Urgent Message: Many Institutions have established guidelines regarding when individuals can return to their regular activities after recovering from COVID-19. Where children and schools are concerned, it’s unclear what the role of testing is (or should be).
Katharine Miao, MD, FACEP; Frank Illuzzi, MD, FACEP, CPE; and Alexander Hwang
Citation: Miao K, Illuzzi F, Hwang A. Prolonged duration of pediatric COVID-19. J Urgent Care Med. 2021;15(5):23-25.
Introduction
Since the outbreak of the SARS-CoV-2 virus within the United States early in 2020, the immediate impact of the pandemic was to trigger a wave of school closures in the initially hardest hit areas. School closures expanded across the country rolling into the traditional summer vacation. During this time period, most children were in an unprecedented state of social isolation in comparison to previous years. The mental health challenges children in isolation face have been raised by alarmed parents, physicians, and health officials.1,2
There has been extensive debate as to when children can safely return to school if they contract coronavirus, with some daycares and even schools requesting a negative PCR test as “a test for cure” after an initial positive test. Current literature has reported extended time periods where patients may continue to test positive even if otherwise appearing healthy.3 Requiring test of cure is not currently recommended by the Centers for Disease Control and Prevention and poses significant long-term social and economic risk both for the parents and the children who may lag behind their peers in educational and social opportunities.
Objective
To determine the mean length of time a pediatric patient may continue to test positive for SARS-CoV-2 virus via a polymerase chain reaction (PCR) n) test after an initial positive test.
Data Source
Testing data were drawn from CityMD’s 130 locations in the New York City metropolitan area.
Study Selection
A retrospective observational study using anonymized chart review of the pediatric population.
Methods
We examined testing results for COVID-19 via PCR in the pediatric population ages 0-17 years at CityMD, with 130 sites in the metro New York City area, during a 6-month period from March 9, 2020 through September 7, 2020.
All patients were accompanied by a guardian who requested a COVID-19 PCR test at the time of visit. All testing was performed at the discretion of the treating provider in accordance with local and state guidelines at the time of evaluation. Patients were examined by a
clinician wearing an N95 and appropriate personal protective equipment (PPE). Tests were obtained from nasopharyngeal swab specimens, transported in VCM (UTM) medium (green-top) tube, for SARS-CoV-2 RNA (COVID-19), Qualitative NAAT testing. All specimens were submitted to commercial laboratories for processing. All repeat positive PCR by medical record number were then sorted by age by the in-house data analytics team and stratified by ICD code. Anonymized charts were then validated to assess for any reports of symptoms which would suggest COVID-19-related illness. As this was a retrospective analysis on anonymized data, an IRB waiver was obtained from Solutions IRB.
Main Outcome and Measures
The primary finding was that the mean length of time that patients continued to show positive PCR tests was 17 days. The median length of time was 20 days. The maximum length of time was 61 days. The range was 6 to 61 days.
Results
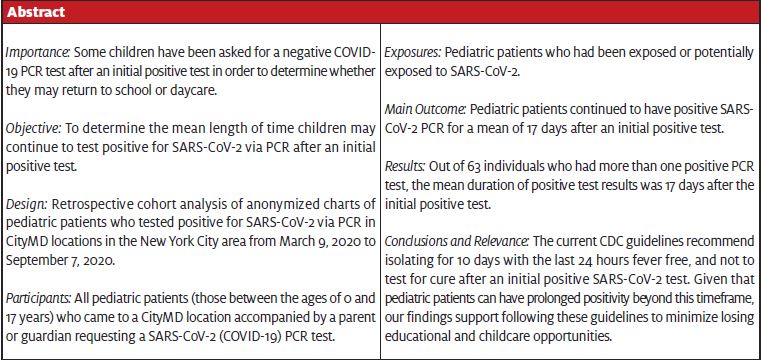
There were 1,282 positive tests out of a total of 45,373 pediatric PCR tests during the study period, for a total positivity of 2.8% in the pediatric population. For relative comparison, there were approximately 933,520 PCR tests done during the same time frame in all age categories. Of these, 43,268 were positive for an overall positivity of 4.6%. This is consistent with our previously reported research that during a time of school closure the pediatric positivity rate was significantly lower than that of the overall population.4 Of the 1,282 pediatric positives, 63 individuals were found to have more than one repeat positive PCR. We found a mean age of 12.0 years in the repeat positive pool compared with the overall pediatric population tested at 11.7 years of age. The median interval between two positive tests was 20 days, and the mean was 17 days. The maximum duration a patient continued to test positive was 61 days. (Figure 1.)
Discussion
This study was a retrospective analysis and chart review on a cohort of repeat PCR-positive pediatric patients during the period following the COVID-19 initial outbreak in the metro New York City region. This span included the April 2020 peak of the pandemic, during which there were almost 800 deaths per day in the New York City area.
At the early stages of the pandemic in the metro NYC area, testing was strictly limited to high-risk individuals as per city and state department of health guidelines. As testing access improved in late April and early May, guidelines were slowly relaxed, which allowed for testing in all patients who sought a test, whether they were symptomatic or not. There were no out-of-pocket charges to the patient (including all uninsured patients) for testing during this time frame. All patients who tested positive were advised to follow the CDC guidelines of 14 days of quarantine from the last known exposure to a COVID source, or 10 days of isolation and 24 hours fever free, if symptomatic.
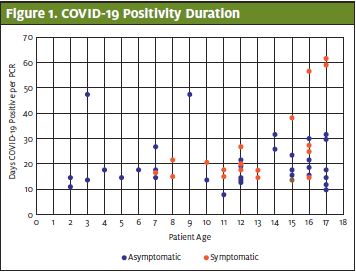
In the repeat positive population, 71% (45 out of 63 individuals) were asymptomatic at their initial presentation. Our previous research over the 3-month period of March 5 through June 22, 2020 showed that 48% of all pediatric patients who tested positive at that time were asymptomatic. We surmise that the higher asymptomatic rate could be due to length of time since initial exposure, as the peak wave in New York ended in April 2020. Eighteen of the 63 individuals who initially presented with symptoms consistent with COVID-19 had a significantly longer mean duration of 27 days of positivity compared with the mean of 20 days overall. (Figure 2.)
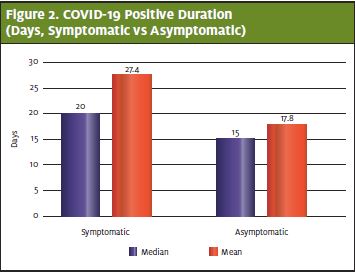
This difference may be due to an overall higher viral load at the beginning of the illness which is consistent with what other researchers have found.5 This cohort also skewed slightly older, with a mean of 13 years of age compared with the overall population with a mean of 12.0 years. Also, of note is that the patient who had the longest period of positivity (61 days) was 17 years old at time of testing, and therefore at the upper age in the pediatric cohort. Females had a slightly longer mean time of positivity at 17 days when compared to male mean positivity of 15 days. (Figure 3.)
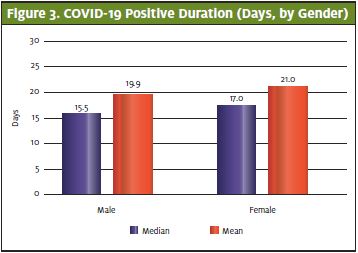
We posit that testing for cure is an unreliable method to ascertain whether children should return to school. Children are generally known to have a milder course of symptoms when compared to adults.6 Current CDC guidelines are that patients are considered fit to return to work after 10 days from the time of an initial positive test if they are asymptomatic, as there are no data to show replication of competent virus after a 10-day period.7 Yet unknown is how long coronavirus remains viable and, therefore, transmissible after the onset of symptoms in the pediatric population.
As a matter of practical concern, it is inadvisable to potentially hold children away from school for months awaiting a negative test. As the symptomatic appear to remain positive for a longer period, it will be important to determine whether this subgroup needs a longer period of isolation compared to the asymptomatic to help mitigate transmission in the community. These data appear to further support current CDC guidelines that testing for cure is an unreliable method.
Acknowledgements
There are no financial disclosures or conflicts of interest in relation to this study by any of the authors. The authors had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Singh S, Roy D, Sinha K, et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293:113429. Epub ahead of print. August 24, 2020.
- Gassman-Pines A, Ananat EO, Fitz-Henley J 2nd. COVID-19 and parent-child psychological well-being. Pediatrics. 2020;146(4):e2020007294.
- Kam KQ, Yung CF, Cui L, et al. A well infant with coronavirus disease 2019 with high viral load. Clin Infect Dis. 2020;71(15):847-849.
- Miao K, Illuzzi F, Hwang AC. High prevalence of asymptomatic COVID-19 in the pediatric population. J Urgent Care Med. 2020;15(1):21-23.
- Yonker LM, Neilan AM, Bartsch Y, et al. Pediatric severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): clinical presentation, infectivity, and immune responses. J Pediatr. 2020;227:45-52.e5.
- Ludvigsson JF. Systemic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088-1095.
- Centers for Disease Control and Prevention. Duration of isolation & precautions for adults. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Accessed December 22, 2020.
Author affiliations: Katharine Miao, MD, FACEP, SummitCityMD. Frank Illuzzi, MD, FACEP, CPE, SummitCityMD. Alexander C. Hwang, SummitCityMD.


