams, and referral to sports medicine or orthopedic surgery. This article serves as a template for urgent care providers on how to evaluate knee pain.
Introduction
The knee is the largest hinge joint in the body and houses the largest articular cartilage surface area, as well as four stabilizing ligaments and many muscles and neurovascular structures. Knee pain is one of the most common musculoskeletal complaints, especially in the younger, athletic population because of overuse syndromes, high energy injuries, and relatively weak growth plates. Seniors often experience knee pain associated with chronic conditions such as osteoarthritis. This article represents a protocol that urgent care providers should follow for all encounters in which a patient presents with knee pain.
History of Knee Pain
Obtaining a good history is the first step toward working on a solid differential diagnosis.
Onset: Acute vs Chronic. The timing and mechanism of pain are arguably the most important pieces of the his- tory. Anterior cruciate ligament (ACL) injuries are almost always traumatic and most commonly due to indirect forces, such as coming down from a layup or an abrupt stop in skiing. Patellofemoral pain syndrome is usually insidious and worsened with walking up and down stairs and sitting for a prolonged period of time. Prior/Palliation/Provocation/Progression. Many seniors with osteoarthritis of the knee can easily identify exacerbations in their knee pain. Very often patients will present with their “typical” pain and swelling after a long day on their feet, or a busy day of running errands. Relief with ice and compression can lead to identification of swelling in the history, and worsening with specific motion points to tendonitis or muscle injuries. Most knee pain improves with time and rest, but worsening pain in spite of rest brings rheumatologic and infectious etiologies into consideration.
Quality. “Aching” anterior knee pain is often patellar in origin. A “pop” is worrisome for a torn ligament. “Clicking” can either be patellar or meniscal.
Radiation. Radiation of pain should lead an urgent care provider to be further concerned about nonknee etiologies, such as the hip or radicular generators of knee pain.
Severity. An ACL tear initially produces severe pain, which dissipates greatly within the first hour. Patellar tendonitis, in contrast, can be mildly painful all day long.
Knee Exam
After a focused history is obtained, a sound physical exam will lead the urgent care provider to a diagnosis in the vast majority of cases.
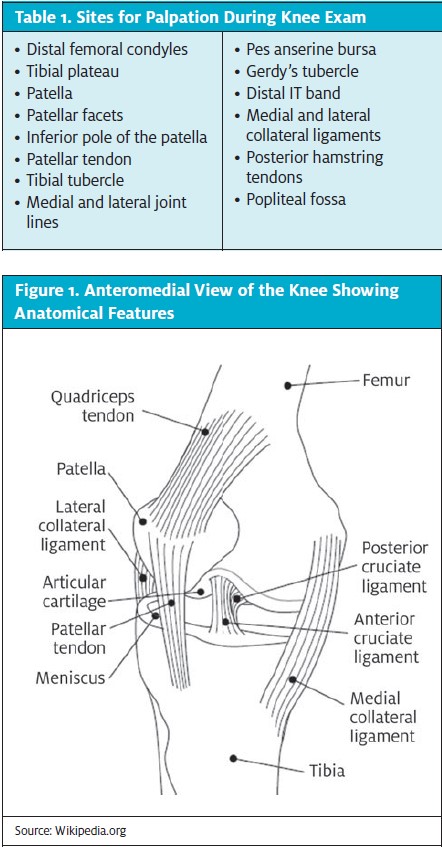
Inspection and palpation. Alignment and redness or skin color changes should be noted with inspection. Improper alignment often indicates patellofemoral etiologies, whereas discoloration can be seen with infection, gout, and hemarthrosis. Soft tissue swelling, bursitis, and effusions are differentiated with palpation. A large effusion from a fracture or intraarticular tear can complicate an exam and make subtle test findings difficult to differentiate. Table 1 lists the landmarks that should be palpated on every knee exam, some of which are also shown in Figure 1.
Range of Motion. The hinged knee joint has an arch of approximately 0 to 130 degrees. Clearly, pain-free range of motion (ROM) is ideal, but ROM from 0 to 110 degrees is functionally desirable in the acute setting. ROM should also be tested in the hip because hip pathologies can present as knee pain.
Strength testing. Strength testing is somewhat less important in the urgent care setting because many patients present with acute pain and decreased effort because of this pain, or external factors. Testing resisted flexion and resisted extension strength in the knee is important because weakness in flexion or the inability to extend fully can indicate a hamstring tear or patellar tendon rupture, respectively. Subtleties in muscle strength testing discrepancies can be further evaluated during followup.
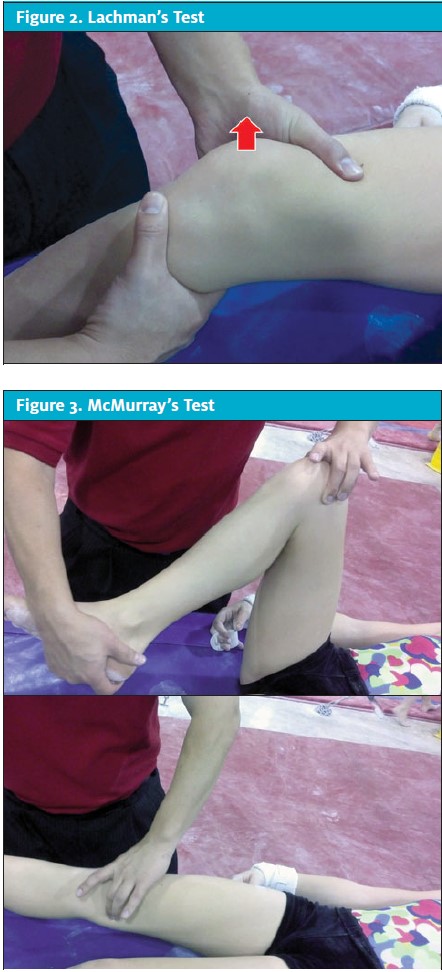
Stability tests. The four stabilizing ligaments in the knee are the ACL, posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). The ACL is the most important stabilizing ligament in the knee and, therefore, should be evaluated during every knee exam. The most specific test for ACL injuries in the knee is the Lachman’s test (Figure 2), which is performed with the patient in a supine position and the knee flexed to 30°. The patient’s thigh is stabilized and an anterior translation force is passively applied to the knee. A firm endpoint and little or no translation across the joint line indicates a negative Lachman’s test. A soft endpoint with increased translation is a positive Lachman’s test.
The medial collateral ligament is very commonly injured with a valgus force to the knee. Patients with this presentation will often feel pain when the clinician performs a passive valgus stress to the affected knee. What is most important, however, is that the pain is not increased compared to the contralateral knee. With severe MCL injuries, recovery may be prolonged.
The PCL and LCL are less commonly injured ligaments in the knee. The PCL is best tested with a posterior drawer test, which is done by applying a passive posterior translation force to the tibia with the patient supine and the knee flexed to 90o. The test is positive when the tibia translates posteriorly in respect to the femur without an endpoint. The LCL is tested the same fashion as the MCL, but with a varus stress to the knee. (no, the MCL and LCL are tested with different stresses).
Special tests. The McMurray’s test is the test most commonly performed when evaluating for a potential meniscal tear in the knee (Figure 3). A positive McMurray’s test includes a palpable click at the medial or lateral joint line as well as pain. Very often, patients will have pain and a click with McMurray’s testing, but the click usually originates at the patella and not the joint line. Apply’s compression test can also be used to evaluate a potential meniscal injury. With the patient prone and the knee flexed to 90o, force is applied through the heel to the knee with internal and external rotation. Other exam. A thorough neurovascular exam should always be performed on patients with knee pain. Functional testing such as balance testing and gait evaluation should also be considered, especially during evaluations for return to work or sports.
Common Injuries and Common Causes of Pain
Although most knee injuries are acute, it is not uncommon to evaluate a patient with chronic knee pain or over- use injuries.
Patella. Patellofemoral pain syndrome is a common reason for anterior knee pain and more common in younger females. Common symptoms include worsening pain with prolonged walking, using the stairs, and prolonged sitting or standing. Patellar subluxation is a common injury in patients who are athletic, and they often actually will notice a pop with a twisting injury during which the knee cap laterally partially dislocates and relocates. Exam findings include pain with patellar apprehension testing and tenderness to palpation over the patellar facets, soft tissue swelling and effusion, and a neg- ative Lachman’s test.
Ligament. As mentioned above the ACL, MCL, PCL, and LCL are the main ligaments in the knee. MCL (7% of knee injuries) and ACL (4%) injuries are more common than PCL or LCL injuries. Most ACL injuries are caused by indirect (approximately 75%) forces to the knee and are accompanied by acute pain and immediate knee effusion. ACL tears are often treated with physical therapy before and after reconstructive surgery.
Posteriolateral corner or fibular head dysfunction injuries are less common disruptions in knee stability. These injuries are difficult to diagnose, but a dial test can be performed to determine whether there is lateral instability. With the patient in a supine position and the hip flexed to 90° and the knee flexed to 90°, passive external rotation forces are applied to the lower leg and compared to the contralateral side.
Tendonitis. Tendonitis is a very common injury of the musculotendinous junction, but can be acute or chronic in nature. Common areas for tendonitis include the patellar tendon, distal IT band, quadriceps and hamstrings (pes anserine bursitis relation). Patients with tendonitis usually present with a history of pain with activation of the muscle as well as tenderness to palpation on exam and occasionally decreased muscle strength testing.
Bursitis/Baker’s cyst. Knee bursitis is also a very common cause of pain. The most common locations are the prepatellar bursa (after direct trauma) and the pes anserine bursa (often due to hamstring hypertonicities). A Baker’s cyst can be diagnosed with posterior fullness and soft tissue swelling. Baker’s cysts commonly fill from swelling in the knee caused by osteoarthritis and a ruptured Baker’s cyst can present as calf swelling and can prove to be a diagnostic dilemma, thus warranting a lower-extremity study for deep venous thrombosis.
Bone Fracture. Fractures are also very common around the knee joint. In the pediatric or adolescent population, Salter-Harris fractures, or growth plate fractures, are very common. Avulsion fractures can also occur after an acute injury to the knee. Patellar fractures are sometimes difficult to diagnose because bipartate patella are some- times incidentally found on plain film examinations after a knee contusion. If a femoral or tibial plateau fracture is diagnosed, be sure that the lower extremity is neurovascularly intact, and ensure proper immobilization before orthopedic referral.
Overuse. Very common overuse injuries in the pediatric population include Osgood-Schlatter’s disease, Sinding Larsen Johannsen (SLJ) syndrome, and less commonl osteochondritis dissecans (OCD) lesions. Osgood-Schlatter’s disease usually occurs in patients aged 9 to 14 years who present with anterior knee pain and tibial tubercle soft tissue swelling and tenderness to palpation. SLJ presents in slightly younger patients with anterior knee pain and tenderness to palpation and soft tissue swelling overlying the inferior pole of the patella with radi- ographic findings of apophysitis. An osteochondritis dessicans lesion can develop as a posttraumatic or as an overuse injury with vague pain and intermittent swelling. Plain film examination findings may reveal alucency in the distal femoral condyles, with the lateral aspect of the medial femoral condyle being the most common area affected. OCD lesions are confirmed with magnetic resonance imaging (MRI) and very often require surgery and non-weight-bearing rehab.
Meniscal Injury. The medial and lateral menisci are the two fibrocartilaginous “cushions” in the knee in between the femur and the tibia. The menisci are commonly injured (10% of knee injuries) and torn, which can cause intermittent swelling. Patients usually state that they have locking symptoms in the knee, those with tears usually present with a small joint effusion as well as tenderness to palpation along the joint line and a positive McMurray’s test. Meniscal injuries are more common in adults age 40 and older.
Infections and Arthritis. By far the most common reason for seniors to develop knee pain and swelling is osteoarthritis, which should be kept in mind before necessarily jumping to other conclusions about atraumatic knee swelling. Cellulitis around the knee should be thoroughly evaluated to ensure that there is no effusion or septic arthritis present. If laboratory testing is available, a complete blood count with differential, erythrocyte sedimentation rate, and C reactive proten measurement can be obtained. Aspiration is a way to distinguish between a hemarthrosis, gouty attack, and septic joint. When there is strong suspicion of a septic joint, however, joint aspiration should be performed after consultation with orthopedic). Although knee pain and soft tissue swelling can result from complex medical etiologies such as lupus or rheumatoid arthritis, the urgent care setting is most appropriate for triaging these patients for followup.
Workup in the Urgent Care
Just as with ankle injuries, there are Ottowa rules for obtaining plain films on patients with knee injuries. These are age ≥55, isolated tenderness of the patella, tenderness of the fibular head, inability to flex to 90 degrees, and inability to walk four steps. One perceived benefit of obtaining plain films in the urgent care setting is to assist the specialists in followup. However, most knee injuries do not require plain film examination. MRI is often very helpful for the orthopedic surgeon in followup. As mentioned previously, aspiration of the knee and subsequent pathologic or laboratory analysis can be helpful when differentiating infectious versus rheumatologic etiologies of knee swelling. In cases of knee pain where an open fracture or fracture with neurovascular compromise is suspected, a computed tomography scan is warranted; however, in the vast majority of cases, a history and physical exam coupled with plain film imaging and routine blood work will suffice.
Management
In general the R.I.C.E pneumonic (Rest, Ice, Compression, Elevation) is appropriate for most knee injuries. More substantial evaluation by orthopedic surgery or transfer to the emergency department is warranted, however, in cases of open fractures, knee injuries or fractures with neurovascular compromise, or cases of abuse. Even if a knee injury such as an ACL tear or meniscal tear is confirmed on the physical examination mobilization, pain control and work restrictions or school restrictions are usually sufficient until proper followup has been done.
Limitations and restrictions are also important patient education measures, mostly with work-related injuries or sports injuries. Work restrictions should be recommended by the urgent care provider based on the patient’s functional evaluation and potential for recovery. Sports restrictions should be recommended based upon the athlete’s ability to protect his or her knee in addition and potential for pain-free range of motion and near full strength in the knee.
Immobilization and crutches are commonly prescribed treatments for knee pain. Immobilization with a brace such as a knee immobilizer is NOT recommended for more than 3 days because of the potential for muscle atrophy and range of motion stiffness. Crutches are very helpful in management of acute knee pain as a way to allow the patient to ambulate at work, home, or at school. Casting is not generally done in the urgent care set- ting because there tends to be a large amount of soft tissue swelling after a fracture and casting is best done once much about soft tissue swelling has resolved. There forem proper bracing and splinting is needed in the urgent care setting for nonsurgical fractures.
Knee aspiration can be a very helpful treatment option for prepatellar bursitis or a large knee effusion caused by chronic osteoarthritis or known rheumatoid arthritis. A local steroid injection (ex: 3 mL 1% lidocaine and 20-40 mg kenalog), if not done in the previous 3 months, can be helpful for knee osteoarthritis, pes anserine bursitis, and anterior patellofemoral pain.
Medications are commonly prescribed in the urgent care setting for musculoskeletal injuries. Over-the- counter medications such as acetaminophen (325-1000 mg po every 4-6 hours as needed) or ibuprofen (600-800 mg po every 8 hours as needed) will provide adequate analgesia for most adult patients. Naprosyn and hydrocodone are also commonly prescribed medications for knee pain. Topical analgesia medications such as diclofenac also can be prescribed.
Referrals are commonly made for knee pain from an urgent care setting to a primary care physician, occupational medicine physician, sports medicine physician, or orthopedic surgeon. In general, referrals within 1 week’s time are adequate, but in the case of nonsurgical fractures or sports-related injuries, early followup is better.
Summary
Musculoskeletal complaints are extremely common in the urgent care setting and the knee is one of the most common areas for musculoskeletal pain because it is the largest joint in the body and very commonly injured by individuals of all ages.
A thorough history and physical will lead the urgent care provider to the vast majority of diagnoses, and good management and proper referral will ensure good patient care. In cases in which the diagnosis and exact etiology of a patient’s knee pain are not clearly elucidated, referral to the proper specialist is important. Definitely there are individuals who present with knee pain for reasons such as avoiding work and obtaining pain medications. Such patients should be referred to the proper occupational or pain medicine specialist. ■
Suggested Reading
- Reider The orthopaedic physical exam- 2nd edition. 2005. p. 201-246
- Grover Evaluating Acutely Injured Patients for Internal Derangement of the Knee. Am Fam Phys. 2012;85(3): 247-252.
- Eiff. Fracture Management for Primary Care 2nd edition. 2003. pp 263-287.
