Urgent message: Falls in the elderly may be mechanical or due to an underlying etiology, making the urgent care evaluation tricky. The provider will need to evaluate the sequelae of the fall as well as searching for the hidden cause.
Introduction
Medical complaints from the elderly population will pose more of a challenge when the chief complaint is fall. The source can range from a neurologic etiology, a cardiac abnormality, or a metabolic or endocrine source.
Presentation
BS, an 83-year-old woman, presented with her daughter reporting a 2-week history of falls. She admits to intermittent fatigue, dizziness, and loss of balance, but denies syncope. The daughter reports the last episode occurred at home 3 days ago.
BS denied any numbness or focal weakness, headache, loss of vision, loss of hearing, chest pain, difficulty breathing, nausea, vomiting, diarrhea, fever, cough, abdominal pain, or urinary symptoms.
- PMH: HTN, DM type 2, hypercholesterolemia
- Medications included vitamin D, glipizide, metformin, simvastatin, telmisartan
- Allergies included sulfa
- Social history: No tobacco, alcohol or drug use
- Physical examination:
- Vital signs: BP 157/78, HR 74, temp 97.7, O2 sat 97%, resp 12
- General: A&O, NAD
- HEENT: NC/AT. PERRL. Neck with painless ROM
- CVS: Heart sounds normal. No murmurs
- Resp: mildly decreased breath sounds in the right lung base posteriorly
- Abdomen: no visible injury. Nontender. Bowel sounds normal. No masses
- Skin: Skin intact
- Extremities: Normal inspection. Extremities atraumatic. Normal gait
- Neuro: Oriented x3. No motor or sensory deficit.
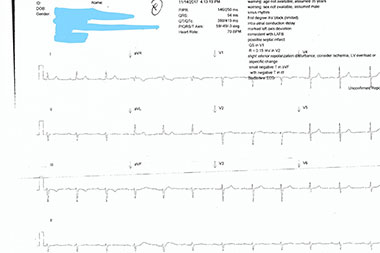
Figure 1
The following tests were performed:
- ECG: Normal sinus rhythm. Normal P waves. Normal PRI. Normal QRS complex. Normal axis. Normal QT. T wave inversion in lead III. Prior ECG unavailable for review. (See Figure 1).
- Bedside tests: Urine dipstick: trace leukocytes; nitrite negative; protein negative; glucose normal; ketones negative; urobilinogen normal; bilirubin negative; trace blood.
- Chest X-ray, PA and lateral: Infiltrate present along the retrocardiac view consistent with pneumonia. (See Figures 2a and 2b).


Figure 2a & 2b
Course and Treatment
The ECG showed T wave inversion only without reciprocal changes; without a prior ECG on file, it was unclear if this was consistent with chronic ECG changes. Due to the lobar appearance of the infiltrate found on chest x-ray, BS was transferred by private vehicle with her daughter to a local emergency room for further evaluation and diagnostic testing.
Discussion
A fall is defined as a person having an accident where he/she comes into contact with the ground or another lower level.1 A person can strike another object prior to making ultimate contact with the ground, leading to two potential sources of harm; the provider needs to evaluate the patient for injury from the fall, as well as the etiology of the fall.
As the United States population continues to age, medical facilities will evaluate patients in greater numbers over the age of 65. Falls are the leading cause of injury-related visits to emergency departments in the United States2 and the primary etiology of accidental deaths in persons over the age of 65 years.3 It is reported that in 2014, 28.7% of older adults reported falling.4 Elderly patients, in particular, need a thorough evaluation as related causes of falls broaden when considering both extrinsic and intrinsic factors.
Extrinsic factors include environmental factors such as walking on a surface needing greater postural control and mobility.1 This also includes when an environment is unfamiliar (ie, a new neighborhood).
Intrinsic factors signify a decline in mobility because of one’s age, muscle tone, and balance. Age-related changes can alter methods involved in maintaining balance and stability while walking, standing, or sitting, and can increase the risk of falls. The elderly can also face impairments with visual acuity and depth perception.1 Contrast sensitivity and the ability to adapt to darker surroundings decline as one ages. Changes in muscle activation patterns and the inability to produce sufficient muscle power may hinder the elderly’s ability to maintain or recover balance in response to uneven surfaces or an object in their footpath.
As urgent care clinicians, our duty is to maintain a high level of suspicion as to why the patient fell, as a fall is often a symptom of serious underlying pathology (eg, infection, electrolyte imbalance, stroke, or cardiac etiology, even when the patient reports a history of a mechanical fall).5 In the urgent care setting, many of us may be limited in our resources for a full diagnostic evaluation in such a patient. Making the diagnosis even more challenging, elderly patients may present later in the course of their acute illness than younger patients.
Table 1 highlights data from a retrospective review completed by Massachusetts General Hospital in Boston, drawn from electronic health records of 161 patients admitted from January 1, 2000 to December 31, 2014. Patients presented with a chief complaint revolving around a fall, were hospitalized, and found to have a coexisting systemic infection (CSI) which may have served as a possible contributing factor.6
Of the patients presenting with a fall and CSI during the study period, 85 (52.8%) were female, with a mean age of 76 years (range 35-102).
The researchers noted that CSI in patients presenting with a chief complaint revolving around a fall is commonly associated with bacteremia, is often not clinically suspected, and is associated with a significant in-hospital mortality.6
Table 1: Coexisting Systemic Infections Found from Retrospective Review
| Infection | No. (%) of patients |
| Urinary tract infections | 71 (44) |
| Bacteremia | 64 (39.7) |
| Lower respiratory tract infections (ie, pneumonia) | 37 (22.9) |
| Sepsis of an unclear source | 34 (21.1) |
Findings in other literature support that elderly present to healthcare institutions later in their illness. This factor, along with a low index of suspicion from the clinician and the lack of classic clinical symptoms of infection, lead to delayed recognition of severe illness in the elderly.74
Summary
Our patient’s presentation could have resulted in nothing more than an evaluation for possible injuries from the fall, but a good history and exam were able to localize an infiltrate which was likely the underlying cause of the fall. UTI, as well as infection in the upper and lower respiratory tracts, can be readily diagnosed, leading to at least one source for the infection that can lead to quicker treatment and recovery. This case highlights the importance of our ability as urgent care clinicians to use the resources available to assist in the care of the elderly presenting to us with a chief complaint of a fall.
Take-Home Pearls
- Falls may be a nonspecific presenting sign of an acute illness in patients over 65 years old.
- If the presentation is suggestive of an infection, consider obtaining a urinalysis and/or chest x-ray to rule out infectious sources of falls.
- More than one etiology is often the cause of a fall in the elderly.
- Assess the sequelae of the fall (fracture, strain, contusion), as well as the etiology of the fall (vertigo, imbalance, infection)
Citation: Kelly K. Infection masquerading as a fall in the elderly. J Urgent Care Med. March 2019. Available at: https://www.jucm.com/infection-masquerading-as-a-fall-in-the-elderly/.
References
- Rubenstein LZ. Falls in the elderly. Merck Manual Professional Edition. Merck & Co., Inc. Kenilworth, NJ.
- National Hospital Discharge Survey. Vital Health Stat. 1998;13:1-76.
- Xu J, Murphy SL, Kochanek KD, et al. Deaths: final data for 2016. Natl Vital Stat Rep. 2018;67(5):1-76.
- Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged >65 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993-998.
- Blickendorf R. Urgent care management of geriatric fall. J Urgent Care Med. Available at: https://www.jucm.com/urgent-care-management-of-geriatric-falls/. Accessed February 10, 2019.
- Durkin M. A new cause to consider in falls: Infections. ACP Hospitalist. 2016 May.
- Brito V, Niederman MS. Predicting morality in the elderly with community-acquired pneumonia: should we design a new car of set a new ‘speed limit’? 2010;65(11):944-945.
Kamilah Kelly, MD, MS is an emergency medicine physician in Elkridge, MD. The author has no relevant financial relationships with any commercial interests.

