Published on
Urgent message: Previously undiagnosed diabetes in elderly patients is too frequently a precursor to the diagnosis of pancreatic cancer. Incidental and unexpected diagnosis of diabetes in older patients in urgent care, especially in normal or underweight individuals, should prompt a discussion about vigilant monitoring for other symptoms of malignancy and close follow-up with a primary care provider.
Joshua Russell, MD, MSc, FCUCM, FACEP
CASE PRESENTATION
A 72-year-old woman with a history of hypertension presented to urgent care with complaints of urinary frequency for the past 6 weeks. She denied burning, urgency, abdominal pain, flank pain, fever, and vomiting. Her only medication was lisinopril-hydrochlorothiazide.
Exam
The patient’s vital signs were normal. She had a normal general exam including no abdominal or costovertebral (CVA) tenderness.
Work-up
The patient’s urine dipstick was negative for nitrites, blood, and leukocyte esterase. However, the urine dip did reveal 1+ protein and 3+ glucose. Based on the results of her urinalysis, a fingerstick glucose was obtained which was 280 mg/dL, suggestive of underlying, undiagnosed diabetes.
Based on the age of onset and timing of symptoms, it was suspected that the patient had type 2 diabetes mellitus (DM2). Interestingly, the patient was not overweight. She was started on metformin 500 mg twice daily and referred back to her primary care provider.
CASE CONTINUATION
Per follow-up with her primary care doctor (PCP), diabetes was confirmed with additional laboratory testing. Her dose of metformin was uptitrated in an effort to achieve adequate glucose control. The patient began having abdominal discomfort and bloating shortly thereafter, which was attributed to an expected side effect of metformin. Her PCP recommended continuing the metformin, expecting that the symptoms would improve in time.
Eight months after her initial UC presentation, she began to develop more severe abdominal pain, weight loss, and early satiety. One evening, the patient noted yellowing of her eyes (ie jaundice) and presented to the emergency department where a computed tomography scan of the abdomen revealed a 4 cm mass of the head of the pancreas. A subsequent biopsy confirmed pancreatic ductal adenocarcinoma (PDAC).
The patient received the standard first-line chemotherapy regimen for approximately 4 months without response. She also tolerated treatment poorly. Subsequently, based on the counsel of her oncologist, she enrolled in hospice care.
Diagnosis
Late-onset Diabetes as a harbinger of Pancreatic Cancer
DISCUSSION
Undiagnosed DM2 is incredibly common in the U.S., with an estimated 8 million people unknowingly living with the disease. Increasing insulin resistance is a normal part of the aging process; however, most cases of DM2 will present before age 50.1 Occasionally, older adults may develop DM2. Approximately 1% of patients >50 years of age with new-onset DM2 will be diagnosed with pancreatic cancer within the subsequent 36 months. Of those pancreatic cancer cases, 60% will develop within the first 12 months after onset of diabetes.2
The strong, complex relationship between PDAC and diabetes seems to be one of “dual causality.”3 Concurrent hyperglycemia and increased insulin-like growth factor (IGF) signaling contribute to inflammation and unregulated cellular proliferation, which in turn, increases risk for malignant transformation.1
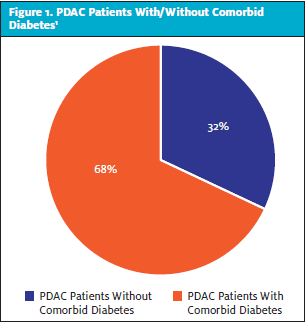
In patients with PDAC and diabetes, the diagnosis of diabetes occurred within the 24 months preceding cancer diagnosis in 74%-88% of cases. Conversely, 68% of patients with PDAC have comorbid diabetes (Figure 1). The relationship is further supported by the observation that 57% of patients with PDAC and DM saw resolution of diabetes after tumor resection.1
The incidence of pancreatic cancer is increasing throughout the world. It is currently the fourth leading cause of cancer-related deaths worldwide and is projected to become the second leading cause of cancer mortality before 2025.4 A primary reason for such high disease-associated mortality is that most cases of pancreatic cancer are unresectable at the time of detection.5 PDAC is the most deadly form of pancreatic cancer, with a 5-year mortality exceeding 90%.1 Hence, a key principle for modifying the mortality of pancreatic cancer is reducing time from onset until detection.
Defining which subset of patients with late-onset diabetes should undergo further screening for pancreatic cancer, and when, has proven to be a challenge. In general, patients who are oldest (ie >70 years) and who have experienced recent weight loss are at the highest risk of having DM2 related to undiagnosed (and unfortunately often clinically undetectable) PDAC.2 This is consistent with the patient’s presentation in this case report.
CONCLUSION
Thankfully, the vast majority of older patients diagnosed with late-onset diabetes (ie, after age 50) will not develop pancreatic cancer. However, as earlier detection is crucial to reduce mortality from the disease, it is useful to educate patients receiving a new diagnosis of diabetes in UC, especially if older and not overweight, about the association with pancreatic cancer and encourage monitoring for worrisome symptoms (eg, upper abdominal pain, early satiety, weight loss) which should prompt immediate re-evaluation.
REFERENCES
- Andersen DK, Korc M, Petersen GM, et al. Diabetes, pancreatogenic diabetes, and pancreatic cancer. Diabetes. 2017;66(5):1103-1110.
- Sharma A, Kandlakunta H, Nagpal SJS, et al. Model to determine risk of pancreatic cancer in patients with new-onset diabetes. Gastroenterology. 2018;155(3):730-739.e3.
- Li J, Cao G, Ma Q, et al. The bidirectional interaction between pancreatic cancer and diabetes. World J Surg Oncol. 2012;10:171.
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913–2921.
- Khadka R et al. Risk factor, early diagnosis and overall survival on outcome of association between pancreatic cancer and diabetes mellitus: changes and advances, a review. Int J Surg. 2018;52:342–346.
Joshua Russell, MD, MSc, FCUCM, FACEP is Editor-in-Chief of JUCM; attending staff physician, NorthShore University Health System (Teaching Affiliate of the University of Chicago); Associate Editor, Urgent Care Reviews and Perspectives Podcast, Hippo Education; and staff physician, Legacy/GoHealth Urgent Care. The author has no relevant financial relationships with any commercial interests.
Read More on Diabetes in Urgent Care
- Original Research: Early Diabetes Screening In The Urgent Care, Part 1
- Original Research: Early Diabetes Screening In The Urgent Care, Part 2
- Diabetes Mellitus: Current Diagnosis, Screening And Management Issues In Urgent Care

