Urgent message: Fractures, in general, are relatively common among pediatric patients. Those most likely to be seen in the urgent care setting include injuries to the radius, ulna, humerus, lateral condyle, clavicle, tibia, and fibula. The second of two parts.
Justin Kunes, MD, Shane R. Hanzlik, MD, Allison Gilmore, MD
As noted in part 1 of this article (published in the February 2011 issue of JUCM and available at www.jucm.com), fractures are common injuries in the pediatric population. Among children seeking medical attention for an injury, approximately 20% will be found to have a fracture.1 Boys are more likely than girls to experience a fractures, with an incidence of 42% between ages 1 and 16 years; for girls in this age range, the incidence is 27%.
This article will review assessment and treatment of the most common fracture sites: the distal radius, clavicle, hand, elbow, and tibia.2
Distal Radius and Ulna Fractures
Distal forearm fractures (Figure 1) occur in falls onto out- stretched hands (FOOSH). These are commonly apex volarly angulated.
Distal radius fracture pat- terns include the torus frac- ture with a thickened ripple in the cortex, often best as- sessed on the lateral view of the wrist.
Greenstick fractures, in which one cortex may re- main intact, are also quite common.
The third most common assessment and treatment of the most common fracture sites: the distal radius, clavicle, hand, elbow, and tibia.2 pattern is a complete transverse fracture.
Management
The goals in treating all fractures are the same: reduce the fracture (manipulate unacceptable alignment to within acceptable limits) and immobilize the limb to minimize pain and prevent recurrent deformity.
In children, reduction often requires conscious sedation to alleviate suffering and allow muscle relaxation for reduction.
Fractures treated within 24 hours of injury should be immobilized in a splint, not a cast, to allow for swelling and prevent a compartment syndrome from forming due to circumferential restriction.
Normal x-rays with pain and tenderness A distal radius or wrist injury is evaluated with clinical and radiographic examination, but sometimes no fracture is clearly identified. These injuries should still be immobilized and sent for follow-up within a week. Sometimes children have occult injuries that do not show up on initial radiographs, but a few weeks later demonstrate abundant callus.
If in doubt, always err on the side of splinting a child.
Immobilization for distal radius fracture
The most reliable means of immobilizing any wrist or forearm fracture is a sugar- tong splint. This prevents forearm rotation by being applied volarly, wrapping around the elbow posteriorly and coming up on the dorsal side of the forearm with the elbow bent. Pre-fabricated, pre-padded fiberglass splints that are readily available in urgent care centers work well, as long as there is sufficient webril (cotton padding) over bony prominences. However, certain precautions must be applied in order to successfully apply such a splint.
- Starting: Dorsally just below the metacarpophalangeal (MCP)
- Forearm in neutral rotation patient seated up- right, elbow held at the patient’s hip, thumb point- ing to the
- Elbow flexed to 90° degrees, the splint makes a 180° smooth curve against the triceps
- End: Volarly at the proximal palmar crease (patient can flex the MCP joints to 90°).
- Sling should be used (fracture can still bend in an ulnoradial direction).
Elbow Fractures
Elbow fractures include any bony injury to the distal portion of the humerus and the proximal ulna and ra- dius. These comprise 10% of all fractures in children. While common, the diagnosis and management of these injuries is complex, and a good outcome requires early recognition and referral to an orthopedist. Most of these fractures involve the supracondylar anatomic region of the distal humerus.
Supracondylar Humerus Fracture
Diagnosis
A child with a supracondylar humerus fracture may have mild swelling to marked swelling and pain at the elbow. Severe injuries have puckered skin, blistering, ecchymosis, and palpable or visible bone.
Even more anatomic structures are at risk than at the wrist, and an even more detailed neurologic and vascular examination is warranted. The ability to flex (median) and extend (radial) the digits and thumb, oppose the thumb and index finger (anterior interosseous branch of median) and abduct and adduct the fingers (ulnar) should be checked.
Assess radial pulse by palpation, and check capillary refill in all digits. If these are absent, perform or refer for a Doppler exam; if pulses remain absent, suspect a brachial artery injury. This requires emergent orthopedic evaluation.
Radiographs should include an anterior-posterior and lateral view of the elbow. The lateral view of the elbow must be perpendicular to the distal portion of the humerus. Then, a line is drawn down the anterior cortex of the humerus (the anterior humeral line).
In a normal elbow, this line should bisect the capitellum. The radial head should also point directly towards the capitellum (Figure 2a).
Sometimes, patients will have an occult injury with a lateral radiograph of the elbow demonstrating an anterior and posterior fat pad sign. An anterior fat pad sign can be normal but a posterior fat pad sign is always ab- normal and suggestive of a fracture (Figure 2b).
Treatment
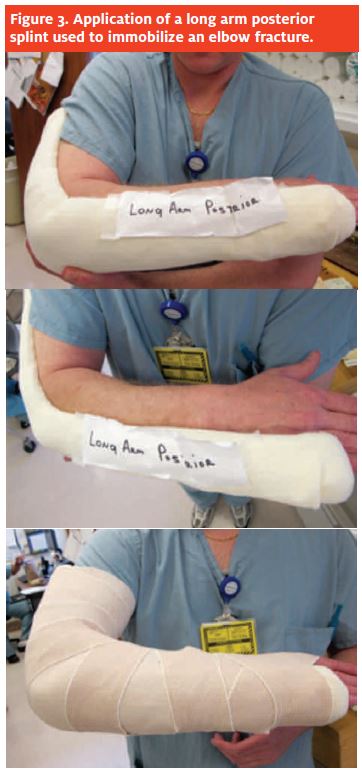
Nondisplaced fractures may be splinted in a posterior long arm splint (Figure 3) in 30° to 40° of flexion and referred to an orthopedic clinic in a few days.
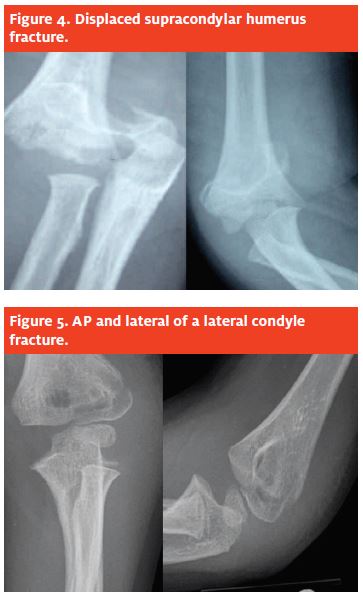
A displaced fracture (Figure 4) must be splinted and transferred to an emergency department with pediatric orthopedic coverage. These fractures are fixed surgically the same evening or early the next morning and for best results treatment should not be delayed.
Lateral Condyle Fractures
The second most common elbow fracture is actually the most common physeal fracture of the elbow, involving the growth plate. The position and force direction for this injury is much the same as the other two fractures (FOOSH), with the addition of a varus movement about the joint.
Diagnosis
In lateral condyle fractures, there is focal swelling and pain at the lateral distal humerus. Evaluate just as you would for a supracondylar humerus fracture, but bear in mind that neurologic and vascular injuries are less com- mon with this fracture pattern. Most require surgery, thought not urgently.
The usual fracture line on the AP film extends from the lateral distal humeral metaphysis to just medial to the capitellum (Figure 5) and exits distally into the joint. These fractures are more subtle and may be nondisplaced.
Treatment
Apply a long arm splint and have the patient follow up with an orthopedist in one to three days to discuss surgery vs. nonoperative treatment.
Clavicle Fractures
Clavicle fractures occur from a direct fall onto the shoulder, a fall onto an outstretched hand, and, less commonly, from a direct blow. Eighty percent occur in the middle third of the shaft, 15% in the distal third, and 5% proximally.3 Patients present with localized pain and discomfort over the fracture site, and pain with shoulder motion.
Diagnosis
A child with an acute clavicle fracture holds the elbow of the injured limb with the opposite hand and tilts the head toward the injured side to minimize the displacing pull by the sternocleidomastoid and trapezius muscles. Obvious deformity is likely visible, with point tenderness over the fracture site and subcutaneous crepitus. Breaks in the skin near the fracture indicate a possible open fracture.
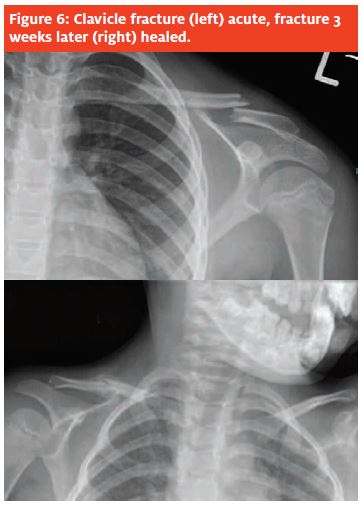
Often, AP views (Figure 6) of the shoulder are sufficient, but a serendipity view (40° cephalad-directed tube angle) may be helpful.
Most pediatric and adolescent clavicle fractures are managed non-operatively with a figure-of-eight band parents and child that a noticeable bump will be visible over the fracture site due to healing callus.
Typically, simple fractures will remodel over six to nine months with no resulting functional impairment. Children with appropriate histories and point tenderness over the clavicle should be treated with the presumption that a fracture has occurred.
Skin tenting and laceration demand emergency room transfer and urgent orthopedic consultation. For the rare open or shortened fracture, surgical management will be necessary.
Tibia and Fibula Fractures
Fractures of the tibia and fibula shaft are among the most common injuries involving the lower extremities in pediatrics. They occur in falls with a twisting movement to the foot, resulting in oblique or spiral fracture configurations. Direct trauma often produces a trans- verse or segmental fracture pattern. These are the most common long bone fractures of the lower extremity (15% of all pediatric fractures).4
Diagnosis
The most common presenting complaint will be pain and an inability to bear weight. Many will be non- displaced with no obvious deformity. Tenderness to palpation at the fracture site should lead to radiographic analysis which includes an AP and lateral radiograph (Figure 7) of the tibia and fibula including the knee and ankle joints.
A thorough neurovascular exam must be documented including the presence of the dorsalis pedis and poste- rior tibial pulses and capillary refill. Document active and passive range of motion at the ankle joint and of the toes. Tight compartments and severe pain with passive great toe extension indicate compartment syndrome, es- pecially in high-energy displaced or segmental tibia fractures.
Acute management
Most non-displaced fractures may be treated with a long leg splint with long side slabs from the foot to two- thirds up the thigh; 20° to 30° of knee flexion will help prevent weight-bearing, and keeping the foot plantar flexed 10° to 15° will keep the pull of the long toe flex- ors from displacing the fracture further.
These patients need to follow up with an orthopedist within one week.
Many urgent care centers have prefab splints which
can be used, as long as care is taken to avoid pressure over the heel, which can lead to a heel ulcer.
Displaced fractures may be treated by an orthopedic doctor with a closed reduction under conscious sedation to obtain near anatomic alignment.
Fractures not amenable to closed treatment should be admitted to the hospital and prepared for surgery.
Any closed reduction should be followed by a careful repeat of the neurovascular examination of the leg and foot.
Toddler’s Fractures
Children less than 2 years of age or just beginning to walk may suffer a non-displaced spiral or oblique frac- ture of the tibia known as a “toddler’s fracture.” These result from a seemingly harmless event, such as tripping while walking or running, stepping on a ball or toy, or falling from a modest height.
Diagnosis
Children with a toddler’s fracture often fail to bear weight or may limp. Findings are often subtle. Most do not have any soft tissue swelling, ecchymosis, or defor- mity. Localized tenderness to palpation is the most common physical finding. It is important to examine the hip, thigh, knee, and ankle joint, as well, to rule out any other causes.
AP and lateral radiographs of the entire tibia and fibula (Figure 8) may demonstrate a spiral fracture of the distal third of the tibia, but they may also be nor- mal. Characteristically, a faint oblique fracture line is seen crossing the distal tibial diaphysis, terminating medially. If a fracture is suspected and not seen, oblique views may be beneficial.5 The fracture line may be visualized on only one film or not visualized at all. Halsey and associates reported that of 39 chil- dren with a suspected toddler’s fracture and negative initial radiographs, 16 (41%) had a toddler’s fracture confirmed on follow-up radiographs.6
Acute management
In small children refusing to bear weight with localized tenderness of the tibia, a long leg plaster splint is indicated even in the setting of negative radiographs. They should be seen by an orthopedist within one week.
Ankle Fractures
Most ankle fractures in children involve the growth plate. Children usually sustain an ankle injury from run- ning or jumping during sports or play.
Diagnosis
Children with ankle fractures present with obvious swelling and pain over the malleoli. They usually can not bear weight. Radiographs include AP, lateral,and mortise radiographs (Figure 9). A good neurologic exam is important.
Management
Displaced fractures involving the growth plate should be reduced under conscious sedation or admitted for surgery the next morning. Injuries at the growth plate in an ankle need to be close to anatomically aligned to pre- vent further deformity, pain and or arthritis. Nondis- placed fractures can be treated in a short leg posterior splint with side slabs (Figure 10); displaced fractures should be splinted with a long leg splint all the way up the thigh to prevent rotation of the fracture. The knee should be slightly bent, and the patient should be sent home non weight-bearing on crutches and be told to elevate the leg until fol- low-up with an orthopedist.
Morbidity is increased with poorly placed splints. Care must be applied to take pressure off of the heel.
Conclusion
Nearly 20% of children coming to the urgent care with an injury will have a fracture. It is important to remember that physeal injuries are very common and may present with no radiographic findings.
Occult injuries are also possible in the shaft of the bone in children. If in doubt, it is still better than not to splint a suspected fracture in a child. If a fracture displaces, a physeal arrest may occur.
A thorough history and exam, adequate radiographs, and a good splint with care to avoid pressure over bony prominences will help patients and their families get through the healing process with minimal discomfort.
Typically, children heal quickly and usually re- turn to full preinjury activity level.
- Buckley SL, Gotschall C, Robertson W Jr, et , The relationships of skeletal injuries with trauma score, injury severity score, length of hospital stay, hos- pital charges, and mortality in children admitted to a regional pediatric trauma center. J Pediatr Orthop. 1994;14(4):449-453.
- Landin LA., Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 202:1-109.
- Stanley D, Trowbridge EA, Norris The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg [Br]. 1988;70(3):461- 464.
- Shannak Tibial fractures in children: Follow-up study. J Pediatr Orthop. 1988;8(3):306-310.
- Dunbar JS, Owen HF, Nogrady MB, et Obscure tibial fracture of infants— The toddler’s fracture. J Can Assoc Radiol. 1964;25:136-144.
- Halsey MF, Finzel KC, Carrion WV, et Toddler’s fracture: Presumptive diagnosis and treatment. J Pediatr Orthop. 2001;21(2):152-156.