Published on
Urgent message: As understanding of COVID-19 in the pediatric age group evolves, it has come to light that children may contract the virus, yet be asymptomatic, more commonly than we initially believed. We have found a high prevalence of asymptomatic pediatric patients testing positive for COVID-19 in our urgent care clinics in the NY metro region.
Katharine Miao MD, Frank Illuzzi MD, and Alexander C. Hwang
IMPORTANCE
SARS-CoV-2 is the novel virus that causes COVID-19. After first being identified in China in December 2019, this disease has erupted into a global pandemic. In an effort to slow down the progression of the disease, many countries have either closed schools or moved toward remote learning.
According to data gathered from Johns Hopkins University and the World Health Organization, the United States bears the burden of nearly 25% of the worldwide infections while local governments, school districts, educators, and parents are attempting to make decisions regarding education in the fall of 2020.
As social distancing will undoubtedly be difficult to achieve in a traditional school setting, many are considering the idea of universal masking to prevent spread of the virus. Some believe that only schoolteachers, staff and older children need to wear masks, as younger children are less likely to contract or transmit this virus. We suggest that a greater understanding of the prevalence of asymptomatic carriers of COVID-19 in children up to age 17 would be helpful to parents, school administrators, and public health officials to make better informed decisions regarding the coming school year.
OBJECTIVE
To determine the rate of asymptomatic carrier status in the pediatric population presenting to a large chain of urgent care clinics during the early weeks of the outbreak in the metro New York City area in Spring 2020.
DATA SOURCE
Testing data from CityMD, which operates 125 locations in the metro New York City area.
STUDY SELECTION
This was a retrospective observational study using anonymized chart review of a pediatric population.
METHODS
CityMD obtained 367,912 COVID-19 PCR test results from March 9, 2020 to June 22, 2020. Of those tested, 12,286 were between the 0 and 17 years of age. All patients were accompanied by a guardian who requested a COVID-19 test at the time of visit. Patients were examined by a clinician wearing an N95 and appropriate personal protective equipment (PPE). Tests were obtained from nasopharyngeal swab specimens, transported in VCM (UTM) medium (green-top) tube, for SARS-CoV-2 RNA (COVID-19), Qualitative NAAT testing. All specimens were submitted to commercial laboratories for processing.
Of the 12,286 tests run in this age cohort, 711 were positive. The positive PCR results were then sorted by age by the in-house data analytics team and stratified by ICD code. Anonymized charts were then validated to assess for any reports of symptoms which would suggest Covid-19-related illness. As this was a retrospective analysis on anonymized data, an IRB waiver was obtained from Solutions IRB.
MAIN OUTCOME AND MEASURES
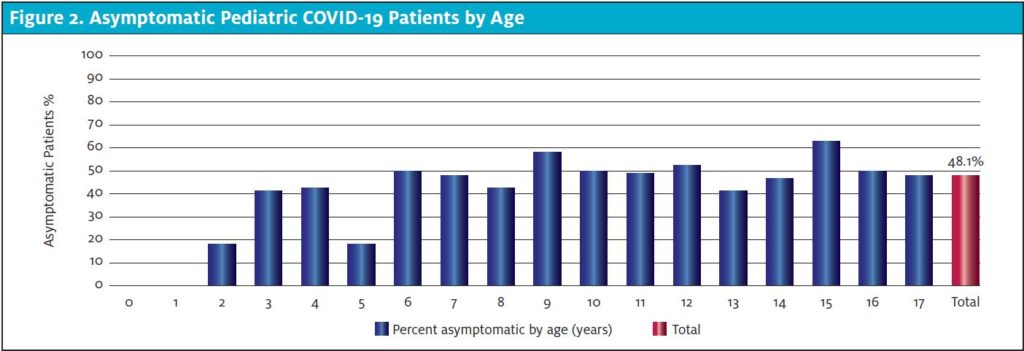
The primary finding revealed that 48.1% of the pediatric patients testing positive for COVID-19 at CityMD clinics during the study period were completely asymptomatic.
RESULTS
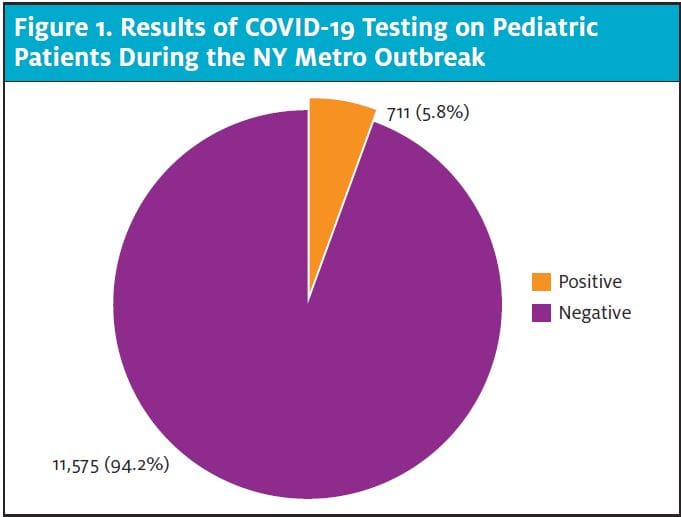
Out of 12,286 patients, there were 711 patients who tested positive for COVID-19. The pediatric positivity rate was 5.8%, compared with a 10.2% positivity rate for the overall population tested at CityMD clinics during the same study period. Among the pediatric patients who were COVID-19 positive, the proportion of asymptomatic carriers was 48.1%, ranging from a low of 0% in the 0-1 age cohort to a high of 63.8% in the 15-year-old age group.
CONCLUSION AND RELEVANCE
This study was a retrospective analysis and chart review on a cohort of PCR-positive pediatric patients during the peak and the period immediately following the COVID-19 initial outbreak in the metro New York City region. Schools in the New York City suburbs began shutting down on March 8, and the New York City schools closed a week later. Thus, the examined testing period was almost completely during a period of school closure.
Testing for COVID-19 via PCR was initially very limited, due to supply shortages and strict criteria limiting the number of tests performed at the beginning of the outbreak. This circumstance led naturally to a selection bias of those who were ill enough to seek and warrant testing. As commercial testing became more available in late April and May 2020, more people were able to obtain tests, and the positivity rate decreased correspondingly. Financial barriers to testing were minimized as there were no copays or deductibles charged to anyone seeking testing, and uninsured patients were tested at no cost to them. Relatively few infants were tested, possibly due to the hesitancy of parents to bring infants to a doctor’s office during a pandemic, and/or parents utilizing other options for the care of their infants.
Our findings indicate that the pediatric patients had a lower positivity rate (5.8%) than the overall population (10.2%; see Figure 1)
There have been extensive discussions in the scientific community as to whether age-related factors may render children less susceptible to SARS-CoV-2 than adults.1 However, the lower positivity rate may be due in part to school closures and stricter social distancing for children. We believe there is an urgent need to study further transmissibility of subclinical infections among children.
The proportion of asymptomatic patients was generally consistent across all pediatric age groups. For instance, the 3- and 4-year old age groups had an asymptomatic rate of 41.7% and 43.8%, respectively, which closely mirrors the overall asymptomatic rate of 48.1%. (Figure 2). Very young children (0-2 age cohort) exhibited a much lower asymptomatic rate, ranging from 0 to 16.7%, but we believe this may be due to selection bias, as parents may be more likely to bring in a sick infant than a well infant for testing.
The most common symptoms and diagnosis of cough, fever, and viral illness were consistent through all age groups (Figure 3). There is a possibility of recall bias in which parents and children under-report symptoms and/or symptoms are not recorded. Of note, some of the symptoms reported in positive patients were as mild as nasal congestion and are unlikely to warrant much concern in the absence of COVID-19. Loss of smell and loss of taste were also more commonly exhibited among teenagers, and we suspect young children may not be able to articulate such symptoms. This suggests that parents may face practical challenges in determining if their young child is exhibiting symptoms of SARS-CoV-2 before heading to school.
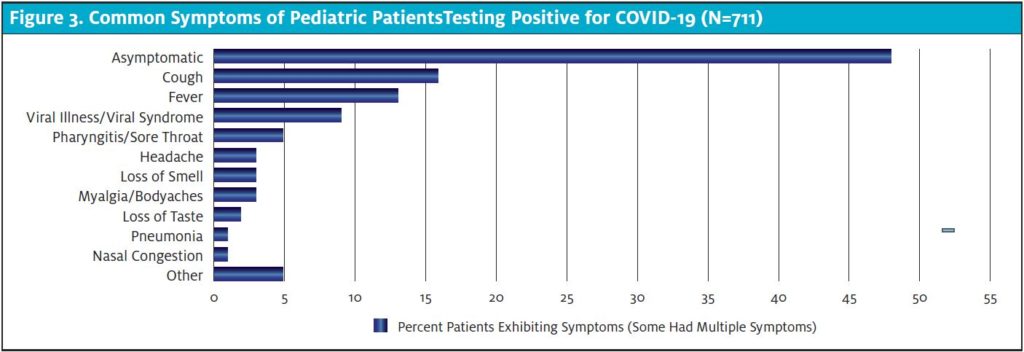
The CDC has noted there is evidence to support transmission in asymptomatic and presymptomatic people.2,3 Given that our data support that 48.1% of children who contract SARS-CoV-2 are asymptomatic, and transmission rates among children as well as from children to adults are currently unclear, it appears that mitigation strategies targeted at identifying and isolating patients based on symptoms (temperature screening, questionnaires, etc.) may be insufficient to curtail outbreaks. Parents and educators cannot rely solely on exhibition of clinical symptoms (fever, cough, etc.) to determine if children are COVID-free before allowing them to participate in in-person learning at school. More comprehensive strategies such as universal masking, strict social distancing, and batch testing may need to be implemented in order to maintain a safer in-school experience for children and staff.
Citation: Miao K, Illuzzi F, Hwang AC. High prevalence of asymptomatic COVID-19 in the pediatric population. J Urgent Care Med. October 2020. Available at: https://www.jucm.com/high-prevalence-of-asymptomatic-covid-19-in-the-pediatric-population/
References
1. Davies NG, Klepac P, Liu Y, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26(8):1205-1211.
2. Furukawa NW, Brooks JT, Sobel J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg Infect Dis. 2020;26(7):e201595.
3. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970.
Author affiliations: Katharine Miao, MD, SummitCityMD; Frank Illuzzi MD, Summit CityMD; Alexander C. Hwang, SummitCityMD. The authors have no relevant financial relationships with any commercial interests.
