Urgent message: Though the most common fracture seen in pediatric trauma patients, elbow fractures can be difficult to identify in younger patients. Familiarity with elbow anatomy, ossification centers, and fracture patterns is essential for optimal outcomes.
Amy Grover, MD
CASE VIGNETTE
A 7-year-old previously healthy female presents to urgent care with a chief complaint of left elbow pain after a fall on outstretched arm. She had immediate pain, swelling and difficulty moving her arm. Her examination is notable for marked left elbow swelling and diffuse elbow tenderness. She has a strong radial pulse, brisk cap refill in her fingers, and can wiggle her fingers easily, but is reluctant to move the rest of her left upper extremity.
BACKGROUND
Elbow fractures are a common injury seen in pediatric urgent care. In a series of more than 15,000 pediatric trauma patients, elbow fractures were the most common fracture (16%).1 Despite the prevalence, the elbow is a location where fractures are frequently missed disproportionately relative to other anatomic locations.2 The cartilaginous nature of the pediatric elbow, along with variability in developmental ossification, make radiographic interpretation challenging. Understanding elbow anatomy, ossification centers, and fracture patterns is essential in caring for and accurately diagnosing pediatric elbow fractures.3
ANATOMY
The elbow joint is comprised of the ulno-humeral and radio-capitellar articulations. It is almost completely nonossified in the newborn period, with ossification centers developing in a predictable pattern over time, demonstrated by the mnemonic CRITOE (capitellum, radial head, internal (medial) epicondyle, trochlea, olecranon, and external (lateral) epicondyle). While there is some individual and gender-based variability, these ossification centers appear at approximately 1, 3, 5, 7, 9, and 11 years of age.4,5 Therefore, if a 5-year-old child has an ossific density in the region of the trochlea, it is likely a fracture fragment and not an ossification center. When there are questions of fractures vs growth centers, contralateral films may be helpful as both elbows tend to ossify similarly.
PHYSICAL EXAM
The physical examination of a child with extremity trauma must include neurologic, vascular, and soft tissue assessment.3
Neurologic assessment of the motor and sensory function of the radial, median and ulnar nerves can be done quickly by asking the patient to demonstrate a “thumbs up“ (radial nerve performs thumb extension); “A-OK” (anterior interosseous nerve flexes the index finger DIP joint and thumb IP joint; be sure they are in flexion to create an O, not just apposed like a pinch); make a fist (median nerve controls finger flexion); and either spread or cross fingers (ulnar nerve).6
Light touch sensation is assessed at the dorsal thenar web space (radial nerve), and the tip of the middle (median nerve) and little (ulnar nerve) fingers. It is crucial not to miss subtle neurovascular deficits preintervention. If the patient has a postintervention nerve palsy and the preintervention exam states “NV Intact” then the injury will be deemed iatrogenic. Over 90% of cases in one series had no documentation of individual nerve examination, and significant nerve injuries were missed.7
Vascular exam includes assessment of radial pulse, as well as finger capillary refill. Doppler assessment can be useful if the pulse is nonpalpable, which is most commonly due to a temporary arterial spasm (though more serious injuries must be ruled out). Early signs of vascular insufficiency include lack of active finger extension, forearm pain with passive finger extension, forearm tenderness or firmness to palpation, and pain out of proportion to injury. These can be present even if the pulse is palpable, as venous and capillary flow are obstructed earlier than major arteries.3,4
There is an increased risk of compartment syndrome with extensive soft tissue injury (swelling, bruising) about the elbow. Any child with concerning findings should be promptly evaluated by an orthopedist and have compartment pressures measured early.3 The skin should be carefully examined to rule out an open fracture. Finally, infection should always be considered on the differential of a swollen joint, especially if the trauma history is vague or nonspecific. If the history is unclear in the presence of a joint effusion, serum inflammatory markers may be helpful. 6
RADIOGRAPHIC EVALUATION
Standard elbow radiographic evaluation includes a true lateral (elbow flexed to 90°), and an anteroposterior (AP) view in full extension. Obtaining true AP and lateral films can be challenging in a child with significant pain and swelling. Pain control prior to imaging can help avoid suboptimal positioning which limits radiographic interpretation. Oblique views can improve diagnostic accuracy for subtle fractures, especially lateral condyle fractures.6
As with all radiographic interpretation, having a systematic evaluation process can help diagnostic accuracy. Evaluation should include assessment of the anterior humeral line, radio-capitellar joint alignment, and the fat pads.
In a lateral projection, the anterior humeral line (drawn along anterior cortex of the humerus) should intersect the middle third of the capitellum, though oblique projections and the small size of the capitellum in patients younger than 5 years of age can make interpretation difficult.5 The radio-capitellar line should intersect from the middle of the radial shaft through the middle third of the capitellum. The sail sign is caused by an intra-articular elbow joint effusion which lifts the anterior fat pad away from the bone, making it visible on x-ray. A small anterior fat pad on a lateral film can be a normal finding, but a posterior fat pad is suggestive of elbow fracture, even if it is the only radiographic abnormality seen.
The majority of these injuries on follow-up are found to be nondisplaced supracondylar fractures.8 Due to the cartilaginous nature of the pediatric elbow, sometimes fractures are only visible in follow-up once callus has begun to form about the fracture site.6
PEDIATRIC FRACTURE PATTERNS
The following discussion outlines the most common pediatric fractures, along with an approach to management for each fracture. Any fracture variations, complicating factors, dislocations, or features that alter the neurovascular status require further discussion with an orthopedic surgeon.
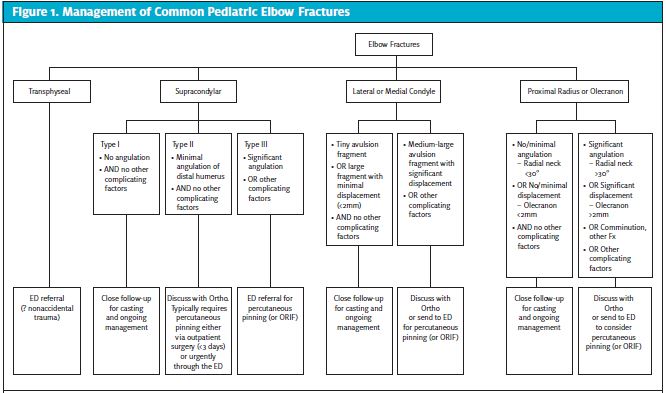
Transphyseal Humerus Fractures
This fracture pattern is only seen in young children, under age 2. It is caused by separation of the distal humeral epiphysis and can mimic an elbow dislocation. Because children of this age infrequently fall on an extended outstretched arm, this fracture is commonly inflicted and not accidental. Further investigation and evaluation for child abuse are recommended for any transphyseal humerus fracture similar to fractures of the mid-humerus in this age group. 5,6
Supracondylar Fractures
Supracondylar fractures are the most common pediatric fracture in the 0-7 age group9 and are generally caused by forcible elbow extension during a fall on an outstretched hand. Along with lateral condyle fractures, they are the most common pediatric elbow fractures requiring surgical intervention.10 Gartland classified extension supracondylar fractures in the following way: type I, nondisplaced fracture; type II, displaced with an intact posterior cortex; and type III, displaced with no cortical contact of the fracture fragment. (See Figure 2.)
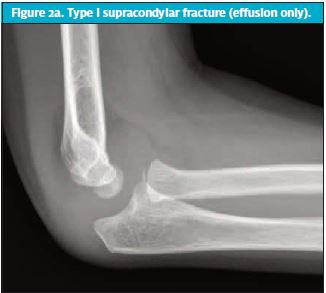


While type III fractures are difficult to miss, type I and II fractures can be subtle. The anterior humeral line is an important landmark to show anatomic position of the humerus against the capitellum. When the line is anterior to the middle-third of the capitellum, this suggests misalignment and possible need for percutaneous pinning to stabilize and align the joint.
Type I fractures are stable and can be treated with a posterior long arm splint with the elbow at 90° of flexion, and orthopedic follow-up for casting. Type II and III fractures require surgical intervention, though practice patterns vary with regards to the timing of the surgical pinning and when to use open vs closed reduction.3,6,10 Nerve injuries, particularly to the anterior interosseous nerve, are common in supracondylar fractures, especially in displaced fractures. Radial, median, and ulnar injuries are all reported.11 The majority of these nerve injuries are transient, with good long-term functional recovery.12
Lateral Condyle Fractures
A lateral condyle fracture (Figure 3) is the second most common fracture in the pediatric elbow. Patients generally present with swelling and tenderness limited to the lateral elbow.3 These fractures are intra-articular and often cross the distal humeral physis into the capitellar ossification center. They are less likely to have significant soft tissue or acute neurovascular injury, but long-term complications such as growth arrest, nonunion, avascular necrosis, and tardy ulnar nerve palsy are possible. Oblique elbow views improve diagnostic accuracy for lateral condyle fractures, which can be missed on standard AP and lateral views. Minimally displaced (<2 mm) fractures can be managed with casting in consultation with orthopedics. The patient should be splinted with forearm in neutral and the elbow at 90° flexion.4 Greater amount of displacement is generally treated with open3,6 or closed reduction with pinning.13

Medial Epicondyle Fractures
Medial epicondyle fractures tend to occur in older children, generally aged 10-14 years. They do not involve the physis, and a fat pad sign will be absent, as the medial epicondyle is extra-articular.3 Neurovascular complications are rare, but the ulnar nerve is most commonly affected. 6 Most patients with isolated, minimally displaced fractures can be acutely managed with a posterior long arm splint and outpatient orthopedic follow-up.3 If there is significant soft tissue injury, joint instability, or a fat pad sign on radiographs, then an additional bony or ligamentous injury should be suspected. Generally, these fractures are stable but if the fragment is significantly displaced or incarcerated in the joint, operative intervention is necessary.14 Fractures of the medial epicondyle should be differentiated from overuse traction injuries of the medial epicondyle apophysis which is sometimes termed “little league elbow.”
Proximal Radius Fractures
Proximal radial fractures are generally caused by a fall onto an outstretched hand leading to fractures of the radial neck or physis, which differs from adults where proximal radius fractures are more often in the radial head.
These fractures are most common in the preteen years.3 In isolated fractures, tenderness is localized to the proximal radius, which is palpable in the depression 1 inch distal to the lateral epicondyle when the elbow is flexed to 90°. Forearm rotation rotates the radial head, such that pronation and supination are painful with these injuries.4 Minimally displaced fractures can be difficult to identify on radiographs and have been reported as one of the most commonly missed fractures in pediatric urgent care. Oblique views, specifically the radiocapitellar view, can help with fracture identification.5 Radial neck fractures with less than 30° of angulation and less than 2-3 mm translation can be managed nonoperatively, in a posterior long arm splint with elbow at 90° flexion and orthopedic follow up. Angulation is better tolerated than translation, which tends to result in loss of supination/pronation if not adequately corrected.3,6
If a displaced radial neck fracture is noted, 50% of children will have another associated fracture. Care should be taken to evaluate the medial epicondyle, olecranon, coronoid process, and distal humerus on radiographs.6 The Monteggia fracture is a dislocation of the radial head associated with a fracture of the ulna. Ulnar malalignment needs to be corrected or it can lead to gradual dislocation of the radial head.
Radial Head Subluxation (Nursemaid’s Elbow)
Radial head subluxations mimic elbow fractures and are one of the most common injuries presenting to pediatric urgent care. This injury is caused by longitudinal traction on an outstretched arm, such as occurs when catching a child who has tripped while holding onto an adult’s hand. The traction causes stretching or partial tearing of the annular ligament which holds the radial head against the proximal ulna, allowing the radius to slip under the annular ligament. This injury is most common in children ages 1-4 and peaks in toddlers between 16 and 24 months of age. Classically, a child with a nursemaid’s elbow presents with no distinct injury; refusal to use the affected arm, holding it down to one side slightly pronated, without any swelling, bruising, or pain on exam.6 Radiographs should be reserved for patients with exam findings or if attempts at reduction have failed (Figure 4). Generally, radiographs will be normal, though a small percentage may have minimal displacement of the radiocapitellar line.15
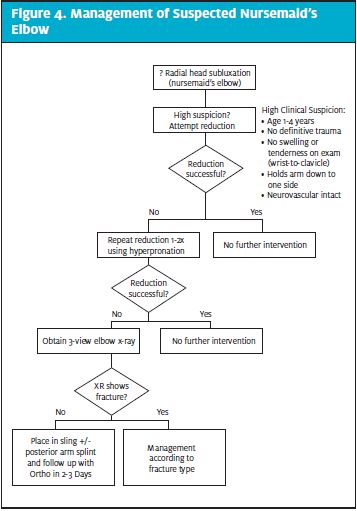
Reduction maneuvers involve either flexion-supination while applying pressure over the radial head or gentle hyper-pronation with elbow flexed. A click should be felt as the radial head reduces. Within a few minutes the child should use the arm normally. If a child fails to gain normal function of the arm and has a negative radiograph, the child should be placed in a posterior elbow splint with elbow flexed to 100° in full supination and follow up with the pediatrician or orthopedist, depending on level of suspicion for fracture. 6
PEARLS AND PITFALLS
- A three-view radiograph series (AP, oblique, lateral) is recommended for any suspected fracture to the pediatric elbow.
- Fractures of the radial neck and supracondylar type I fractures can be subtle. Special attention is necessary to avoid missing these fractures on radiographic assessment.
- Splinting and an orthopedic consultation are always recommended for any fracture where there are concerns about alignment, displacement, or exam findings out of proportion to the radiographic ones.
VIGNETTE CONCLUSION
Radiographs demonstrated a type II supracondylar humerus fracture with slight displacement of the distal humerus, suggested by displacement of the anterior humeral line. The patient was placed in a posterior long arm splint and sling. Orthopedics was consulted and able to arrange an outpatient ambulatory evaluation the next day to be followed by closed percutaneous pinning at an outpatient surgery center.
References
- Voth M, Lustenberger T, Auner B, et al. What injuries should we expect in the emergency room? Injury. 2017;48(10):2119-2124.
- Freed HA, Shields NN. Most frequently overlooked radiographically apparent fractures in a teaching hospital emergency department. Ann Emerg Med. 1984;13(10):900-904.
- Skaggs D, Pershad J. Pediatric elbow trauma. Pediatr Emerg Care. 1997;13(6):425-434.
- Eiff MP, Hatch R, Calmbach WL. Elbow fractures. In: Eiff MP, Harch R, eds. Fracture Management for Primary Care. 2nd ed. Philadelphia, PA: Elsevier; 2003:148-173.
- DeFroda SF, Hansen H, Gil JA, et al. Radiographic evaluation of common pediatric elbow injuries. Orthop Rev. 2017;9:21-26.
- Wenger DR, Pring ME. Elbow—distal humerus. Elbow—proximal radius and ulna. In: Rang M, Pring ME, Wenger, DR, eds. Rang’s Children’s Fractures. 3rd ed. Philadelphia PA: Lippincott Williams & Wilkins; 2005:95-134.
- Robertson JS, Marsh AG, Huntley JS. Neurological status in paediatric upper limb injuries in the emergency department – current practice. BMC Research Notes. 2012;5:324.
- Skaggs DL, Mirzayan R. The posterior fat pad sign in association with occult fracture of the elbow in children. J Bone Joint Surg Am. 1999;81:1429-1433.
- Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma. 1993;7:15-22.
- Pannu GS, Eberson CP, Abzug JM, et al. Common errors in the management of pediatric supracondylar humerus fractures and lateral condyle fractures. Instr Course Lect. 2016;15:385-398.
- Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop. 2010;30:253-263.
- Valencia M, Moraleda L, Díez-Sebastián J. Long-term functional results of neurological complications of pediatric humeral supracondylar fractures. J Pediatr Orthop. 2015;35:606-610.
- Justus C, Haruno LS, Riordan MK, et al. Closed and open reduction of displaced pediatric lateral condyle humeral fractures, a study of short-term complications and postoperative protocols. Iowa Orthop J. 2017;37:163-169.
- Vuillermin C, Donohue KS, Miller P, et al. Incarcerated medial epicondyle fractures with elbow dislocation: risk factors associated with morbidity. J Pediatr Orthop. 2017.
- Snyder HS. Radiographic changes with radial head subluxation in children. J Emerg Med. 1990;8:265-269.
Author affiliations: Amy Grover, MD is Senior Instructor of Pediatrics, Children’s Hospital Colorado, Section of Emergency Medicine, Section of Hospital Medicine.
Read More Pediatric Urgent Care Articles
- Pediatric Elbow Assessment: An Urgent Care Approach
- Pitfalls In Assessing And Managing Common Pediatric Injuries
- Preparedness For Emergencies In Pediatric Urgent Care Settings

