Urgent message: Though data are limited and approaches to burn blister management remain controversial (eg, leaving blisters intact vs deroofing or aspirating), appropriate initial care in the urgent care setting is both feasible and advisable and can reduce risk for infection and scarring.
Muhammad Zeeshan Ahmed MBBS, FRNZCUC, Winston McEwan FRACS, and Sana Maqsood MPhil, Cert PH
Citation: Ahmed MZ, McEwan W, Maqsood S. Management of burn blisters in urgent care. J Urgent Care Med. 2022;16(10):13-18.
INTRODUCTION
Though positive outcomes can be achieved with appropriate wound care and dressing, assessing and managing burn injuries can be a challenge in the urgent care setting, especially concerning burn blisters and immediate dressings. What literature exists leaves the clinician on the horns of a dilemma: whether to aspirate or deroof blisters or leave them intact to act as a biological dressing.
Varying opinions on management of burn blisters emphasize their biochemical, physiological, and anatomical features. Burn blisters contain a mixture of several chemicals; some promote, while others delay, wound healing.
Arguments favoring the preservation of intact blisters focus on the idea of a natural biological protective process from intact blisters. On the other hand, those favoring aspiration or deroofing perceive that it reduces wound infection rate and complications and makes dressings more secure. In addition, there have been conflicting statements on the management of small and medium or large blisters. Some propose leaving small blisters less than 6 mm2 intact, with debridement for others.
CASE DESCRIPTION
A 12-year-old girl presented to the urgent care facility with a burn on her right thigh. Her parents accompanied her.
The girl burned her thigh after hot boiled water spilled over her thigh approximately 2 hours prior to presentation. She had immediate severe pain, and later blisters started to develop. The burn area cooled with running water at home for 5 minutes.
Past medical history was not significant, and she had no known drug allergies. She was fully immunized.
Examination
The patient had a pulse of 115 with a blood pressure of 122/72, and she was afebrile. She was alert and well-appearing on general examination. She was given acetaminophen 500 mg on arrival during triage.
Examination of the leg revealed a superficial dermal burn of approximately 5 x 6 cm / 1% total body surface area (TBSA) on the right lower anterior thigh with small blisters formation.
The rest of the examination revealed no other injuries, and the limb’s distal neurovascular status was intact.
The Plan
Further cooling with running water was provided at the clinic intermittently for 20 minutes. Gentle cleaning with saline and chlorhexidine was done. The wound was dressed with Jelonet.
On discharge, she was advised to rest and keep the limb elevated. She was given a script for acetaminophen and ibuprofen for pain relief, with instructions to return for review and a change of dressings in 48 hours.
The follow-up exam 2 days later revealed erythema was decreasing, though there was still some tenderness. Most small blisters were still intact. A couple of them were self-ruptured but still acting as good biological skin, and there was not much loose skin for doing any debridement. The plan was to continue with similar dressings and care.
Short-term and long-term scar care plans, including moisturizer use and protecting the burn area from the sun, were explained to the patient and family. Follow-up for ongoing review with the general practitioner and scar care with the scar team was advised.
BACKGROUND
This article will review published literature and guidelines on the management of blisters in the partial-thickness burn (superficial and mid-dermal) with emphasis on implementing appropriate methods into clinical practice to achieve optimal outcomes.
While some urgent care providers leave blisters intact, others aspirate or deroof the blisters. In deciding, one has to consider a few essential aspects that are vital in general patient care and wound healing, such as:
- Are there some blisters that can be left as such?
- Is it necessary to debride blisters to assess the burnt area better?
- Is it painful for the patient?
- What is going to heal better and quicker?
Burn injuries are distinctive, as the injured area usually contains various zones of tissue damage depending upon the amount of heat transfer.1 Clinicians working in emergency rooms, urgent care, or even primary care encounter burn blisters on a regular basis. Management of more minor burn injuries in the urgent care center can be improved by providing appropriate first aid, good burn dressings, and effective wound management. Overall, this will reduce the chances of a burn getting deeper or infected and reduce the need for specialist review or surgery.2
Burn wound healing is a very complex and intricate process that involves several cell types and chemical mediators.3 Multiple factors (eg, burn area, patient’s age, overall health level, comorbid conditions, smoking status, and many others) contribute to burn wound healing.
As a burn blister contributes to wound healing by protecting the wound,4 its management can prove to be pivotal for the outcome. The critical parameters that help define the treatment options are patient comfort, ease of dressing, cost-effectiveness, risk of infection, healing time, functional and aesthetic outcome.4 Clinicians should take these outcome factors, as well as the available literature, into account when deciding on burn management.
EPIDEMIOLOGY/STATISTICS
A burn is a common form of trauma in all age groups. Burns are the fourth most common type of trauma worldwide following traffic accidents, falls, and interpersonal violence.5
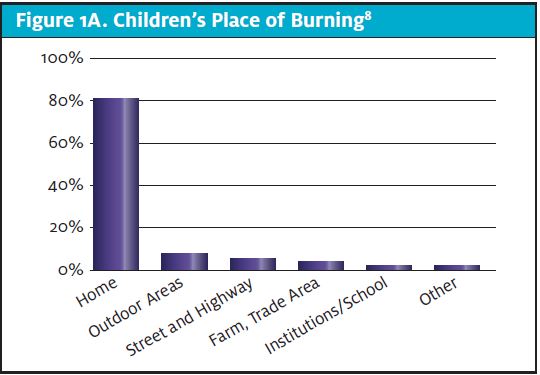
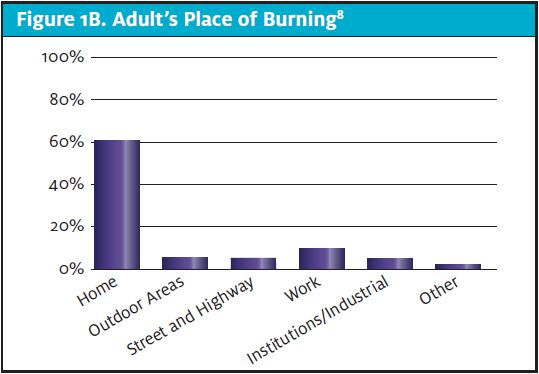
Approximately 486,000 burns requiring medical treatment occur annually in the United States.6 In both adults and children, the most typical place to be burned is in the home.7-9 In children, 82% of accidents occur at home.9,10 (See Figures 1A and 1B.) Most scald burns in children and adults happen in the kitchen and the bathrooms.
Data as recent as 2020 indicate that the most prevalent modes of burn among pediatric patients are scald (52%), contact burn (25%), and flame burn (11%). In contrast, flame burn (42%) is the most common mode in adults, followed by scalds (26%) and contact burns (18%).8
ASSESSMENT AND BURN CLASSIFICATION
When assessing burns and considering treatment options, it is important to bear in mind certain aspects of the history, including:
- Mechanism of burn
- Time since burn
- Immediate cooling/irrigation
- Assessment of degree of burn
- When to refer based on TBSA burn, burn of particular areas, cause of the burn
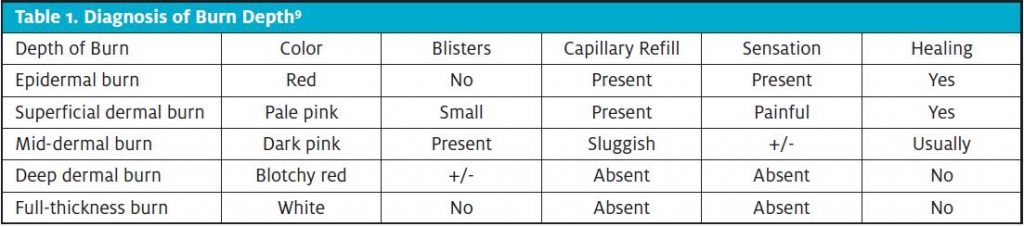
Next, burn classification helps in identifying burn depth based on clinical assessment. Burns are subclassified according to the thickness of the burn (see Table 1):
- Epidermal burn
- Superficial dermal burn
- Mid-dermal burn
- Deep dermal burn
- Full-thickness burn
In practice, all burns are a mixture of different depths due to differences in heat transfer.1
THE NATURE OF THE BURN BLISTER
It is essential to know why burn blisters form in the first place. A burn induces inflammatory changes that lead to increased capillary permeability, resulting in the fluid collection between the dermis and epidermis.4 The epidermis separates from the dermis, resulting in formation of blisters of various sizes.1,4 The blister contain several chemicals and molecules that affect wound healing.11
Burn blisters occur mainly in superficial dermal burns, but they can also develop in mid- to deep dermal burn areas.4,12 Superficial dermal burns damage the epidermis and upper part of the dermis, ie, the papillary dermis. The prominent feature of superficial dermal burn is blister formation. This type of burn should heal spontaneously by epithelialization within 2 weeks and leave only a color-match defect.4,13
In mid-dermal burn, spontaneous healing usually does not happen as the damage is deep, and thus there are fewer surviving cells to facilitate re-epithelialization.4,13
After initial assessment of the burn, it is vital to answer the following questions:
- Can that burn be safely managed on site?
- Does it need discussion with the plastic surgery team?
- Should the burn patient be transferred to a plastic surgery/burn center? (For example, burns >10% TBSA or 5% in a child, burns to special areas—face, hands, feet, perineum, over major joints, full thickness burns >5% TBSA, circumferential burns of the limbs or chest, burn with inhalation injury etc.9)
Most reported burns in the community do not need hospital-level care and can be safely managed in the urgent care center. A large proportion of these burns are superficial burns with the hallmark of blister formation. On the other hand, major burns reported to the burn centers usually require significant debridement.
Once the management plan is decided based on the burn assessment, the next step is dressings and addressing the blister areas.
EVOLUTION OF BURN BLISTER MANAGEMENT
Current evidence regarding management of burn blisters is limited and controversial.1,14 The last three decades have seen a remarkable evolution in burn management, which has resulted in a vast reduction in mortality; further, morbidity outcomes are significantly better. Burn wound care has also evolved as more patients have survived. Research has advanced to the point that we now can observe details of wound healing at a microscopic level. In the process, several dressing options have emerged to allow wounds to heal more quickly and thoroughly.
Looking all the way back to the 1940s, management of burn wounds initially meant leaving the blisters intact.4
That practice was reinforced a decade later in a study that is likely to be considered unethical in the current practice. Gimbel, et al created a row of burns on healthy volunteers.15 Few blisters were left intact, with others deroofed or aspirated. The intact blister group healed faster.
Later, concerns were raised that blister fluid might propagate bacterial growth, which led to the concept of debridement of the blisters and using some dressings. With advances in the 1970s and 1980s, dressings like silver sulfadiazine, auto and allografts, Biobrane and TransCyte were increasingly used, with the goal of increasing wound healing and achieving better scarring.4 Burn wound or blister debridement was required for using these special dressings.16
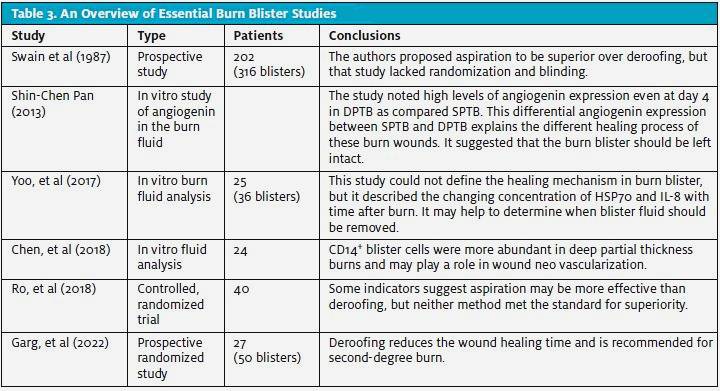
Swain et al published a study in 1987 analyzing bacterial colonization and wound pain in three treatment options for blisters—ie, deroofing, aspiration, and leaving blisters intact. The incidence of infection with Staphylococcus aureus was higher with the exposed (deroofed) group with a p-value of <0.05. The pain score was also higher and statistically significant in the exposed group.17 The authors proposed aspiration to be superior over deroofing, but that study lacked randomization and blinding.11,17
Studies involving burn fluid analysis, which could prove to be an essential indicator in deciding the fate of blisters, have shown conflicting results.
Shin-Chen Pan published a study in 2013 analyzing the burn fluid in the neovascularisation of the burn wound healing.3 Early injury conditions contain important angiogenic factors that promote the neovascularization phase of wound healing. The study noted high levels of angiogenin expression even at day 4 in deep partial thickness burn (DPTB) as compared to superficial partial thickness burn (SPTB). This differential angiogenin expression between SPTB and DPTB explains the different healing process of these burn wounds. It suggested that the burn blister should be left intact. The study provided a model to show how angiogenin factors, cytokines and growth factors play a role in burn wound revascularization.3
On the other hand, Yoo, et al (2017) studied another spectrum of blister fluid.13 They did serial analysis for heat shock protein 70 (HSP70) and interleukin-8 (IL-8) levels in the blister fluid. Previous studies have shown HSP70 and IL-8 as pro-inflammatory factors, prolonging the inflammatory phase of wound healing. HSP70 peaked at 12 hours postburn, and IL-8 peaked on the fourth day. Based on that, they suggested that these levels may help determine when the blister fluid should be removed. The study had some limitations, including small sample size, and it does not clearly describe the healing mechanism and role of those factors.12
In 2018, Chen, et al analyzed various chemicals and factors in burn blister fluids in superficial and deep partial-thickness burns.12 Their data noted a predominance of CD14+ in blister fluid of deep partial-thickness burns, and they suggested that it plays a role in burn wound neovascularization. Though the study did not directly suggest leaving the blisters intact, it indirectly shows that burn blister fluid has some factors that help to heal. In 2018, Ro, et al published their prospective randomized controlled trial comparing aspiration with deroofing burn blisters (larger than 6 mm) as a method of burn blister management.1 Outcomes included healing time, patient comfort, wound colonization, and functional and aesthetic outcomes. While the sample size was relatively small (N=40), neither aspiration nor deroofing treatment options was found to be superior.1 It should be noted that aspiration was found to be a more effective method reducing pain and scar thickness, though not to a statistically significant degree. The researchers noted that the deroofed group had worse scarring than the aspirated group. Deroofing itself can be a painful procedure for the patient and can be a potential reason for increased bacterial colonization and infection. (See Table 2.) Surprisingly, the aspiration group with burns to the head and trunk areas, both of which are very vascular, healed more slowly than limbs. Again, however, this finding was not statistically significant.
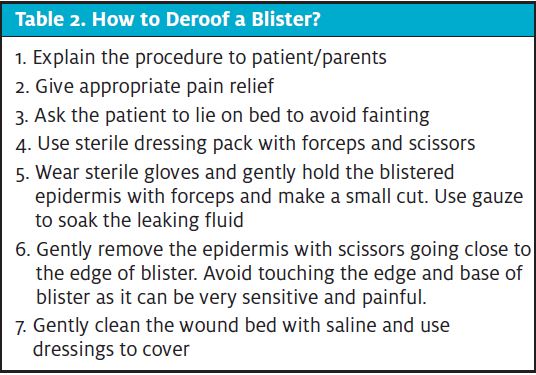
Garg, et al in 2022, published their prospective study on 50 burn blisters in 27 cases.16 They randomly assigned them into two categories and noted deroofing reduces the wound healing time and is recommended for second-degree burn. The study noted higher pain score in the deroofing group, 16 cases (64%) in the deroofing group gave a severe pain score of 4 or more on the visual analog scale as compared to 2 cases in the intact blister group with pain score of 4. See Table 3 for a summary of essential burn blister literature.
Blister Management Considerations
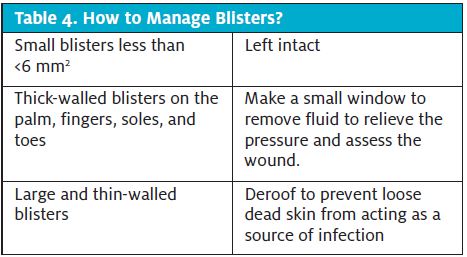
Burn blister management depends on the size of blisters; smaller blisters (<6 mm) are treated differently than larger ones.1,17 Similarly, blisters on the soles of feet (more likely to rupture spontaneously) will be treated differently than blisters somewhere else on the body.10,16
There have been conflicting statements on the management of small and medium or large blisters. Some propose leaving small blisters <6 mm2 and doing debridement for others. The New Zealand National Burn Centre (NZNBC) suggests small blisters can be left intact except for those over the joints or if movement is limited, whereas large, tense blisters should be snipped and covered with dressings.9
The British Burn Association (BBA) proposes management depending on the site and size of burn blisters.14 They suggest leaving small blisters <6 mm2 intact and debriding or deroofing larger blisters.
It is crucial to deroof blisters, at times, as this allows proper observation of the wound bed and accurate assessment of burn depth.11 Ruptured blisters should be managed by removing the nonviable skin to allow faster wound healing and reduce risk for scarring.
Deroofing tense large blisters reduces tension on the underlying tissue, and thus preserves the wound microcirculation and prevents the progression of burn depth.17
The Royal Australian College of GP (RACGP) recommends blister debridement and applying nanocrystalline silver dressings for 2 days before a decision regarding burn depth is made.2
Literature reveals some recommendations, but there are many limitations in those studies. There is a need for a large, well-designed randomized controlled study based on the available data and treatment options.
Small blisters less than <6 mm2 can be left intact as they are unlikely to self-rupture or damage underlying tissues. Leaving them intact can also control pain as it does not expose the superficial nerves to the outside world.
Thick-walled blisters on the palm, fingers, soles, and toes are associated with discomfort and limited mobility. They can be managed by making a small window to remove fluid to relieve the pressure and assess the wound.
Large and thin-walled blisters are likely to rupture spontaneously, so they are better deroofed to prevent loose dead skin from acting as a source of infection. Debrided areas should be covered with recommended dressings.
See Table 4 for a summary of blister management considerations.
Burn dressing availability is quite variable across the medical practices and emergency departments. Bactigras, gauze dressing, or Jelonet is usually available in most clinics, whereas silver dressing other than silver sulfadiazine availability has been quite variable. There is no role of systemic prophylactic antibiotics in prevention of infection.18
Recommendation based on the research is to have burn management and blister care written protocol posted in the urgent care clinics. Most minor burns do not need discussion with the plastic surgery/burn team. If a commonly agreed protocol is available, it will reduce confusion amongst the treating clinicians and thus will provide continuity of care.
CASE RESOLUTION
In the case mentioned above, the burn area was relatively small, with small blisters, so leaving them intact was possibly the better option.2 If blisters self-rupture, it is better to gently debride the dead loose skin as it can be a source of infection or discomfort for the patient.
The family followed up with their general practitioner as was recommended in the urgent care center. Further follow-ups with their doctor saw good signs of healing. The wound healed completely in 2 weeks.
CONCLUSION
Burn blister management remains controversial, though recommendations from the limited data support leaving smaller blisters intact and deroofing or aspirating the larger blisters. Since most minor and partial-thickness burns are common presentations in urgent care clinics, the outcome can be improved by providing appropriate initial care, including good wound care and dressings. Thus, it can reduce the risk of the burn becoming deeper or infected and potentially reduce over scarring.
REFERENCES
- Ro H-S, Shin JY, Sabbagh MD, et al. Effectiveness of aspiration or deroofing for blister management in patients with burns: a prospective randomized controlled trial. Medicine. 2018; 97:17(e0563).
- Douglas HE, Wood F. Burn dressings. Austral Fam Phys. 2017;46(3):94-97.
- Pan S. Burn blister fluids in the neovascularisation stage of burn wound healing. A comparison between superficial and deep partial-thickness burn wounds. Burn Trauma. 2013;1:27-31.
- Sargent RL. Management of blisters in the partial-thickness burn: an integrative research review. J Burn Care Res. 2006;27:66–81.
- Peck MD. Epidemiology of burn injuries globally. In: UpToDate. Jeschke MG, ed. UpToDate. Waltham MA. https://www.uptodate.com/contents/epidemiology-of-burn-injuries-globally. Accessed June 5, 2022.
- American Burn Association. Burn incident fact sheet. Available at: https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/. Accessed May 20, 2022.
- Safekids Aotearoa. Childhood Burns in Aotearoa 2020. Available at: https://media.starship.org.nz/download-childhood-burns-in-aotearoa-2020-%3E%3E/Childhood_Burns_2020.pdf. Accessed October 08, 2021
- Monash University. Burns Registry of Australia and New Zealand Annual Report 2019/20. Available at: https://anzba.org.au/assets/BRANZ_AnnualReport_Jul19-Jun20.pdf. Accessed October 08, 2021
- New Zealand National Burn Service. Initial assessment and management of burn Injuries – guideline, Counties Manukau District Health Board. Available at: http://www.nationalburnservice.co.nz/assets/Documents/Emergency-plan/c3976d141b/NBS-initial-assessment-guideline.pdf. Accessed October 08, 2021
- Morgenstern J, Gottlieb M. Emergency department management of burn blisters. Ann Emerg Med. 2020;76:770-771.
- April MD, Koyfman A, Long B. Select burn blisters should not be left intact. Ann Emerg Med. 2020;76:771-773
- Chen S-H, Wong T-W, Lee C-H, et al. Predominance of CD14+ cells in burn blister fluids. Ann Plast Surg. 2018;80(1):S70-S74
- Yoo K, Suh KY Choi GH, et al. Serial changes of heat shock protein 70 and interleukin-8 in burn blister fluid. Ann Dermatol. 2017;29(2):194-199
- British Burn Association. BBA clinical practice guideline for the management of burn blisters. Available at: https://www.britishburnassociation.org/wp-content/uploads/2017/06/BBA-Burn-Blister-Management-Guideline-20.6.18.pdf. Accessed October 08, 2021.
- Gimbel NS, Kapetansky DI, Weissman F, Pinkus HK. A study of epithelization in blistered burns. AMA Arch Surg. 1957;74(5):800-803.
- Swain AH, Azadian BS, Wakeley CJ, Shakespeare PG. Management of blisters in minor burns. Br Med J. 1987;295:181.
- Garg R, Rakesh D, Mittal RK, et al. Managing blisters in minor burns: Should they be deroofed? Indian J Burns. [Epub ahead of print].
- Wiktor A, Richards D. Treatment of minor thermal burns. UpToDate. Moreira ME, Torrey SB, eds. Available at: https://www.uptodate.com/contents/treatment-of-minor-thermal-burns?source=history. Accessed June 5, 2022.
