Urgent message: Ultrasound can provide essential data in the urgent care evaluation of suspicion of acute appendicitis. Facilitating a rapid diagnosis allows for immediate and appropriate decisions regarding management.
Andrew Alaya, MD, MSc
INTRODUCTION
Appendicitis is thought to be the result of luminal obstruction due to various etiologies (such as lymph node hyperplasia, coprolites, or parasites) which lead to increased mucus production and bacterial overgrowth. This results in wall tension and eventually necrosis and potentially perforation.1
Appendicitis is one of the most common causes of acute abdominal pain requiring urgent surgical intervention. For this reason, caution should be exercised in patients in whom appendicitis is suspected; in short, it should not be missed. Appendicitis effects males more than females (lifetime risk of 8.6% vs 6.7%, respectively).2
Though common, appendicitis still presents as a diagnostic challenge—especially in females of childbearing age, due to similarities in the clinical representation of appendicitis and gynecological abnormalities. In pregnancy, it is the most common nonobstetric surgical emergency, with an incidence of 6.3 per 10,000 pregnancies during the antepartum period that increases to 9.9 per 10,000 postpartum.3
In the United States, more than 300,000 appendectomies are performed each year. Due to the extensive use of CT scan, in less than 10% of these appendectomies does the removed appendix turn out to be normal.4 In Europe, on the other hand, diagnosis is often made clinically, resulting in higher laparoscopy rate and higher negative appendectomies (up to 32%).5
If untreated, appendicitis can result in perforation. The perforation rate of appendicitis is 16%-40% overall, with higher occurrence among young patients (40%-57%) and patients 50 years of age and older (between 55% and 70%). The mortality rate of perforated appendicitis is around 5%.6 Acute pelvic pain, defined by the sudden onset of abdominal pain with particular intensity, is related to a wide variety of diseases.
The presence of vague or altered clinical signs can make it difficult to diagnose acute appendicitis. This can be due to the large variations in the location of the appendix. Diagnosis is more complicated in pregnant women due to concurrent maternal physiologic and anatomic changes.7
The clinical diagnosis of appendicitis is based on the classic anamnesis such as: McBurney’s, Blumberg’s, Rovsing’s, obturator, and psoas signs during the physical examination, together with fever and elevated inflammation values from laboratory tests.
Clinical signs and symptoms are more helpful in confirming the diagnosis rather than ruling it out when absent. The clinical diagnosis of appendicitis is not always easy and can be challenging, involving a combination of clinical, laboratory, and radiological findings. The use of laboratory investigations such as total leukocyte count, differential leukocyte account, C-reactive protein, and others are thought to be sensitive but lack sufficient specificity.8 Ultrasound is thought to be a useful modality after the introduction of graded compression by Puylaert9 in diagnosis of appendicitis. Ultrasound is operator-dependent and in the right hands is considered to have the same accuracy as CT scan for the diagnosis of acute appendicitis.10
HISTORY AND PHYSICAL EXAMINATION
One of the most important functions of urgent care diagnosis is an accurate patient history. A patient must always be asked about the time of onset of symptoms, site of pain, medical history, and current medications. Physical examination for the known signs of appendicitis such as a positive McBurney’s sign, psoas sign, obturator sign, and Rovsing sign are essential.
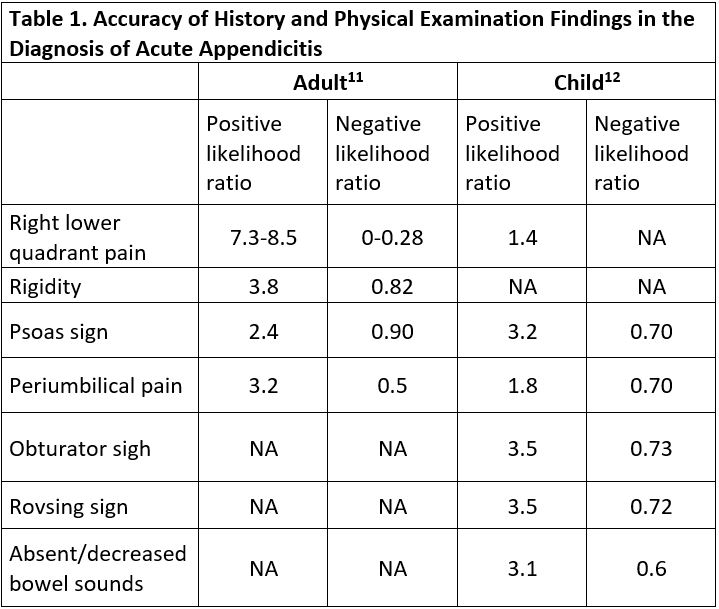
The signs and symptoms that best rule in acute appendicitis in adults are right lower quadrant pain, abdominal rigidity, and radiation of periumbilical pain to the right lower quadrant with positive likelihood ratio of 7.3-8.5, 3.8, and 3.2 respectively.11 In children however, absent or decreased bowel sounds, a positive psoas sign, a positive obturator sign and positive Rovsing sign are the most reliable for ruling in acute appendicitis with positive likelihood ratio of 3.1, 3.2, 3.5 and 3.5, respectively.12Table 1 presents the likelihood ratios of various signs and symptoms in adults and children.
When a patient complains of a change in the location of pain from the upper abdomen to the right lower abdominal quadrant, this is most often associated with acute appendicitis. This is due to a “shift” of periumbilical or epigastric pain (visceral) to the right lower quadrant (somatic) pain when the parietal peritoneum becomes involved with the inflammatory process.13
Care must be taken when it comes to children and adolescents. History and physical examination must be taken according to the patient’s age and developmental stage. Experience in clinical diagnosis is very important, especially when it comes to small children. Absence of nausea and vomiting, abdominal tenderness and leukocytosis rules out appendicitis with 98% accuracy.14
The location of the appendix is very important. In pregnant women the appendix may be displaced cranially due to the enlarged uterus resulting in pain felt in the upper abdomen rather than in the right lower quadrant. Symptoms of nausea, vomiting, and abdominal pain can be difficult to distinguish from pregnancy-related symptoms.3
Moreover, depending on the location of the inflammatory process such as along the psoas muscle, pain may be perceived in the lower back, thigh, or knee and not on the right anterior abdominal wall. This makes diagnosis of acute appendicitis in pregnant women challenging. Delay in the diagnosis of acute appendicitis may lead to increased mortality and morbidity rates for both mother and fetus. It is very important to diagnose acute appendicitis as early as possible; at the same time, care must be taken to avoid negative appendectomy due to misdiagnosis.
Laboratory Tests
There are no specific laboratory parameters specific to diagnosing acute appendicitis. Individually, white blood cell (WBC) count, leukocytosis/neutrophilia, and an elevated serum concentration of C-reactive protein (CRP) are considered and widely used for this purpose; however, they are nonspecific signs of inflammation.15
These parameters are also high in healthy pregnant women.14 Nevertheless, it has been shown that WBC count value of higher than 18×109/L is one of the most important parameters for the diagnosis of acute appendicitis in pregnant women.16 Laboratory tests are helpful when combined with clinical signs and symptoms and clinical decision rules or in combination with imaging studies as part of a structured evaluation of the patient and patient management.15 Body temperature should be measured, and urinalysis should be performed. At the same time, a pregnancy test should be done in females of childbearing age.10 These tests serve to rule out several differential diagnoses of right lower quadrant pain such as urolithiasis, urinary tract infection, and ectopic pregnancy. In females with unclear clinical presentation, gynecological consultation should be considered. A digital rectal examination is of low diagnostic benefit and needs not be performed.17
Scoring Systems
Many scoring systems have been developed so that an investigation can be done objectively and independent of the clinical experience of the examiner in suspected diagnosis of acute appendicitis. The most commonly used scoring systems are the Alvarado score (1986) and the Appendicitis Inflammatory Response (AIR) score (2008).18 Many countries do not generally use scoring systems like these as part of routine clinical practice to aid in the diagnosis. The Alvarado score system has a 99% sensitivity but is only 43% specific. This is because of the setting of the threshold. If the threshold is increased from 5 to 7, the specificity increases to 81% at the cost of a lower sensitivity, down to 82%. That is why the Alvarado score system is most useful for ruling out appendicitis, rather than diagnosing it. The AIR score has a sensitivity of 92% and a specificity 63%18.
The use of a scoring system alone for the diagnosis of acute appendicitis is not recommended by the World Society of Emergency Surgery (WSES),19 which prefers a stepwise diagnostic approach pathway depending on age, sex, and clinical signs and symptoms of the patient.
Imaging
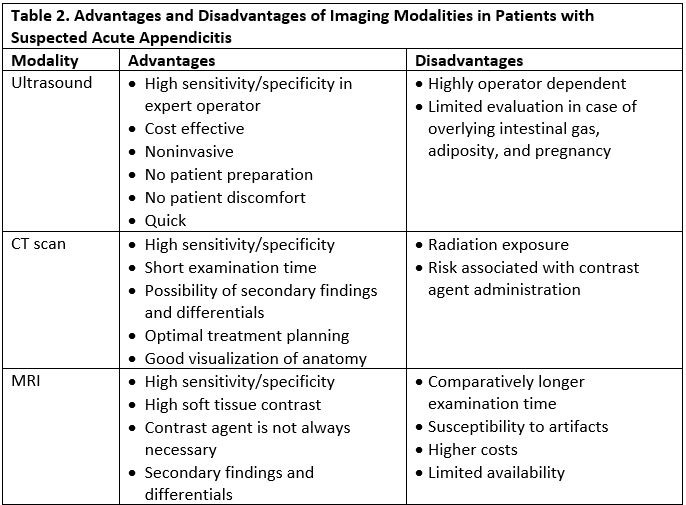
Ultrasound, CT, and MRI are the imaging modalities used to evaluate a patient with suspected appendicitis; each has its relative merits and drawbacks (see Table 2).
Since the beginning of the millennium, in the United States CT scanning has been considered as the gold standard for diagnosing appendicitis.19 Many organizations such as the National Cancer Institute, the American Academy of Pediatrics , and the American College of Radiology recommend ultrasound as the initial imaging modality, especially in children and pregnant women.20 However, ultrasound is operator-dependent, and its diagnostic accuracy depends on the skills and experience of the operator. This places ultrasound at a disadvantage compared with other modes of imaging. A negative ultrasound finding may not suffice to rule out appendicitis.21 Moreover, obesity is a problem for ultrasound. Patients who are overweight (BMI >30 kg/m2) are more likely to undergo a CT scan (see Figure 1), as ultrasound will not be helpful for such patients.21 This is due to the fact that ultrasound waves cannot attenuate the fat layer, not reaching and visualizing the appendix for accurate diagnosis.

URGENT CARE DISPOSITION
In an urgent care setting, it is important to estimate the pre-image likelihood of appendicitis to facilitate the appropriate diagnostic workup and necessary referrals. Using scoring systems such as AIR and Alvarado scores, patients are categorized as low risk, intermediate risk, or high risk.
Patients categorized as low risk are discharged with appropriate safety netting, whereas high-risk patients are referred directly to the hospital as they are likely to require surgery. Intermediate-risk patient are those who can benefit from diagnostic imaging.22
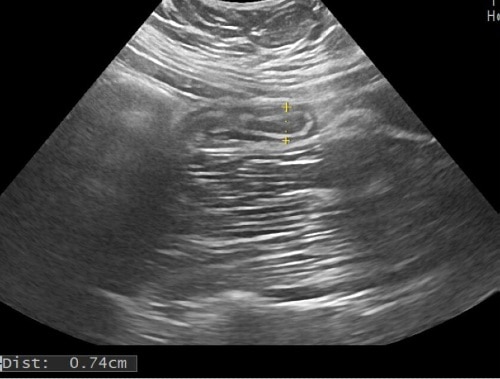
The overall sensitivity and specificity of ultrasound in the diagnosis of appendicitis are 76% and 95%, respectively.23 In one meta-analysis, the sensitivity and specificity of ultrasound in diagnosis of acute appendicitis were even higher, at 91% and 97%.24 According to WSES,20 ultrasound in combination with clinical parameters may improve the diagnostic sensitivity and specificity and reduce the need for CT scanning in adult patients with suspected acute appendicitis (see Figure 2). In the case of pediatric and young adult patients, ultrasound is the initial imaging study of choice for the diagnosis of acute appendicitis.

MRI may play a role in avoiding radiation dose from CT scanning in children and pregnant women with inconclusive ultrasound findings. A prospective study performed by Kinner, et al25 compared MRI and CT scanning, and showed similar diagnostic accuracy of acute appendicitis—85.9% sensitivity and 93.8% specificity for unenhanced MRI, 93.6% and 94.3% for contrast-enhanced MRI, and 93.6% and 94.3% for CT scanning, respectively. The cost and availability of MRI often prevents its use as the initial imaging investigation in the cases of suspected acute appendicitis.
In females, a transvaginal examination can be done to rule out diseases of the female genitalia such as ovarian torsion,26 symptomatic ovarian cysts, or an ectopic pregnancy27 and diagnosing appendicitis if a transabdominal ultrasound did not yield a definitive diagnosis. Acute appendicitis is the most common cause of an acute abdomen during pregnancy.3 Ultrasound is the modality of choice when it comes to pregnancy. In the first and second trimester of pregnancy ultrasound has a good diagnostic yield (see Figure 3); however, in the third trimester, ultrasound is limited due to the changes of the anatomy in pregnant women at this stage of pregnancy.3 This is due to the enlargement of the uterus displacing the appendix from the lower right quadrant to the upper right quadrant over the course of the pregnancy.
Treatment
In the diagnosis and treatment of acute appendicitis, there is increasing discussion of the possibility of nonsurgical treatment, of the optimal timing of surgery, and of the appropriate postoperative care.28
According to the WSES, the Society of American Gastrointestinal Endoscopic Surgeons (SAGES), and the European Association for Endoscopic Surgery (EAES), appendectomy is the treatment of choice for uncomplicated acute appendicitis in all age groups.28 Recently, many publications have documented the successful conservative treatment of uncomplicated appendicitis with antibiotics in children and adults. This approach was first proposed by Harrison in 1953, but is attracting increased attention.28 Current evidence is insufficient to enable the detection of any advantage for conservative treatment and surgery remains the treatment of choice for acute uncomplicated appendicitis. Moreover, surgery should not be delayed by more than 12 hours in children and adolescents, patients over age 65, or patients with comorbidities.29
There is no standard evidence-based approach to the treatment of complicated acute appendicitis. In principle, it can either be treated with urgent surgery or managed conservatively (ie, with antibiotics alone or with the interventional placement of drain). The morbidity and efficacy of conservative management are still debatable, however, and further studies are needed to determine the best way to treat complicated appendicitis in consideration of the patient’s risk factors and clinical condition.30
COMPLICATIONS
The main concerning complication of acute appendicitis is perforation as this may lead to abscesses, peritonitis, bowel obstruction, sepsis, and even fertility problems in females. The rate of perforation in adults ranges from 17% to 32%.31 Perforation may lead to the extended use of antibiotics and more severe postoperative complications. The risk factors for perforation include age over 65, immune suppression or acquired immune deficit, and pregnancy. Perforation risk is directly associated with the time from onset of diagnosis and surgery.32 Demonstration of an appendicolith on an ultrasound is highly associated with perforation if not treated with early appendectomy.28 In the risk factor group of patients with high leukocyte counts, CRP values are correlated with the risk of gangrenous appendicitis. In pregnant women, appendectomy can be carried out safely in all three trimesters. Miscarriage is more common in complicated appendicitis (20%) than in uncomplicated appendicitis (1.5%).33
CONCLUSION
Appendicitis can present itself as acute or complicated acute. Diagnosis is based on imaging findings and clinical presentation. Ultrasound is the first choice for the diagnosis of appendicitis but has the disadvantage of being dependent on the skills and experience of the operator. When ultrasound is not conclusive, such as in patients having a high BMI, CT scan may be considered. In pregnant women, MRI should be performed if available. Treatment is currently based on surgical intervention, although future research looks to focus on conservative measures. To date, antibiotic treatment has demonstrated efficacy in the short term but recurrence is likely in the long term. Laparoscopy has surgical advances as it enables patients same-day discharge, fewer complications, shorter recovery times, and low cost.
REFERENCES
- Cervellin G, Mora R, Ticinesi A, et al. Epidemiology and outcomes of acute abdominal pain in a large urban emergency department: retrospective analysis of 5,340 cases. Ann Transl Med. 2016;4(19):362.
- Jaschinski T, Mosch C, Eikermann M, Neugebauer EA. Laparoscopic versus open appendectomy in patients with suspected appendicitis: a systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015;15:48.
- Zingone F, Sultan AA, Humes DJ, West J. Risk of acute appendicitis in and around pregnancy: a population-based cohort study from England. Ann Surg. 2015;261(2):332-337.
- Cuschieri J, Florence M, Flum DR, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 2008;248(4):557-563.
- Lim J, Pang Q, Alexander R: One year negative appendicectomy rates at a district general hospital: A Retrospective Cohort Study. Int J Surg 2016; 31: 1-4.
- Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886-892.
- Masselli G, Derchi L, McHugo J, et al. Acute abdominal and pelvic pain in pregnancy: ESUR recommendations. Eur Radiol. 2013;23(12):3485-3500.
- Shogilev DJ, Duus N, Odom SR, Shapiro NI. Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014. West J Emerg Med. 2014;15(7):859-71.
- Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158(2):355-60.
- Sartelli M, Baiocchi GL, Di Saverio S, et al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J Emerg Surg. 2018;13:19.
- Wagner JM, McKinney WP, Carpenter JL. Does this patient have appendicitis? JAMA. 1996;276(19): 1589-1594.
- Benabbas R, Hanna M, Shah J, Sinert R. Diagnostic accuracy of history, physical examination, laboratory tests, and point-of-care ultrasound for pediatric acute appendicitis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med. 2017;24(5):523-551.
- Kharbanda AB, Dudley NC, Bajaj L, et al. Validation and refinement of a prediction rule to identify children at low risk for acute appendicitis. Arch Pediatr Adolesc Med. 2012;166(8):738-744.
- Anandalwar SP, Callahan MJ, Bachur RG, et al. Use of white blood cell count and polymorphonuclear leukocyte differential to improve the predictive value of ultrasound for suspected appendicitis in children. J Am Coll Surg. 2015;220(6):1010-1017.
- Yu CW, Juan LI, Wu MH, et al. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br J Surg. 2013;100(3):322-329.
- Theilen LH, Mellnick VM, Shanks AL, et al. Acute appendicitis in pregnancy: predictive clinical factors and pregnancy outcomes. Am J Perinatol. 2017;34:523–528.
- Takada T, Nishiwaki H, Yamamoto Y, et al. The role of digital rectal examination for diagnosis of acute appendicitis: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0136996.
- Scott AJ, Mason SE, Arunakirinathan M, et al. Risk stratification by the Appendicitis Inflammatory Response score to guide decision-making in patients with suspected appendicitis. Br J Surg. 2015;102(5):563-572.
- Holscher HC, Heij HA. Imaging of acute appendicitis in children: EU versus U.S. … or US versus CT? A European perspective. Pediatr Radiol. 2009;39(5):497-499.
- Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27.
- Reich B, Zalut T, Weiner SG. An international evaluation of ultrasound vs. computed tomography in the diagnosis of appendicitis. Int J Emerg Med. 2011;4:68.
- Chang ST, Jeffrey RB, Olcott EW. Three-step sequential positioning algorithm during sonographic evaluation for appendicitis increases appendiceal visualization rate and reduces CT use. AJR Am J Roentgenol. 2014;203(5):1006-1012.
- Smith MP, Katz DS, Lalani T, et al. ACR Appropriateness Criteria right lower quadrant pain–suspected appendicitis. Ultrasound Q. 2015;31(2):85-91.
- Matthew Fields J, Davis J, Alsup C, et al. Accuracy of point-of-care ultrasonography for diagnosing acute appendicitis: a systematic review and meta-analysis. Acad Emerg Med. 2017;24(9):1124-1136.
- Kinner S, Pickhardt PJ, Riedesel EL, et al. Diagnostic accuracy of MRI versus CT for the evaluation of acute appendicitis in children and young adults. AJR Am J Roentgenol. 2017;209(4):911-919.
Read Similar Articles
- Atypical Appendicitis In The Older Patient
- Appendicitis Due To Squirrel Dinner
- How Useful Is Ultrasound In Diagnosing Ovarian Torsion?

