Urgent message: Point-of-care ultrasound (POCUS), just starting to become more prevalent in the urgent care setting, facilitates improved diagnostic and interventional clinical decision-making by aiding the clinician in discerning between cellulitis, abscess, or both.
Chelsea M. Burgin, MD FAAFP and Dustin S. Morrow, MD FACEP
INTRODUCTION
Each year in the United States around 14 million patient encounters present with skin and soft tissue infections (SSTIs). A detailed history and focused exam differentiate between cellulitis and/or abscess the majority of the time. However, there are scenarios when it is challenging to distinguish among cellulitis, an abscess, or a combination of the two. POCUS has been shown to reduce clinician uncertainty in treatment for SSTIs while altering management up to half of the time.1-5
BACKGROUND
While use of POCUS is on the rise in urgent care centers, emergency medicine physicians have incorporated the use of bedside ultrasound for the detection of abscesses in SSTIs for the past two decades (though perhaps considerably less time in nonteaching community hospitals).6-8 POCUS has been found to have a sensitivity of 91.1%─96.2% with a specificity of 76.9%─82.9%3,9 for the identification of an abscess, compared to physical exam alone. The POCUS application for SSTI is favorable to patient outcomes as it improves diagnostic accuracy for ruling in abscess while reducing unnecessary incision and drainage when abscess is ruled out.
DISCUSSION
POCUS is an emerging technology that can advance the urgent care clinician’s management of SSTIs. The application of soft tissue ultrasound for infection requires elementary skills that are easy to learn and apply in practice when used to distinguishing abscess from cellulitis. Even a clinician who is a novice in the use of POCUS may readily differentiate tissue edema (cellulitis) from a pocket of fluid (abscess) on ultrasound image after minimal training under good mentorship for quality assurance.10
Accurately identifying the presence or absence of an abscess has significant treatment implications. Cellulitis proves clear indication for antimicrobial therapy, whereas an abscess requires incision and drainage.
A practice-altering meta-analysis published in the BMJ in 2018 provides patient-centered guidelines after thorough review of the role of antimicrobials for simple abscesses. Complicated SSTIs with systemic signs, deep tissue infection, or hidradenitis suppurativa were not considered in these guidelines. High-quality evidence recommendations highlighted the use of TMP-SMX or clindamycin for simple abscess in addition to incision and drainage based on the findings of a 5% absolute reduction risk of SSTI treatment failure at 1 month and an 8% absolute reduction risk of reoccurrence at 3 months.
In contrast to control patients not treated with antimicrobials, an additional (high-quality evidence) finding reported clindamycin had a 10% higher risk of diarrhea, while (moderate-quality evidence) TMP-SMX was found to have a 2% higher risk of nausea. Due to the high prevalence of MRSA (49%─88%) and failed treatment, the recommendation (moderate-quality evidence) was made against the use of early and later generation cephalosporins compared to TMP-SMX or clindamycin.11
In addition to these guidelines, local prevalence of resistant bacteria and MSSA need also be considered.
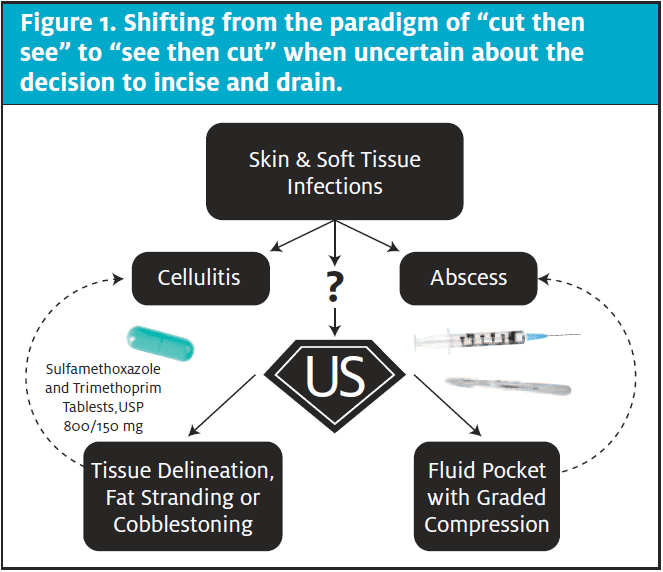
In acknowledgement of the aforementioned clinical guidelines, the role of POCUS is not to determine the presence or absence of benefit from pharmacotherapy. Rather, the role of POCUS is to clarify in the clinical decision-making process whether or not the addition of surgical intervention is of medical necessity. It is time for urgent care clinicians to advance from a cut then see approach to one of see then cut. Answering this question accurately is arguably the most invaluable in the pediatric population affected by SSTI. POCUS may assist in the avoidance of unnecessary consternation for both patient and parent often accompanying a procedure.
Another opportunity to highlight the indication for POCUS is when initial treatment fails by antimicrobial therapy alone. It is important to appreciate how SSTIs exist on somewhat of a spectrum. Over time, cellulitis may progress from soft tissue edema into more focal fluid collection(s) like an abscess. The diagnosis of cellulitis by physical exam alone or with the addition of POCUS merits clear education from the clinician to the patient or guardian as worsening pain, swelling, or erythema may imply treatment failure or the development of an abscess—at which point re-evaluation would be imperative.
NORMAL SKIN AND SOFT TISSUE
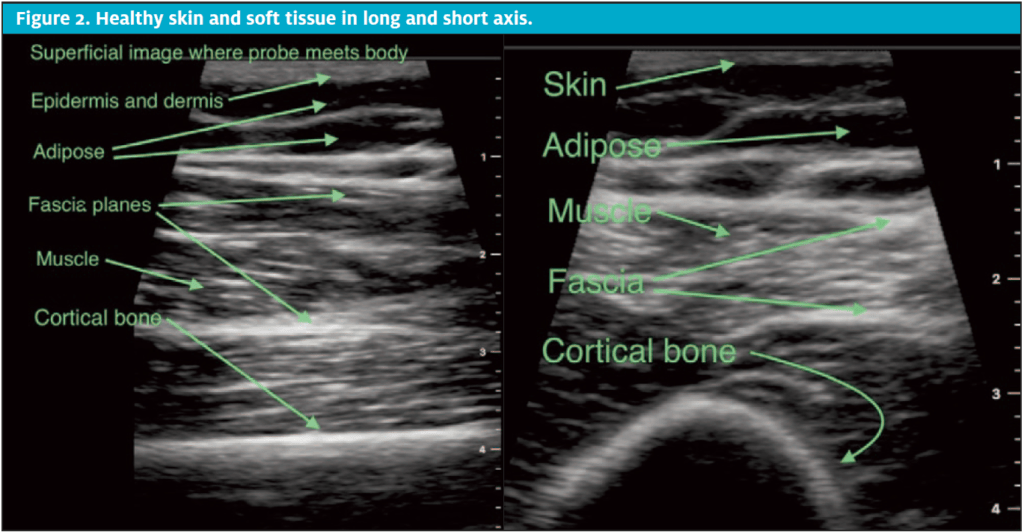
The inter-lumen blood-filled space of arteries and veins are anechoic (the ultrasound term to describe a fluid state). This lack of color is the result of absorbed sound waves and a lack of echo wave production. Many soft tissue structures have varying densities in more of the gray scale, such as adipose and muscle. These have hypoechoic tendencies on ultrasound image, typically more gray than black. On the other extreme of the grayscale, dense structures such as fascia and cortical bone create echo waves, sound waves that come in contact with the structure and bounce back to the probe triggering bright white or hyperechoic markings on the ultrasound image. Differentiating hypoechoic soft tissue by pattern recognition is key.
Moving from superficial to deeper structures, ultrasound characteristics on healthy skin and soft tissue layers are as follows: the epidermis and dermis are hyperechoic and typically thin crowded at the top of an ultrasound image by the gel-probe interface. The subcutaneous adipose also has significant variability in thickness depending body habitus. On ultrasound, adipose is hypoechoic (dark gray to near black) in the subcutaneous regions, appearing like a tight connection of overlapping oblique ovoid structures outlined by fine hyperechoic lines (bright lines of inter-adipose connective tissue). Under the adipose layer, there are fascial planes and muscle tissue which in long axis are fibrous and in short axis appear like prime filet mignon. Muscle sits just superficial to hyperechoic cortical bone. Due to the nature of bone and how it reflects sound waves, there are reliable shadow patterns deep to bone on any ultrasound image on.
CELLULITIS
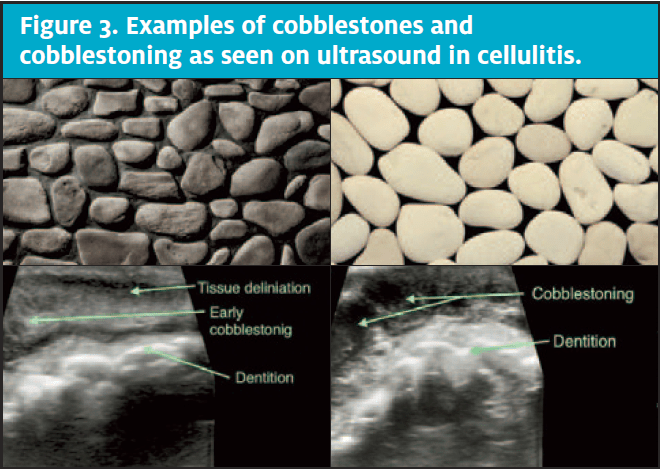
Early cellulitis on ultrasound appears as a mere delineation or blurring of previously sharp borders of normal soft tissue planes; this is often best determined by evaluating an unaffected area on the patient and comparing it to the affected area. This can easily be done by scanning proximal or distal to the area of concern or by scanning the same region on the contralateral side. Unaffected skin and soft tissue has distinct patterns.
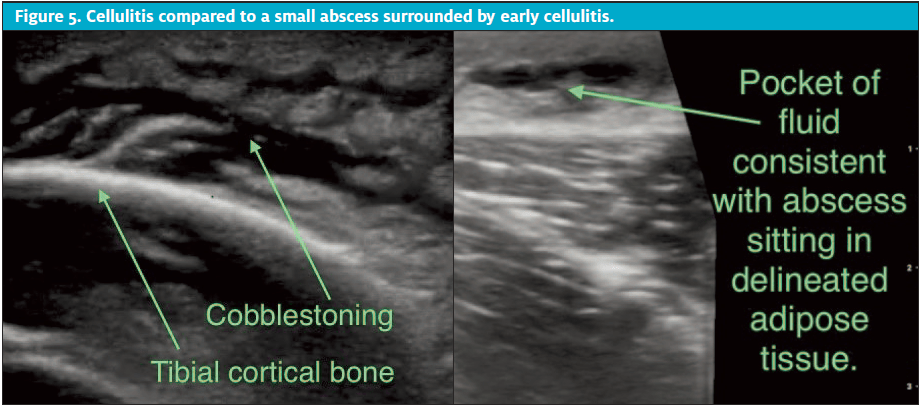
On the infection continuum, cellulitis transitions from delineation into more fat stranding and then into mature cellulitis which appears as edema in the interstitial space between adipocytes. Mature cellulitis has a classic cobblestone appearance. As in the images of cobblestones below, note that the more hyperechoic round globules of subcutaneous adipose are separated by a slightly irregular lattice of anechoic or hypoechoic fluid.
Cobblestoning is not pathognomonic for cellulitis. Masqueraders of cellulitis on ultrasound include local allergic reactions or CHF-related edema; all three present with cobblestoning. POCUS is most helpful when used as an adjunct to the patient history and physical exam.
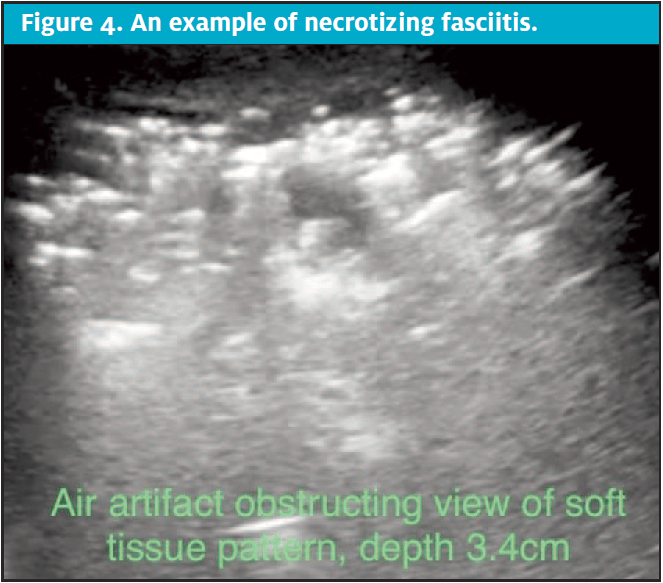
Necrotizing fasciitis is an alarming, rapidly progressive disease process that needs to be quickly evaluated for when history and physical exam raise the concern. Aligning with crepitus on palpation of the affected skin and soft tissue, subcutaneous air can be seen on ultrasound. Air is a nightmare for sound wave imaging on all applications with the exception of lung, particularly if emphysematous tissue is suspected. In SSTI, timely transfer reduces morbidity and mortality.12,13
ABSCESS
On ultrasound, an abscess is a greater consolidated collection of hypoechoic fluid. In comparison to cellulitis which appears to have small avenues of interstitial fluid in network, an abscess is the result of potential fluid coalescence into a greater volume found typically within the loose connective tissue layer of subcutaneous adipose. Abscess contents such as purulent matter with swirling debris and loculation can be seen on ultrasound.
Graded compression is one technique of probe manipulation used to differentiate an abscess from one of its lookalikes. It is achieved by intermittently delivering significant pressure through the probe over the area of concern, evaluating for compressibility. Soft tissue edema does not “squish” whereas a pocket of fluid does.
SPECIAL CONSIDERATIONS
As noted, POCUS is excellent at discerning a pocket of fluid from tissue edema; however, a diligent urgent care clinician utilizing POCUS will remain alert to keep these key points in mind:
- Cellulitis; does the clinical context support infection, local swelling from an allergic reaction, or more diffuse swelling as seen in CHF or low serum protein disorders?
- Does the clinical context and POCUS exam provide evidence for an abscess? Cyst? Hematoma? Herniated bowel? Lymph node? Pseudoaneurysm?
- Does the ultrasound image look strange or like a nighttime picture without flash of a field glowing with fireflies? Think necrotizing fasciitis. Call the surgeon.
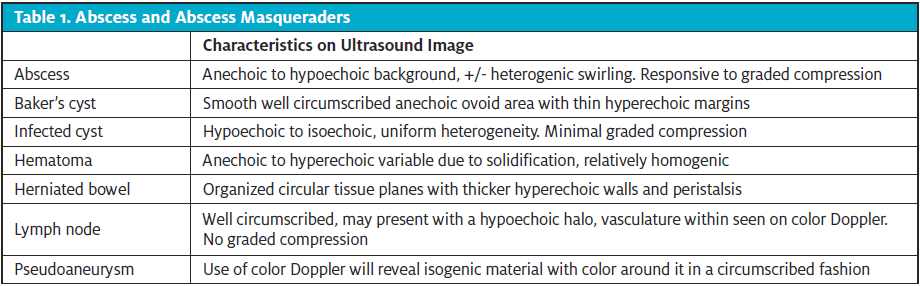
To avoid deception from SSTI masqueraders, be cognizant of a full differential and then place ultrasound examination findings in clinical context. For example, POCUS would not differentiate cellulitis from local swelling after a bee sting or spider bite, both present as soft tissue edema with mature findings of cobblestoning. An appropriate question to answer with POCUS in the context of a bite or sting would be, Is there a pocket of fluid accumulating within the tissue edema?
APPLICATION GUIDELINES FOR SSTI IMAGE AQUISITION
- Record 6-second video clips sweeping the board side of the probe over the affected area, at least twice, the second, 90 degrees from the first, typically in long and short axis relative to muscle and bone beneath. Remember, one view is no view.
- With the point of interest centered in the image, provide graded compression to test for compressibility and swirling debris; capture this in a brief clip.
- Turn on color Doppler and record a final clip to assess for embedded and adjacent vasculature. Do not compress the probe for this clip, as veins easily compress and can be obliterated from the image.
- Consider a static image where calipers can be used to measure depth below the surface, as well height and length.
- Take time to label clips and images for future reference and quality assurance; this is a billable procedure.
- If needed for comparison, and especially helpful in early SSTI, scan normal-appearing skin and soft tissue over the same region on the contralateral side.
CONCLUSION
The application of SSTI ultrasound to identify and discern a pocket of fluid from tissue edema is well supported in the medical literature. As a first-line clinician, the urgent care provider can utilize POCUS to refine medical decision-making and advance patient care. It is important to keep SSTI POCUS within its evidence-based medicine scope of practice; for example, ultrasound of local swelling from a bee sting or spider bite will not distinguish allergic from infective tissue edema but is effective at determining if a pocket of fluid or abscess has developed. Implementing POCUS as a tool will guide a prudent clinician in their delivery of excellent patient centered care.
Burgin CM, Morrow DS. Utility of POCUS in skin and soft tissue infection. J Urgent Care Med. June 2020. Available at: https://www.jucm.com/utility-of-pocus-in-skin-and-soft-tissue-infection/.
References
- Lam SHF, Sivitz A, Alade K, et al. Comparison of ultrasound guidance vs. clinical assessment alone for management of pediatric skin and soft tissue infections. J Emerg Med. 2018;55(5):693-701.
- Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care ultrasound for diagnosis of abscess in skin and soft tissue infections. Acad Emerg Med. 2017;70(4):580-582.
- Barbic D, Chenkin J, Cho DD, et al. In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis. BMJ Open. 2017;7(1):e013688.
- Iverson K, Haritos D, Thomas R, Kannikeswaran N. The effect of bedside ultrasound on diagnosis and management of soft tissue infections in a pediatric ED. Am J Emerg Med. 2012;30(8):1347-1351.
- Marin JR, Dean AJ, Bilker WB, et al. Emergency Ultrasound-assisted examination of skin and soft tissue infections in the pediatric emergency department. 2013;20(6):545-553.
- Squire BT, Fox JC, Anderson C. Abscess: applied bedside sonography for convenient evaluation of superficial soft tissue infections. Acad Emerg Med. 2005;12(7):601-606.
- Tayal VS, Hasan N, Norton HJ, Tomaszewski CA. The effect of soft-tissue ultrasound on the management of cellulitis in the emergency department. Acad Emerg Med. 2006;13(4):384-388.
- Ramirez-Schrempp D, Dorfman D, Baker W, Liteplo A. Ultrasound soft tissue applications in the pediatric emergency department: to drain or not to drain? Pediatr Emerg Care. 2009;25(1):44-48.
- Gottlieb M, Avila J, Chottiner M, Peksa GD. Point-of-care ultrasonography for the diagnosis of skin and soft tissue abscesses: a systematic review and meta-analysis. Ann Emerg Med. February 17, 2020. [Epub ahead of print]
- Marin JR, Alperin ER, Panebianco NL, Dean A. Assessment of training curriculum for emergency ultrasound for pediatric soft tissue infections. Acad Emerg Med. 2011:18(2);174-182.
- Vermandere M, Aertgeerts B, Agoritsas T, et al. Antibiotics after incision and drainage for uncomplicated skin abscesses: a clinical practice guideline. BJM. 2018;360:k243.
- Testa A, Giannuzzi R, De Biasio V. Case report: role of bedside ultrasonography in early diagnosis of myonecrosis rapidly developed in deep soft tissue infections. J Ultrasound. 2015;19(3):217-21.
- O’Rourke K, Kibbee N, Stubbs A. Ultrasound for the evaluation of skin and soft tissue infections. Mo Med. 2015;112(3):202-205.
Chelsea M. Burgin, MD FAAFP is the Medical Director of Boiling Springs MD360 Convenient Care and Director of MD360 Ultrasound, Prisma Health and Assistant Clinical Professor, University of South Carolina School of Medicine Greenville. Dustin S. Morrow, MD FACEP is POCUS Enterprise Director, Prisma Health – Upstate; Division Chief of Emergency Ultrasound, Department of Emergency Medicine; Director of Ultrasound Education and Clinical Assistant Professor, University of South Carolina School of Medicine Greenville. The authors have no relevant financial relationships with any commercial interests.


