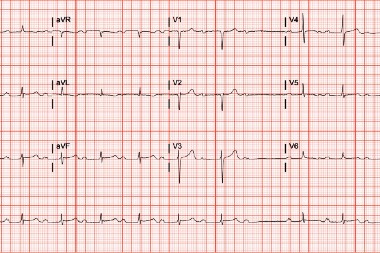
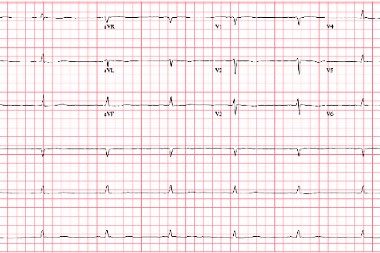
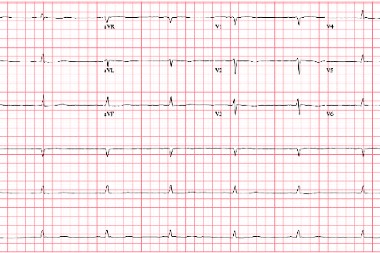
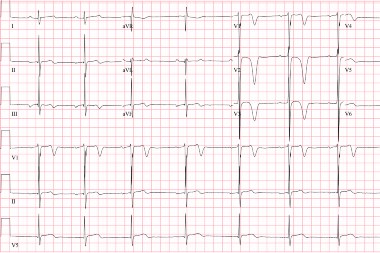
A 38-year-old man present to urgent care complaining of pain around his entire pelvis after a fall on a slippery floor at home. Imaging is obtained. Review the image taken and consider what your diagnosis and next steps would be. Resolution of the case is described on the following page.
Read More