Urgent message: Urgent care centers can execute and implement innovative ideas to ameliorate overcrowded Emergency Rooms. The creation of a mobile health diversion program to transport low acuity conditions to urgent care instead of a hospital emergency department can improve population health and reduce healthcare cost; providing the opportunity to leverage value-based care by targeting the triple aim (reducing cost, increasing patient satisfaction, and improving outcomes) while freeing up the emergency medical system services.
Cesar Mora Jaramillo, MD, FAAFP, FCUCM
Citation: Jaramillo CM. Reducing low-acuity preventable emergency room visits by utilizing urgent care center services via mobile health unit diversion program. J Urgent Care Med. 2022;16(6):35-37.
INTRODUCTION
Volatility and continuously rising costs in the United States healthcare system have created a marketplace in which urgent care centers can play an essential role by helping to reduce cost, increase patient satisfaction, and improve outcomes.
At the same time, overwhelmed emergency departments need help in minimizing low-acuity/unnecessary usage while reducing cost and assisting in health disparities.
According to the Centers for Medicare and Medicaid Services (CMS), healthcare spending is expected to increase to 19.4% from 17.9% in the next 7 years, giving UCCs the opportunity to step up in cost-reducing actions.1
Emergency departments are overused in multiple ways—varying levels of severity including acute conditions, acute on chronic illnesses, mental health, substance abuse, and prescription refills, among others.2
There is evidence showing patients using the emergency room for complaints that could be treated in settings that represent a cost-effective environment (including urgent care or patient-centered medical homes).3 Initiatives to explore how patients with low-acuity conditions can be transported to a more appropriate setting such as urgent care instead of a hospital ED should be considered. This could reduce ED utilization for nonemergent conditions while also reducing overall healthcare cost without affecting patient satisfaction.
Description
The Providence (RI) Fire Department receives approximately 33,000 medical-related calls in a year, of which 7,500 are dispatched as basic life support (BLS) and approximately 14,000 are transported and billed as BLS calls. About 39 calls qualified as BLS are received in a period of 24 hours.4
The implementation of the Mobile Health Unit initiative provides patients who have non-life-threatening conditions the opportunity to receive immediate care in an appropriate ambulatory care setting (urgent care) while freeing up the EMS system to respond to severe/life-threatening emergencies.
Two lieutenants from the PFD were assigned to the Mobile Health Unit starting late August in 2019. When a patient calling 911 is identified as having a non-emergency condition or complaint, the crew will assess the patient in the field, communicate with a registered nurse at an urgent care center, and may transport the patient to the facility instead of the ED.
In this article we discuss how an innovative federal qualified health center facility (Providence Community Health Centers) managed to create a program mobile health unit” in collaboration with state health insurance (Neighborhood Health Plan of RI) and the city department. The initiative consisted of transporting low-acuity or BLS calls to immediate appropriate quality care in an urgent care center while ameliorating the EMS system and preventing avoidable ER visits.
The Express Clinic manages close to 25,000 visits a year while the entire organization serves a total of approximately 60,000 patients (seeking primary care), predominantly Hispanic/Latino. The population served by the community health center (CHC) includes 90% of households that are under 200% of the federal poverty level (FPL) and a significant proportion of uninsured patients are undocumented immigrants.
METHODOLOGY
Retrospective Descriptive study
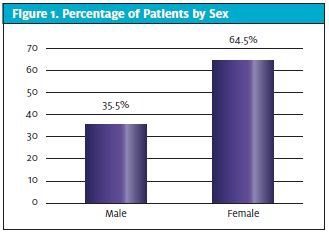
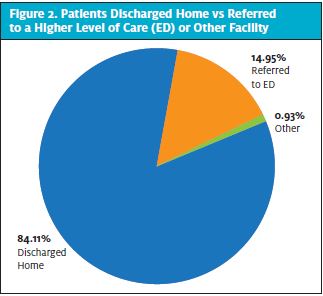
Data were retrospectively reviewed from the urgent care department of a Federally Qualified Health Center (FQHC) in Providence, RI to determine the percentage of preventable ER visits via the innovative Mobile Health Unit. A query of the electronic medical record database identified 107 patients who were transported to urgent care after calling 911 between August 26, 2019 and March 16, 2020. (The program was put on a hold due to the COVID-19 pandemic.) The data reviewed included age, sex, chief complaint, diagnoses, referral to ED, other referrals/disposition, and diagnoses of any psychiatry condition and/or substance use reported in the visit note, problem list, or the under the diagnosis history prior to the EMS transported visit.
The objective of analyzing the data was to study if the mobile diversion program successfully prevented avoidable ER visits. In addition, data were reviewed to investigate the percentage of any psychiatric conditions and/or substance use within the population studied. The Providence Community Health Centers approved the project.
RESULTS
A total of 107 patients were transported to Express (UCC) after calling 911 between August 26, 2019 and March 16, 2020. Of these patients, 69 were female (64.5%). (See Figure 1.) The age of the patients seen in urgent care ranged from 16 years to 81 years with a median of 40.
Of those 107 patients, 90 (84.1%) were discharged home and 16 (14.9%) were referred for higher level of care to a local ED. One individual was referred to a detox facility. (See Figure 2.)
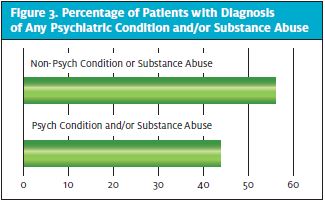
Among the 107 patients transported to the urgent care facility for health services, 47 (43.9%) had a diagnosis of any psychiatric condition and/or substance use. (See Figure 3.) Of these patients 19 (40.4%) had a diagnosis of depression and/or other psychiatry condition. In terms of substance use, seven patients (14.8%) of the 47 had a diagnoses of only alcohol use and four (8.5%) of only cannabis use.
The most common chief complaints observed were pain in 47 patients (43.9%) and GI symptoms in 21 patients (19.6%). Pain was identified as musculoskeletal-related in 28 of those 47 patients (59.9%); nine patients (19%) complained of abdominal pain.
Additionally, out of the 107 patients transported to Express via Mobile Health Unit, 30 were diagnosed with infectious diseases (28%).
DISCUSSION
Innovative federal qualified health center facility (Providence Community Health Centers) was successful at executing a program to prevent avoidable emergency room visits while freeing up the EMS system to respond to true emergencies and life-threatening conditions.
In the United States, approximately 13% to 27 % of ED visits can be addressed in ambulatory settings (including urgent care Centers). Diverting these patients to the appropriate setting for care could decrease healthcare costs by $4.4 billion.5
Misuse and/or overuse of 911 calls for nonemergencies can overwhelm the emergency medical system services, threating to increase ambulance wait time and adding cost to city services. The consequences of such a rise in EMS response time intensifies the risks of serious outcomes or mortality. Organizations should invest in understanding the population/communities and investigate the drivers for patients to seek care in local EDs via 911 calls.
Redirection of nonemergency 911 callers to more appropriate sources of medical care like UCCs can be accomplished. During the 26 weeks of the Mobile Health Unit Diversion program, 8.4 out of every 10 patients diverted to a UCC were discharged home—consequently, avoiding an ED visit while patients were treated in a cost-effective setting. This initiative offered an alternative to low-acuity 911 calls or a trip to the ED.
Some of the studied drivers for ED overuse are low incomes/poverty, no health insurance, lack of access to timely care services, and financial and legal obligations by hospitals to treat all patients who arrive in the ED.2
A large portion of ED visits fall into the category of “avoidable” use resulting from patients seeking nonurgent care or ED care for conditions that could have been treated and/or prevented in other settings, like UCCs.2
While some medical conditions have been associated with ED overuse, this study shows an association of pain, infectious diseases, and mental health with ED usage. In collaboration with key stakeholders, these avoidable visits can be prevented without compromising patient accessibility or quality of care.
Adults with psychiatric conditions and/or substance use issues are more likely to utilize the ED for care for medical conditions in comparison with patients without mental health disorders. The Agency for Healthcare Research and Quality (AHRQ) states that “from 2007 to 2013, the overall rate of emergency department visits with a principal diagnosis related to mental health, alcohol, or substance abuse increased from 1,527.8 to 1,883.0 per 100,000 population nationwide.”6
Organizations are stepping up with actions to assist in providing this much-needed help and decrease ER over use. The New Haven Community Health Care Van study (mobile needle exchange–based healthcare delivery system) was associated with a decline of more than 20% decline in ED visits among injection-drug users.7
The Mobile Health Unit study shows a high prevalence of psychiatric conditions and substance use among the patients who were transported to a UCC after calling 911. Approximately 4.3 in 10 patients had a mental health and/or substance use condition. Addressing these risk factors in our communities is paramount to decreasing health costs. Access to integrated behavioral and expanding services (accessibility) are some of the strategies CHCs are implementing to leverage a value-based approach, managing the cost of care for this specific patient population. Thus, a substantial amount of money could be saved annually by eliminating avoidable ED use for mental health conditions.
The struggle of communities to manage the overwhelmed 911 system is evident. Urgent care medicine continues to expand in the United States, offering accessibility, quality, and substantial cost reduction of healthcare services. UCCs are capable of linking patients to greatly needed preventative health services and offer a setting to potentially reduce avoidable ER visits. Furthermore, urgent cares provide other opportunities for engagement and education for patients in a setting other than the ED.
More initiatives and research into programs with focus in diverting patients away from ERs are needed.
CONCLUSION
Urgent care centers play an essential role in providing immediate services while offloading overcrowded and high-cost emergency department care. This study shows how UCCs fit in the national value-based care and population health while contributing to an efficient low-cost high-quality healthcare system. UCCs can offer an effective alternative response and prevent unnecessary ED visits by providing care to patients who call 911 with low-acuity complaints.
Patients need (and deserve) access to high-quality care in a timely manner. This includes access to urgent care centers for nonemergent acute conditions. This can be accomplished by intertwining key stakeholders and connecting/transporting patients to appropriate care settings.
The Mobile Health Unit Diversion program supports the idea of a well-designed community/mobile-integrated health intervention that can be effectively executed while ameliorating overcrowded ERs of unnecessary visits and freeing up EMS services to response to severe/life-threatening emergencies.
REFERENCES
- National Health Expenditure Projections 2018-2027. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/ForecastSummary.pdf. Accessed August 12, 2020.
- New England Healthcare Institute. A matter of urgency: reducing emergency department. Available at: https://www.nehi-us.org/writable/publication_files/file/nehi_ed_overuse_issue_brief_032610finaledits.pdf. Accessed August 12, 2020.
- Preventing unnecessary ER visits to reduce health care costs. Fractal. Available at: https://fractal.ai/preventing-unnecessary-er-visits-to-reduce-health-care-costs/. Accessed August 12, 2020.
- Providence Fire Department Mobile Health Unit. City of Providence. Available at: https://www.providenceri.gov/mobile-health-unit/. Published February 5, 2020. Accessed August 12, 2020.
- Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J Healthc Manag. 2013;58(6):412-427.
- Chartbook on Care Coordination. AHRQ. Available at: https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/carecoordination/measure2.html. Accessed August 12, 2020.
- Pollack HA, Khoshnood K, Blankenship KM, Altice FL. The impact of needle exchange-based health services on emergency department use. J Gen Intern Med. 2002;17(5):341-348.
- EMSWorld. Good News Care Center launches ER diversion program. EMS World. Available at: https://www.emsworld.com/article/10373536/good-news-care-center-launches-er-diversion-program. Published April 13, 2011. Accessed August 12, 2020.
- Daly R. Preventable ED use costs $8.3 billion annually: analysis. Available at: https://www.hfma.org/topics/news/2019/02/63247.html. Accessed August 12, 2020.
- Urgent Care Association. Urgent Care Industry White Paper. The essential role of the urgent care center in population health. November 2019. Available at: https://www.ucaoa.org/Resources/Industry-Reports/White-Paper. Accessed February 11, 2022.
- Imig D. Radar Evaluation Report. Memphis Data Partners. February 2018. Available at: www.memphisdatapartners.org.
Author affiliations: Cesar Mora Jaramillo, MD, FAAFP, FCUCM, Providence Community Health Centers; Warren Alpert Medical School Brown University; College of Urgent Care Medicine. The author has no relevant financial relationships with any commercial interests.
