Urgent message: Undiagnosed type 2 diabetes mellitus affects more than 9 million Americans. This first part of a two-part article focuses on evaluation of diabetes screening for the adult urgent care patient in whom diabetes has not been diagnosed, using effective early disease-detection strategies to reduce the long-term burden of diabetes. How this article helps you: by providing data to assist you in deciding about screening in your center.
Introduction
There are now more than 9000 urgent care centers across the United States, and they serve as the main entry point for the medical care of a large percentage of the population.1 Lack of access to primary-care services, medical workforce shortages, lack of health insurance, and lack of time for many Americans have steadily increased the use of urgent care centers for nonurgent problems.2 Historically, urgent care centers focused on providing episodic care for acute illness and injury. In response to recent health-care capacity strain, many urgent care centers have adjusted clinical procedures to provide both acute and chronic care.
Chronic diseases like type 2 diabetes mellitus are occurring in epidemic proportions, creating a demand for urgent care practitioners to diagnose and manage more complex illnesses. With urgent care centers providing a significant portion of primary-care services, communication between the urgent care provider and the primary-care provider (PCP) is essential. Yet the literature demonstrates consistently impaired communication between urgent care providers and PCPs. [Editor’s note: See “‘Why Are You Calling Me?’ The Problem with Patient Transfers in Urgent Care,” at https://www.jucm.com/why-are-you-calling-me-the-problem-with-patient-transfers-in-urgent-care/, and ‘Why Are You Calling Me?’ How to Fix Relationships with Emergency Departments,” at https://www.jucm.com/why-are-you-calling-me-how-to-fix-relationships-with-emergency-departments/.] Urgent care centers must expand and improve current practice standards to incorporate a coordinated effort toward preventative care, primary care, and chronic-disease management.
Background
Diabetes is a leading cause of premature morbidity and mortality.3,4 The economic and health burden continues to grow.5 In 2012, the estimated global prevalence of diabetes was 8.3%, or more than 371 million people living with diabetes, and the projection for 2030 is 552 million adults.5,6 In the United States, the number of cases of diagnosed diabetes has steadily risen over the past few decades, increasing from 23.6 million in 2007 to over 25.8 million in 2011. An estimated 79 million Americans have blood glucose levels in ranges indicating prediabetes or a risk of developing diabetes. In total, the numbers place more than 100 million Americans at risk.7
Some estimate that undiagnosed diabetes affects more than 9 million Americans.7 This number is likely low, because more than 50 million Americans are without health insurance and have little or no access to health care. The Patient Protection and Affordable Care Act is the latest attempt at health-care reform, bringing a projected 32 million newly insured citizens into the health-care system by 2019.2,8 More than half of all currently uninsured citizens do not have a regular source of health care, and many of these individuals likely will gain access to initial care through urgent care centers.2 This influx of patients will provide urgent care centers with the opportunity to obtain more accurate disease-prevalence data through the development and implementation of screening measures to detect chronic diseases such as prediabetes and diabetes.
The total U.S. diabetes expenditure9 reached approximately $48 billion in 2013, and is projected to reach an astonishing $79 billion by 2023. Findings consistently demonstrate a strong link between early diabetes detection and improved health outcomes. The significant health and financial impact supports the pressing need to develop early-detection strategies to reduce the long-term burden of the disease.
Methods
To better understand current diabetes screening strategies in the asymptomatic patient population, we conducted a literature review in PubMed, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Embase, Cochrane Library, and Scopus. Over 10,000 articles across all databases matched the search criteria. Sixteen studies matched the intended project purpose. This comprehensive literature review revealed few descriptions of diabetes screening methods in the asymptomatic population.10,11 High-quality evidence to support the efficacy of diabetes screening was predominantly found in the preoperative setting.10–13
The supported value of diabetes screening in the perioperative setting suggests that future studies specific to diabetes screening in the urgent care environment may yield similar results. Translation of the preoperative study findings to the urgent care setting can be used to (1) establish the feasibility of routine diabetes screening in the asymptomatic population, (2) perform diabetes screening in asymptomatic patients as an intervention to demonstrate a positive relationship between early screening and a reduction in future complications, and (3) prove that to minimize the long-term burden of the disease, providers outside the primary-care specialty must adjust current practice regimens to routinely include screening measures for chronic diseases.
Diabetes Screening
The 16 studies selected for analytical review included evaluation and discussion of unknown hyperglycemia across all practice settings, with a primary focus on the perioperative and operative setting. Researchers who looked at the opportunity for diabetes screening in the preoperative patient found strong support for screening fasting preoperative patients on the day of surgery to reduce the prevalence of undiagnosed diabetes.10–13 Tapp et al found that even among patients who had insurance and recent primary-care visits, nearly one-quarter still had previously unrecognized elevated fasting plasma glucose (FPG) levels identified on the day of surgery.13 Wang et al found that in patients undergoing surgery who are not known to have diabetes, increased preoperative glucose levels are a marker for worse postoperative outcomes.11
Data from this research demonstrated that prediabetes or diabetes would be diagnosed earlier in the disease process in millions of individuals annually through the screening processes described in these studies alone.10 These studies’ findings validate the strong link between early diabetes detection and reduced long-term complications.10–13 Translation of evidence supporting asymptomatic diabetes screening in the preoperative setting can be used to develop methods for early screenings in the urgent care environment. To improve the urgent care provider’s ability to make the diagnosis earlier in the disease process, solutions must be directed at developing screening measures that are adaptable to a variety of practice settings, including fast-paced arenas such as urgent care centers. Urgent care providers are in a unique position to use evidence-based guidelines to identify undiagnosed prediabetes and diabetes in the volumes of patients they treat annually.
Clinical Guidelines
The 2016 American Diabetes Association (ADA) guidelines regarding standards of medical care in diabetes, along with a consensus statement by the American College of Endocrinology and the American Association of Clinical Endocrinologists, serve as evidence-based guidelines for the diagnosis and treatment of prediabetes, diabetes, and comorbidities associated with diabetes.14,15
Even though several high-quality diabetes treatment guidelines are available, they are frequently ignored in urgent care centers.14 One reason seems to be the challenge of adapting these guidelines into a format suitable to the specific practice demands of specialties outside of primary care. Compounding the problem, medical service reimbursement decreases have driven a trend toward shorter visit times to increase patient volume and resultant revenue. Increasing the requirements of urgent care providers to include detection of chronic diseases could result in increased patient wait times and staff overload, in turn negatively impacting buy-in from the health-care team.
Even though guidelines are not fully used by urgent care centers, people will continue to present for primary-care services and require diabetes screening. Urgent care centers must develop new and efficient ways to address the care of these individuals and move toward consistently providing the same preventative-care approaches that would normally occur at PCP offices.
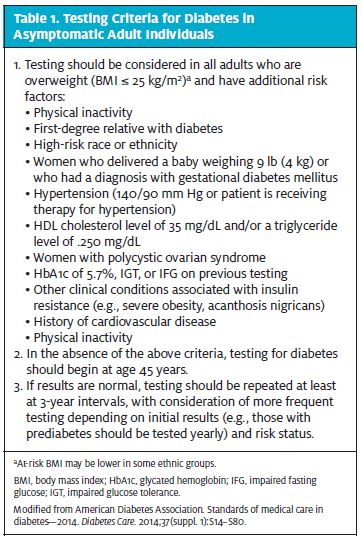
The authors of the 2016 ADA guidelines used high-level, evidence-based research for the recommendations, and the guidelines can be viewed as the gold standard for diabetes screening, diagnosis, and treatment across all practice settings.14 The guidelines address clinical diagnosis and management of diabetes both for symptomatic and asymptomatic individuals. According to the ADA guidelines, screening is to be conducted in all patients 45 years of age and older, and in younger overweight patients with at least one defined risk factor10,14 (Table 1). Measures to create efficient and cost-effective ways to improve the ability of urgent care providers to implement the ADA guidelines will translate to increased disease detection and reduced associated complications. Urgent care use of the guidelines to identify undiagnosed diabetes is not yet well studied or implemented, and this must be addressed.
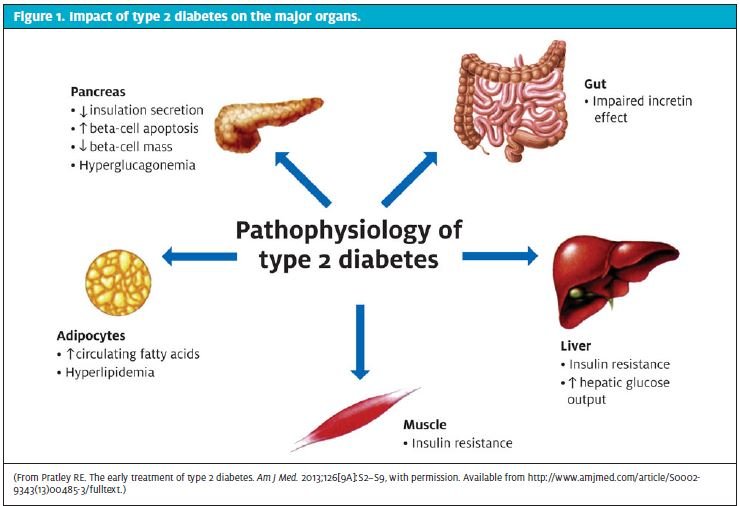
 PathophysiologyApproximately 90% to 95% of those with diabetes have type 2.6,7,14 The disease is a complex and progressive process characterized by chronic hyperglycemia resulting from defects in insulin action and insulin resistance in the peripheral tissues.14 Hyperglycemia is associated with long-term damage to multiple organs, as depicted in Figure 1, with particular effects on the eyes, kidneys, nerves, heart, and blood vessels. The cause of type 2 diabetes is a combination of resistance to insulin action and inadequate compensatory insulin secretory response caused by the gradual decline in pancreatic beta-cell function.14,16
PathophysiologyApproximately 90% to 95% of those with diabetes have type 2.6,7,14 The disease is a complex and progressive process characterized by chronic hyperglycemia resulting from defects in insulin action and insulin resistance in the peripheral tissues.14 Hyperglycemia is associated with long-term damage to multiple organs, as depicted in Figure 1, with particular effects on the eyes, kidneys, nerves, heart, and blood vessels. The cause of type 2 diabetes is a combination of resistance to insulin action and inadequate compensatory insulin secretory response caused by the gradual decline in pancreatic beta-cell function.14,16
Most patients with type 2 diabetes are obese, with obesity itself accounting for some degree of the insulin resistance. The risk of developing type 2 diabetes increases with age, obesity, and lack of physical activity. Type 2 diabetes occurs more often in women with a history of gestational diabetes and in individuals with hypertension or dyslipidemia.14
Classic symptoms of the disease include polyuria, polydipsia, and weight loss, with some patients experiencing polyphagia and blurred vision. Patients with prediabetes and diabetes have an increased incidence of developing atherosclerotic cardiovascular, peripheral arterial, and cerebrovascular disease, as well as hypertension and dyslipidemia.14 A study by Tapp et al demonstrated that individuals with impaired fasting glucose (IFG) and type 2 diabetes often have increased bodily pain and reduced physical functioning, general health, mental health, and vitality at baseline.13
A growing body of evidence suggests that the risk of developing complications is greater with glucose levels beyond established thresholds, and individuals with levels in the prediabetic range are already at risk. The microscopic damage typically starts during the lengthy prediabetic stage and gives rise to a substantial increased risk of developing overt type 2 diabetes in parallel with persistent hyperglycemia.3,12 Although there are currently no approved medication treatment options for prediabetes, the evidence shows that early intervention with lifestyle modifications such as diet, exercise, and weight-loss measures may slow how quickly the disease progresses.3 The duration of glycemic burden is the strongest predictor of adverse outcomes, supporting the need for effective strategies to prevent the progression from prediabetes to diabetes.3,10
Testing for Diabetes
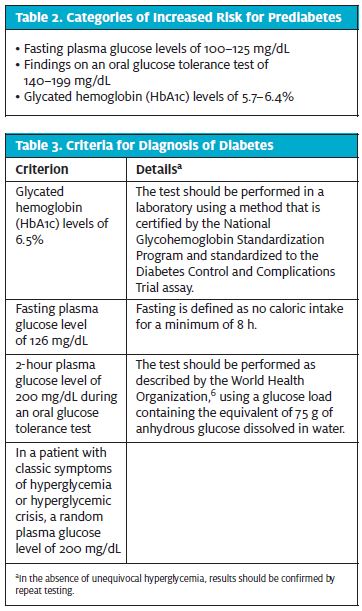
The 2014 ADA guidelines recommend testing to detect type 2 diabetes and prediabetes in asymptomatic adults who are overweight or obese, with a body mass index ≥25 kg/m2, in combination with one or more risk factor for diabetes (Tables 2 and 3). For those who are age 45 years and older, testing should be conducted regardless of body mass index or risk factors. The glycated hemoglobin (HbA1c) test, the FPG test, and the 2-hour, 75-g oral glucose tolerance test (OGTT) are all considered appropriate means for detection of prediabetes and type 2 diabetes. Patients who present to urgent care centers are typically not fasting; therefore, obtaining an HbA1c value is often the best diagnostic option. The ADA recommends that if test findings are normal, the test should be repeated at 3-year intervals. The same tests are used for both screening and diagnosing and can identify prediabetes and diabetes anywhere along the clinical spectrum of the disease process.14
 Making the DiagnosisIn general, diagnosis of diabetes should be made when HbA1c values are ≥6.5%. The test should be performed in a laboratory certified by the National Glycohemoglobin Standardization Program and standardized to the Diabetes Control and Complications Trial assay. Fingerstick HbA1c values should be used only for screening purposes. All patients who test in the prediabetic and diabetic range by fingerstick should undergo standard laboratory testing to confirm diagnosis. An FPG ≥126 mg/dL meets the criteria for diagnosis of diabetes; fasting is defined as no caloric intake for at least 8 hours. A diabetes diagnosis is confirmed when a 2-hour plasma glucose level is ≥200 mg/dL.14
Making the DiagnosisIn general, diagnosis of diabetes should be made when HbA1c values are ≥6.5%. The test should be performed in a laboratory certified by the National Glycohemoglobin Standardization Program and standardized to the Diabetes Control and Complications Trial assay. Fingerstick HbA1c values should be used only for screening purposes. All patients who test in the prediabetic and diabetic range by fingerstick should undergo standard laboratory testing to confirm diagnosis. An FPG ≥126 mg/dL meets the criteria for diagnosis of diabetes; fasting is defined as no caloric intake for at least 8 hours. A diabetes diagnosis is confirmed when a 2-hour plasma glucose level is ≥200 mg/dL.14
Prediabetes is a diagnostic term used to describe individuals who have IFG and impaired glucose tolerance (IGT) on any one of the three standard tests. Those who test in the prediabetes range have a higher risk of developing diabetes.3,12,14 IFG and IGT are linked to obesity, dyslipidemia, and hypertension. Criteria for prediabetes diagnosis14 (Table 3) include IFG levels of 100 to 125 mg/dL, IGT values of 140 to 199 mg/dL, and HbA1c values of 5.7% to 6.4%.
The Debate Over Glycated Hemoglobin
Early detection of diabetes is fundamental in preventing diabetes and its associated complications. Research has shown that the HbA1c test, the FPG test, and the OGTT are all well-established instruments for diagnosing diabetes.14 However, all diabetes-testing methods are imperfect and have unique advantages and disadvantages regarding sensitivity and reliability. A strong body of evidence supports measurement of HbA1c for diabetes screening.3,12,14 The HbA1c value provides a reliable measurement of chronic glycemic control, and is a simple, cost-effective test that can be performed in all health-care environments. One of the main concerns discussed in the literature regarding the HbA1c test is the variation in results and the established threshold recommendations for diagnosis generated from both studies and guidelines.12 Variability is most often attributable to incomplete correlation between average glucose levels in individuals of particular races or ethnicities or to the presence of certain anemias and hemoglobinopathies. Epidemiologic studies responsible for HbA1c recommendations have been conducted in all populations and demonstrate HbA1c cut point generalizability. For patients with abnormal red blood cell turnover, such as during pregnancy, after recent blood loss or transfusion, or in some anemias, the ADA advises that only blood glucose criteria be used to diagnose.14
Suggested methods to reduce variability and improve detection involve the use of lower thresholds of HbA1c values. Studies whose authors caution against the use of HbA1c values for diabetes screening have used high threshold cutoffs that are sensitive enough to identify those with diabetes but not always those with prediabetes. It is equally as important to identify prediabetes as diabetes, and all patients who screen positive for prediabetes or diabetes require repeat testing to confirm their diagnosis. A 6-year community-based prospective study by Choi et al found HbA1c testing to be an effective screening method and a strong predictor of future disease.12 Evidence reveals that using a lower HbA1c cutoff such as 5.9% helped clinicians to identify more individuals with undiagnosed diabetes. Further, individuals with an HbA1c value ≥5.6% were shown to have an increased risk of developing diabetes, independent of other risk factors.12,14
Use of HbA1c values for screening in the general population has several advantages over the FPG test and the OGTT: (1) Specific to the urgent care setting, HbA1c values are preferable because the patient does not have to be fasting; (2) initial screening can be done with a fingerstick HbA1c test, which produces immediate results; and (3) the HbA1c test better indicates chronic fluctuations in elevated glycemic levels, taking into account a 3-month average rather than a snapshot in time.
Connecting Urgent Care with Primary Care
The 2014 Benchmarking Survey of the Urgent Care Association revealed that an average of 75% of urgent care patients have a PCP outside the center, leaving 25% who may be using urgent care centers as their PCP. Only 26% of urgent care centers are affiliated with a multispecialty clinic that provides primary care.1
The association’s 2012 survey demonstrated that 93% of urgent care centers have a standard process in place to help patients find a regular provider, yet only 55% of patients are actually assisted with this task.1 Standard processes in place at some urgent care centers include providing a list of local PCPs and assisting patients in making a future appointment with either an internal PCP or a PCP outside the practice. Urgent care centers’ assistance levels have been found to be either very high or very low, which likely ties into whether the urgent care center formally provides primary care internally.
Lack of access to primary-care services, lack of health insurance, and lack of time for many Americans has resulted in a steady rise in the use of urgent care centers for primary-care services.2 Underuse of evidence-based clinical practices combined with inconsistent PCP referral procedures has historically impacted the connection between urgent care and primary care.1,2 With urgent care centers providing many primary-care services, communication between the urgent care provider and the PCP is essential for continuity of care. This concept is especially critical when urgent care centers provide primary services and diagnose individuals with chronic diseases.
Making the Case for Screening
A growing trend toward walk-in clinics, e-clinics, and telephone provider visits has emerged in response to increased demand for quick, accessible, and affordable care. The urgent care center stands as one of the most evolved and established walk-in clinic models, historically designed to provide only episodic acute care. As the standard in the convenient-care industry, the next task is to improve the consistency with which walk-in clinics coordinate with PCPs and to improve the ability to provide comprehensive preventative and primary-care services.
 What’s NextPart 2 of this article (in the October 2016 issue) will review the results of an urgent care center pilot study implementing a structured, multidisciplinary pathway to evaluate and identify undiagnosed prediabetes and diabetes. The study population included adult patients with no previous diagnosis of prediabetes or diabetes who presented for care at Synergy Health Center and Urgent Care, a community-based multispecialty clinic and urgent care center in Pleasanton, California. The purpose of the project was to demonstrate a guideline specific to urgent care for improving early diabetes screening methods that do not impact patient-encounter times, clinic efficiency, or cost. Study aims included increasing detection rates of undiagnosed prediabetes and diabetes, improving referral between urgent care centers and primary care, and demonstrating the feasibility and usability of diabetes screening measures in the urgent care environment.
What’s NextPart 2 of this article (in the October 2016 issue) will review the results of an urgent care center pilot study implementing a structured, multidisciplinary pathway to evaluate and identify undiagnosed prediabetes and diabetes. The study population included adult patients with no previous diagnosis of prediabetes or diabetes who presented for care at Synergy Health Center and Urgent Care, a community-based multispecialty clinic and urgent care center in Pleasanton, California. The purpose of the project was to demonstrate a guideline specific to urgent care for improving early diabetes screening methods that do not impact patient-encounter times, clinic efficiency, or cost. Study aims included increasing detection rates of undiagnosed prediabetes and diabetes, improving referral between urgent care centers and primary care, and demonstrating the feasibility and usability of diabetes screening measures in the urgent care environment.
Conclusion
Diabetes is a disease of huge health consequence, and continued efforts to investigate screening options in a variety of health-care settings is required. Data in the literature consistently reveal that a high proportion of patients with a new diagnosis of prediabetes or diabetes already have comorbidities and complications.14,16 For this reason alone, interventions directed at early screening to identify those with impaired glycemic control are imperative. Further research is required to determine the feasibility of diabetes screening in fast-paced environments such as urgent care centers.
Because the U.S. health-care system is faced with severe capacity strain and because the implementation of the Patient Protection and Affordable Care Act has brought an influx of millions of newly insured citizens, the demand for urgent care centers to provide primary-care services and manage chronic diseases is critical. The best way to address this problem is to develop modalities to reach those who need primary-care services but have access only to urgent care centers for this type of care. To accomplish this goal, urgent care centers and urgent care providers must consider adjusting current practice standards and clinical procedures.
Acknowledgments
We thank Carley Kalafut, BS, and George Gigounas, JD, for assistance in revising the manuscript.
Citation: Clark SR, Wilson MR. Original research: early diabetes screening in the urgent care, part 1. J Urgent Care Med. September 2016. Available at: https://www.jucm.com/original-research-early-diabetes-screening-urgent-care-part-1/.
References
- Urgent Care Association. 2014 Urgent Care Benchmark Survey Results. Naperville, IL: Urgent Care Association. © 2014 [accessed 2015 December 8]. Available from: http://www.ucaoa.org/?UCBenchmarking
- Kaissi A. Primary care physician shortage, healthcare reform, and convenient care: Challenge meets opportunity? South Med J. 2012;105:576–580.
- Pratley RE. The early treatment of type 2 diabetes. Am J Med. 2013;126(suppl 1):S2–S9.
- Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14.
- International Federation of Diabetes. IDF Diabetes Atlas. 5th edition. Brussels, Belgium: International Diabetes Federation; 2011 [accessed 2013 May 8]. Available from: http://www.diabetesatlas.org/component/attachments/?task=download&id=116
- World Health Organization. Diabetes fact sheet 312. Geneva, Switzerland: World Health Organization [published 2011 January; last updated 2016 June; accessed 2013 May 8]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
- Centers for Disease Control and Prevention (CDC). National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011 [accessed 2013 May 8]. Available from: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf
- Goldman LE, Chu PW, Tran H, et al. Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med. 2012;43:142–149.
- DeVol R, Bedroussian A. An unhealthy America: the economic burden of chronic disease. Santa Monica, CA: Milken Institute; © 2007 [accessed 2010 July 4]. Available from: http://assets1b.milkeninstitute.org/assets/Publication/ResearchReport/PDF/chronic_disease_report.pdf
- Sheehy AM, Benca J, Glinberg SL, et al. Preoperative “NPO” as an opportunity for diabetes screening. J Hosp Med. 2012;7:611–616.
- Wang R, Panizales MT, Hudson MS, et al. Preoperative glucose screening tool in patients without diabetes. J Surg Res. 2014;186:371–378.
- Choi SH, Park KS, Kim TH, et al. Hemoglobin A1c as a diagnostic tool for diabetes screening and new-onset diabetes prediction a 6-year community-based prospective study. Diabetes Care. 2011;34:944–949.
- Tapp RJ, O’Neil A, Shaw JE, et al; AusDiab Study Group. Is there a link between components of health-related functioning and incident impaired glucose metabolism and type 2 diabetes? The Australian Diabetes Obesity and Lifestyle (AusDiab) Diabetes Care. 2010;33:757–762.
- American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care. 2016;39(suppl 1):S14–S112.
- Garber AJ, Abrahamson MJ, Barzilay JI, et al; American Association of Clinical Endocrinologists. AACE comprehensive diabetes management algorithm 2013. Endocr Pract. 2013;19:327–336.
- Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Affairs. 2010;29:1630–1636.
