Differential Diagnosis
- Atrial flutter with 2:1 conduction
- Atrial fibrillation with rapid ventricular response
- Sinus tachycardia
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrioventricular reentrant tachycardia (AVRT)
Diagnosis
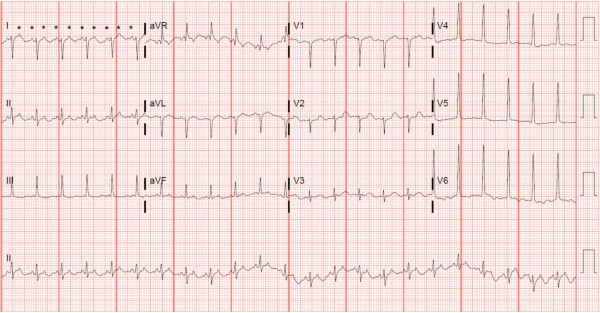
This patient was diagnosed with atrial flutter with 2:1 conduction. The ECG shows a regular narrow-complex tachycardia with a rate of 160 beats per minute. There is a left axis deviation with left ventricular hypertrophy (as evidenced by the tall R wave in aVL), and T-wave inversions in I and aVL consistent with a left ventricular strain pattern. (See the February 2020 issue of JUCM for further clarification of the left ventricular strain pattern).
On initial assessment of this ECG, atrial activity is not readily apparent, making it difficult to distinguish among atrial flutter, sinus tachycardia, and other supraventricular tachycardias such as AVNRT or AVRT. In this case, the astute clinician has two options:
- A trial of an atrioventricular node blocker (eg, adenosine) will “unmask” atrial activity if present, or
- A simple strategy to check “the Lewis lead,” which might reveal the underlying rhythm
Developed and described in 1913 by Sir Thomas Lewis, the Lewis lead is a unique configuration of the ECG electrodes over the atrium that allows for the amplification of atrial activity.2
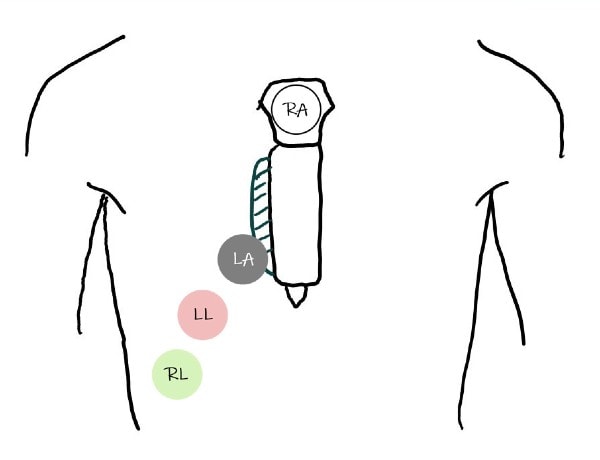
To evaluate the Lewis lead on an ECG, move the right arm (RA) electrode to the manubrium, the left arm (LA) electrode to the fifth intercostal space on the right sternal border, and the left leg (LL) electrode to the right lower costal margin (Figure 2). With the electrodes in this position, lead I will best illustrate atrial activity.3,4 This positioning centers lead I over the right atrium, magnifying its activity.
When the Lewis lead was performed in our case, flutter waves were clearly present in lead I (and lead II), cinching the diagnosis of atrial flutter with 2:1 conduction (Figure 3).
While this article demonstrates the benefit of a Lewis lead to aid the diagnosis of undifferentiated regular, narrow-complex tachycardias, this technique may also be used with wide-complex tachycardias. In these cases, performing a Lewis lead ECG allows the clinician to identify atrioventricular dissociation and make the diagnosis of ventricular tachycardia in stable patients.5
Learnings/What to Look for
- Hidden P-waves in regular narrow-complex tachycardias can be unmasked by adenosine or a Lewis lead ECG
- After reorganizing electrodes in the Lewis lead configuration, obtain another ECG and look at lead I for clues about the underlying atrial activity
Pearls for Urgent Care Management
- In stable patients with no obvious atrial activity on ECG, a Lewis lead can help you make the diagnosis and treat accordingly
- Patients with atrial flutter with rapid ventricular response typically would benefit from transfer to a facility with cardiology services available, but making the diagnosis and stabilizing before transfer is paramount
References
1. Cooper B, Giordano J, Fadial T, Reynolds C. Lewis lead. In: ECG Stampede: A Case-Based Curriculum in Electrocardiography Triage. Houston, TX: Null Publishing Group; 2021:159-161.
2. Lewis T. Auricular fibrillation. In: Clinical Electrocardiography. 1913:86-97.
3. Bakker ALM, Nijkerk G, Groenemeijer BE, et al. The Lewis lead. Circulation. 2009;119(24).
4. Huemer M, Meloh H, Attanasio P, et al. The Lewis Lead for detection of ventriculoatrial conduction type. Clin Cardiol. 2016;39(2):126-131.

