Urgent message: Ultrasound can provide essential data in the urgent care evaluation of gynecological and obstetrical problems, such as suspected ectopic pregnancy (and is the test of choice for first-trimester pregnant women with abdominal pain or vaginal bleeding).
Andrew Alaya, MD, MSc and Harold Pelikan, MD
INTRODUCTION
An ectopic pregnancy or extrauterine gravidity (EUG) is a pregnancy that implants outside of the uterus. In 90% to 95% of EUGs, the pregnancy lies in the fallopian tubes, in about 5% in the ovarium, and in 1% to 3% in the cervix, in the surrounding abdominal cavity, and in prior cesarean scar.1 Prevalence of EUG has been reported to be as high as 18% in women who present due to vaginal bleeding and/or abdominal pain.2 EUG is one of the first differential diagnosis for abdominal pain in women of childbearing age. However, generally it is ruled out when urine human chorionic gonadotropin (hCG) levels are negative and with no evidence of intra or extrauterine gravidities present on ultrasound examination.3
Outside of a hospital setting, serum hCG is less likely to be available and urine tests are usually performed. A standard urine test can detect βhCG as low as 20 IU/L.3 A negative urine test would indicate no pregnancy.
Unfortunately, this is not always correct.
This case study shows that an EUG can take place with a negative urine test and no evidence of intra or extrauterine pregnancy with the use of ultrasound performed by an inexperienced operator. And yet an EUG was large enough to rupture. Considering the mortality and morbidity associated with a ruptured EUG, this illustrates the necessity of the use of serum hCG before ruling out EUG.
CASE PRESENTATION
A 23-year-old nulliparous woman presented complaining of acute right lower abdominal pain. She had marked right tenderness on superficial and deep abdominal palpation. She was alert and well appearing. She had a regular menstruation cycle, no intermittent blood loss and was on the third day of what she thought was her menstruation cycle. She did not think that she was pregnant or had any sexual transmitted disease. Her last sexual intercourse was 1½ months ago. Her temperature was 36.3°C, heart rate was 90 beats per minute, blood pressure 116/67 mm/Hg and SpO2 was 100%. Vaginal inspection showed clear blood coming from the cervical ostium; the cervix itself and vaginal walls looked normal. Ultrasound showed a normal uterus and endometrium, no evidence of EUG. The left ovary was normal (2.3 x 1.5 cm) with 2.5 cm fluid around it; the right ovary was enlarged (5.3 x 3.5 cm) with thick walls. Sliding movement was painful. Her bloodwork was normal. The woman was referred to the hospital where she was admitted for observation with a differential diagnosis of a possible ruptured cyst or torsion.
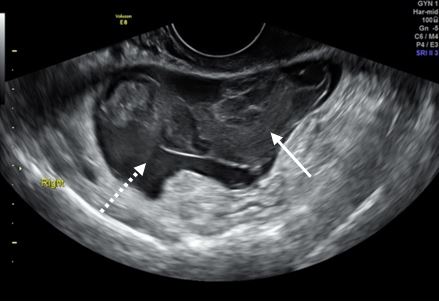
A transvaginal ultrasound showed an echogenic, avascular mass of 2.8 x 2.5 cm (Figure 1) next to the right ovary, that had a blood clot hanging from it, floating in the ascites (Figure 2). A ruptured fallopian tube due to an EUG was suspected.
She underwent laparoscopy with findings of a perforated fallopian tube due to an EUG. Approximately 600 mL of blood with clots was evacuated from the abdomen. Pathology confirmed the presence of a tubal EUG.
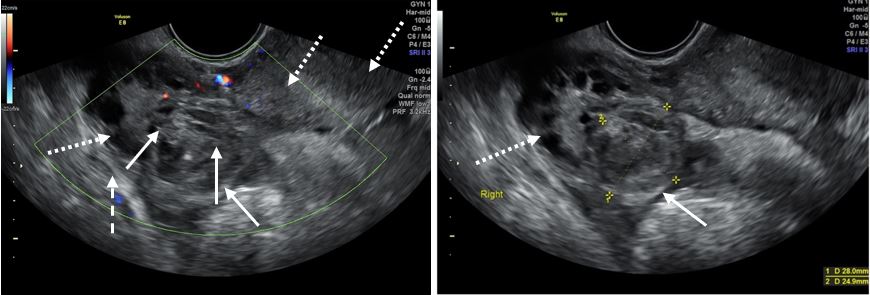
1a: Echogenic avascular mass (arrow) next to ovary (dotted arrow); 1b: echogenic mass of 2.8 x 2.5 cm (arrow) next to right ovary (dotted arrow).
DISCUSSION
EUGs comprise about 2% of all live birth pregnancies. Risk is increased with previous genital infection such as pelvic inflammatory disease (PIC) from Chlamydia trachomatis or Neisseria gonorrhoeae, but is also increased in patients with congenital abnormalities, endometriosis of previous surgery.4 Incidence can increase to as high as 4% among those using assisted reproductive technology (ART). In total, EUG is responsible for about 10% of women’s deaths during the first trimester of pregnancy.5
In the urgent care setting, a woman with vaginal bleeding and/or abdominal pain who is of childbearing age should have a pregnancy test. A positive test should be followed with an ultrasound to look for ectopic pregnancy.
Abdominal ultrasound is useful, but transvaginal ultrasound is superior in confirming an intra or extrauterine pregnancy, with a sensitivity of 93% and specificity of 97%.1 Together with ultrasound, hCG is a valuable tool for assessing pregnancy. A combination of ultrasound and hCG has a very high sensitivity (96%) and specificity (97%), for EUG.5
Taking these two factors into consideration, it would be reasonable to assume that EUG in this case would not be on the top of the list of a differential diagnosis. Instead, a ruptured hemorrhagic cyst with active bleeding or ovarian torsion would have a higher priority. However, ultrasound is very much operator-dependent, and experience is crucial in diagnosing complex abnormalities.
CONCLUSION
Ultrasound can be considered as the gold standard in the diagnosis of EUG.
REFERENCES
- Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update. 2014;20(2):250-261.
- Bulletins—Gynecology. ACOG Practice Bulletin No. 193: Tubal ectopic pregnancy. Obstet Gynecol. 2018;131(3):91-103.
- Lee Y-A A, Farine G, Lhamon L. Ruptured ectopic pregnancy with a negative urine pregnancy test. J Urgent Care Med. 2013. Available at: https://www.jucm.com/ruptured-ectopic-pregnancy-with-a-negative-urine-pregnancy-test/. Accessed December 6, 2021.
- Marion LL, Meeks GR. Ectopic pregnancy: History, incidence, epidemiology, and risk factors. Clin Obstet Gynecol. 2012;55(2):376-86.
- Alkatout I, Honemeyer U, Strauss A, et al. Clinical diagnosis and treatment of ectopic pregnancy. Obstet Gynecol Surv. 2013;68(8):571-81.
Author affiliations: Andrew Alaya, MD, MSC, Bronovo Hospital, The Hague, Netherlands. Harold Pelikan, MD, Bronovo Hospital, The Hague, Netherlands. The authors have no relevant financial relationships with any commercial interests.
