Urgent message: Follow-up after a patient visit is essential to the continuum of care and to the perception of customer service. Especially in the urgent care setting, where providers may have no ongoing relationship with a patient, the most basic office practices (eg, collecting accurate and accessible contact information) can seem deceptively simple but are of critical importance.
Jimmie Toler, MSN, NP-C, Emily E. Johnson, PhD, and Barbara J. Edlund, PhD, ANP, BC
Introduction
Continuum of care is synonymous with appropriate care. In the urgent care environment, this continuum includes the ability to follow up by telephone after care has been rendered in the clinic environment. However, the ability to follow up is often hampered by inaccurate contact information. While this may be due to out-of-date phone numbers or illegible information provided by the patient, the importance of accurate contact information must be appreciated by the staff. This quality improvement project evaluated the impact of easily implemented clinic interventions designed to improve patient telephone follow-up rate.
With this in mind, we sought to answer a key question with profound clinical implications: Will patient and staff awareness of the importance of accurate contact information through education, posters, and changes in the intake form increase contact information accuracy and therefore telephone follow up rate?
Background
Discussions with management and staff of a locally owned and operated clinic were conducted in an effort to identify a process or procedure of concern. One consensus was concern regarding the ability to follow up with patients after treatment.
This concern varied based upon the role of each staff member. Medical assistants who conducted a majority of these contact attempts expressed frustration due to the amount of time required to try to find alternative methods of contact. Management expressed concern over the correlation of follow-up and customer satisfaction. Providers recognized that the ability to follow up allows for more appropriate care and decreases liability.
An initial review of medical records demonstrated an inability to follow up due to inaccurate contact information in >5% of contact attempts. While this was actually less than the level perceived by staff members, all felt that improvement would be beneficial.
The next question was how best to improve follow-up with the resources at hand.
“Healthcare” is a continuum provided at a variety of levels based on both real and perceived patient concerns. The urgent care setting typically addresses concerns that the patient believes warrant immediate evaluation and treatment, yet are not severe enough to require care at an emergency room. Patient expectations may not always be realistic. However, all patients rightfully expect quality care. Clinical quality includes the timely follow-up of findings, test results, and, when appropriate, referral to a higher-acuity facility.1 Following up with patients by telecommunication has long been demonstrated to increase outcomes, as evidenced by nurse-led systemic telephone follow-up which improved health-related quality of life for patients after myocardial infarction to expediting primary care follow up of patients after discharge from the emergency room.2,3
Failure to follow up is a leading cause of malpractice claims. Many legal firms exist solely as an extension of the current medical model, and they cast a broad net to filter for alleged wrongdoing and negligence. The urgent care setting is ripe for this “shotgun” approach, to include the following concerns: misdiagnosis, lack of supervision, failure to diagnose, and failure to monitor care. Timely follow-up by telephone may improve patient satisfaction, recognize a health status change, and minimize claims and lawsuits.
Purpose
The purpose of this quality improvement project was to improve the accuracy of patient contact information in order to increase the follow-up contact rate after being seen in the urgent care clinic.
Setting/Sample
This initiative was completed at a stand-alone urgent care clinic in the coastal southeastern United States. A majority of the patients treated reside in the local area, with many viewing the clinic and staff as their primary care. Many others utilized the urgent care on an as-needed basis and sought care only for acute concerns; this includes a transient group who were in the area (or passing through) on vacation. The sample included 1,235 patients seen in this urgent care clinic for a period of 2 months prior to interventions and 1,316 patients after implementation of the intervention. Patient ages varied from as young as 2 years old to octogenarians.
Framework
The Deming Model of the plan-do-check-act (PDCA) cycle is a well-known method for quality improvement.4 This continuous process consisted of the following steps:
- Plan: A review of processes and chart audits was conducted in an effort to identify probable causes for inability to contact patients for telephone follow-up after treatment. The following were identified for interventions:
- Increase patient awareness of the importance of accurate contact information
- Edit the patient registration form, clarifying the area delineated for acquisition of this information
- Do: The project director (PD) created posters for the patient waiting area and exam rooms emphasizing the importance of accurate contact information. The PD also edited the existing patient registration form to emphasize and provide appropriate space for the collection of contact information. With the review and approval of the clinic manager, the PD had a local printer produce the posters and registration forms.
- Check: Patient contact rates were compared pre- and postintervention.
- Act: Improvement in clinic operating procedures are an ongoing process. Interventions found to benefit patient care will become standard operations, whereas processes that offer no clinical or administrative benefits will be reviewed for improvement or discontinuation.
Interventions
Interventions were directed toward staff and patient. First, a review of the form used to obtain patient information revealed the area designated for the patient to write their telephone number may have been insufficient to provide legible information. This area also was located in the middle of the form, midway through various demographic, employer, and health information. This negatively impacted collection of accurate information by minimizing the importance of this information to the patient. The intervention moved this portion of the form to the beginning of the document, with a slightly larger font and additional room for pen and ink input by the patient. This also engaged the patient input earlier during form completion, when patients may be more alert and focused. If other areas of the form are found to be inaccurate or illegible, these concerns may be corrected later by telephone as long as the contact information is accurate.
The second intervention was directed toward patient awareness of the importance of accurate contact data. The purpose of having accurate contact information may not be fully realized by the patient, or not viewed as important in the urgent care setting because patients may anticipate never returning to that provider. Patients who had previously utilized the services of the clinic may also have changed phone numbers (a more frequent occurrence in today’s transient communications and technology environment).
Patient awareness posters were created to emphasize the importance of accurate follow-up information to address the following needs:
- Patient follow-up to evaluate response to treatment
- Review of laboratory results obtained during the initial visit
- Review of radiological findings which may not have been apparent during the initial reading or that become available after radiology over-read
- Treatment recommendations or changes to recommendations based on these additional results or response to interventions
These posters were developed by the PD and clinic staff, printed by a local printing company, and placed in the patient waiting area and exam rooms.
Staff education alerted the staff to these changes, and reinforced the importance of accurate contact information. Staff were encouraged to engage in discussion with patients to ensure this information was up to date. This discussion period was also an opportunity to ensure patients understood the impact of having accurate and up-to-date contact information.
Data Collection
A staff member attempts to contact patients approximately 48 to 72 hours after the patient was seen in the clinic. This contact is typically initiated by a medical support person, advanced practitioner, or physician based on the anticipated purpose of the follow-up. This follow-up is conducted by phone using the contact information on file within the electronic medical record demographic section. A summary of this contact is chronicled as an addendum to the original chart note. If patient follow-up was not completed, the reason for this failure is also noted in the addendum. Data were collected utilizing the information found within this addendum for each patient treated at the clinic for 60 days prior to and after interventions.
Data Analysis
Patient follow-up addenda were reviewed for each of the days prior to and after interventions for a period of 56 days. Not all patient encounters for each clinical day required follow-up; thus, some encounters were not included in the analysis. These encounter types included office visits for simple exams, immunizations, and labs. Patient encounters that involved patient care were reviewed for follow-up contact notes. Patient visits with inaccurate contact information were divided by total patient visits to provide a percentage of patient follow-up attempts which were not able to be completed due to inaccurate contact information. This percentage of the pre-interventional contact failure rate was compared with the postinterventional rate, in order to evaluate impact of the intervention.

Results
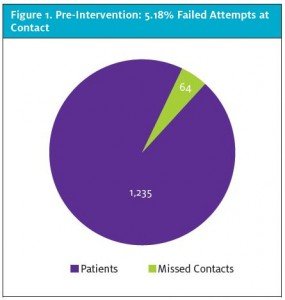
A review of 1,235 applicable patient charts prior to interventions demonstrated a failure to follow up due to inaccurate contact information for 64 patients, or 5.18% (Figure 1). Postintervention data for 1,331 patients indicated a failure to follow up due to inaccurate contact information for 15 patients, or a 1.13% failure rate (Figure 2). A comparison of pre- and postintervention numbers of patients with inaccurate contact information indicated a decrease in follow-up failure rate of 4.05%, or an improvement in follow-up of 78.19%.
Discussion
The beginning of any attempt to improve care delivery is recognizing the need or desire to provide a better service. This area for improvement was recognized by a discussion with management and staff attempting to identify process concerns. Though the concern varied based upon clinic role, the issue was the same. A review was completed in order to identify a process by which to quantify the current status and impact of any interventions.
After the current patient follow-up rate was established, interventions were implemented which were anticipated to improve contact accuracy through a process of simple changes to the intake form, staff training, and patient education. A review of data was again completed; this demonstrated the effectiveness of these interventions.
Conclusion
An improvement process to provide better customer service and improve clinical care need not involve an expensive intervention implemented through a random control process. An open discussion with members of the staff is typically all that is needed to identify concerns. Attempts for improvement should be completed utilizing one of the numerous well validated plans in order to better demonstrate changes.
References
- Ayers AA. Post-visit follow-up calls: improving patient satisfaction, center profitability and clinical outcomes. J Urgent Care Med. 2013. Available at: https://www.jucm.com/post-visit-follow-up-calls-improving-patient-satisfaction-center-profitability-and-clinical-outcomes-2/2/. Accessed July 28, 2017.
- Hanssen T, Nordrehaug J, Eide G, Hanestad B. Improving outcomes after myocardial infarction: A randomized controlled trial evaluating effects of a telephone follow-up intervention. Eur J Cardiovasc Prev Rehabil. 2007;14(3): 429-437.
- Biese K, Lamantia M, Shofer F, et al. A randomized trial exploring the effect of a telephone call follow-up on care plan compliance among older adults discharged home from the emergency department. Acad Emerg Med. 2014;21(2):188-195.
- Johnson C. The Benefits of PDCA. Quality Progress. May 2002. Available at: http://rube.asq.org/quality-progress/2002/05/problem-solving/the-benefits-of-pdca.html. Accessed July 28, 2017.
