Urgent message: Make the distinction between viral and bacterial conjunctivitis to ensure children receive appropriate treatment and to avoid the negative consequences of antibiotic overuse.
Julian P. Ponsetto MD, Momoko K. Ponsetto MD
Citation: Ponsetto JP, Ponsetto MK. Differentiating acute conjunctivitis presentations in children. J Urgent Care Med. 2023;17(11):15-20.
Infectious conjunctivitis or “pink eye” is common in the pediatric population, accounting for 2.7% of diagnoses in pediatric urgent care.1 However, it can be difficult to distinguish viral from bacterial disease, and it’s important to not presume the cause is infectious. Additionally, some schools and daycares have mandates requiring children with pink eye to stay home or even receive antibiotic treatment prior to returning.
Difficulty in making a clinical distinction between viral and bacterial conjunctivitis and the desire to get children back to school leads many prescribers to write for topical antibiotics in most, if not all, cases of infectious conjunctivitis. However, antibiotic use is ineffective against viral conjunctivitis, and the extent of its benefit in most forms of bacterial conjunctivitis appears marginal. Overuse of antibiotics leads to bacterial resistance, unnecessary expense, and added stress in attempts at administration for young children and their caregivers.
This article reviews the common pathogens that cause infectious conjunctivitis in children and adolescents and discusses the history and exam findings that help differentiate viral and bacterial etiologies, as well as other causes of eye redness.
Non-Infectious Etiologies Of Red Eye
While infectious conjunctivitis is the most common cause of eye redness in children, it is important to differentiate eye redness and/or eye discharge from the non-infectious causes. These include:
- Allergic conjunctivitis – Characterized by tearing, burning, itching, and conjunctival edema (chemosis) with conjunctival papillae on lid eversion. Allergic conjunctivitis is often associated with rhinitis but lacks fever and lymphadenopathy.
- Chemical eye injury – Characterized by redness, pain, and swelling after splashes of irritating or toxic chemicals. Depending on the chemical, concentration, and exposure, this can be vision-threatening. Especially in the case of extreme pH acidic or alkali exposure injuries, the exposure can be a medical emergency. An exposure history is usually suggestive for considering this diagnosis.
- Corneal abrasion and/or foreign body – Characterized by severe pain, redness, tearing, and photophobia after a traumatic injury or contact lens use. With more significant abrasions, patients may be resistant to eye opening. Globe rupture can occur. Pain is usually relieved with application of topical anesthetic.
- Nasolacrimal duct obstruction – Commonly presenting in the first year of life, this condition occurs when the nasolacrimal duct is incompletely formed/patent. Patients will present with excessive tearing (epiphora) without redness, which may worsen when suffering from an upper respiratory infection. If redness, purulent discharge, or swelling appear around the medial canthus, this is suggestive of concomitant dacryocystitis.
- Dry eyes – This condition is characterized by chronic eye irritation and occasional conjunctival infection. This can commonly occur postoperatively and in contact lens wearers. Rarely, dry eyes can be related to autoimmune disease, such as Sjogren’s syndrome.
- Uveitis – Also commonly referred to as “iritis,” uveitis is caused by inflammation along the uveal tract (iris, ciliary body, and choroid). Uveitis is characterized by eye pain, photophobia, and “ciliary flush” pattern of redness surrounding the iris predominantly. While this can occur from blunt ocular trauma, it’s most commonly idiopathic (60% of cases), and the remaining cases are often associated with autoimmune disorders (eg, Behçet’s disease or most commonly juvenile idiopathic arthritis).
Differentiating Between Bacterial and Viral Infectious Conjunctivitis
Presentation of infectious conjunctivitis is variable and nonspecific and can include discharge, conjunctival erythema, photophobia, itching, burning, tearing, and foreign body sensation. Severe pain, vision changes, and/or significant photophobia suggest a different and more concerning etiology. Classic clinical presentations of the various etiologies of conjunctivitis are rare, and patients tend to have overlapping constellations of signs and symptoms.
Since patients can have some or all of these symptoms in either bacterial or nonbacterial disease, it’s important to look closely at differentiating factors to make the most accurate diagnosis. Illustrating this point, a study of patients with culture-positive bacterial conjunctivitis found: 58% had itching; 37% had bilateral involvement; and 35% had serous or no discharge.[i]
Among all pediatric patients with conjunctivitis, a bacterial pathogen can be cultured about 50% of the time, although culture is not recommended as part of routine practice, as it would rarely change practice or affect outcomes.[ii] The variables most associated with having a negative bacterial culture were: 1) age 6 years and older; 2) no glued or matted eyes in the morning; 3) no discharge or watery discharge; and 4) presentation in April through November. Patients fulfilling all 4 of these criteria rarely had positive cultures, whereas presence of mucoid or purulent discharge and matted eyelids predicts a >95% risk of positive bacterial culture.[iii]
A practical approach for the urgent care provider to differentiate bacterial and viral conjunctivitis may include the following:
- Visual acuity or “the vital sign of the eye” – Age-appropriate assessment of visual acuity is crucial in any vision or eye complaint. Conjunctivitis does not cause changes in visual acuity. Altered vision should prompt consideration for other etiologies of redness in the eye.9
- Eye discharge – Bacterial conjunctivitis is more commonly associated with purulent eye discharge, especially if it persists throughout the day. While both bacterial and viral disease can cause the affected eye(s) to be “stuck shut” in the morning, the absence of discharge or the stuck-shut finding makes viral disease much more likely, especially when associated with other viral symptoms (eg, fever, cough, etc.).8
- Unilateral vs bilateral disease – While bacterial disease is more classically unilateral, both bacterial and viral disease can cause either unilateral or bilateral disease. Since the urgent care evaluation is a single point in time, it is difficult to extrapolate etiology from the disease laterality. Viral conjunctivitis frequently starts with redness of one eye, but the second eye often becomes involved in 24-48 hours.
- Patient age – Bacterial conjunctivitis is more common than viral etiologies in children, especially in infants, toddlers, and preschool age children. The younger the patient, the higher the likelihood of bacterial etiology.12
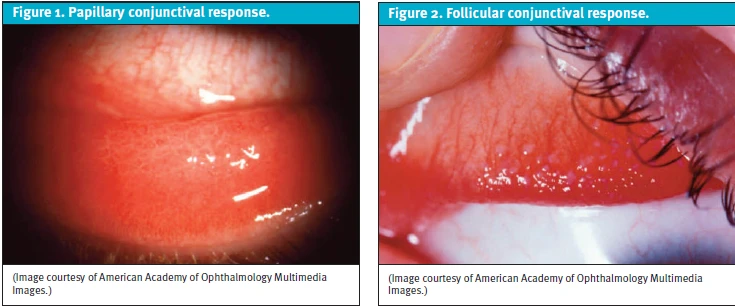
- Conjunctival exam – A papillary reaction in the conjunctiva can appear as flattened nodules, which are vessels surrounded by acute and chronic leukocytes (Figure 1). This is more common in allergic conjunctivitis. In contrast, a follicular reaction in the conjunctiva appear more as dome-shaped nodules, which are a core of lymphocytes and mononuclear cells (Figure 2). Follicular reaction is more common in infectious conjunctivitis. These exam findings are best elicited with careful inspection of the conjunctiva and the fornices. Use of a fluorescein stain with a Wood’s lamp, especially in an urgent care setting where a slit lamp may not be readily accessible, can be helpful in highlighting these conjunctival changes.11
- Other exam findings – Relative to bacterial conjunctivitis, viral disease is more commonly associated with other systemic symptoms such as fever, adenopathy, and pharyngitis; however, eye redness may be the only manifestation of disease. A small, tender preauricular lymph node may be suggestive of adenovirus.9 As herpes simplex virus (HSV) and varicella (VZV) can cause conjunctivitis but also keratitis, a careful examination of the surrounding eyelid and skin for vesicles and dendritic fluorescein staining pattern can be useful in differentiating among HSV, VZV, and other viral causes.9 Bacterial conjunctivitis may be associated with local bacterial disease as is common in the conjunctivitis-otitis syndrome.13
Epidemiology
A prospective study of children aged 6 months to 17 years seen in an urban pediatric emergency department (ED) with conjunctivitis found that bacterial culture was positive in approximately 65% of cases, with Haemophilus influenza and Streptococcus pneumoniae the most frequently isolated pathogens.14 Staphylococcus aureus and Moraxella catarrhalis were also commonly identified. Viral causes of infectious conjunctivitis in children include adenovirus (often associated with fever and pharyngitis) but also coxsackie and enteroviruses among others.
Treatment
In cases in which viral etiology is highly suspected (ie, older children, bilateral disease, watery discharge, significant itching, etc.) treatment is supportive with preservative-free artificial tears for comfort as needed and observation at home.11 The focus should be on preventing spread of disease using good hygiene and some isolation.
In cases in which routine bacterial etiology is highly suspected, treatment with topical antibiotic therapy is recommended. However, it is worth noting that most forms are self-limited, and vision-threatening outcomes are exceedingly rare. In one study, 86% of children given antibiotic drops had resolution of symptoms by day 7, compared with 83% of children given a placebo drop.
Resolution of symptoms, even among cases of bacterial conjunctivitis, seems only marginally accelerated with the use of antibiotic drops. In a recent Finnish study, children treated with moxifloxacin drops had resolution of symptoms in 3.8 days vs 4.0 days in children treated with placebo (carboxymethylcellulose drops). Interestingly, patients receiving no treatment took the longest for clinical recovery (5.7 days). This finding suggests there may be an irrigation or “washout effect,” as prior studies have also demonstrated similar times to resolution between antibiotic and placebo eye drops.15
In cases that are ambiguous and mild, a watch-and-wait approach is reasonable. This practice has been found to reduce antibiotic use without significantly altering outcomes. While more rare and mild, adverse reactions still occur 5-10% of the time with use of antibiotic eye drops.12 There are also more practical considerations for delaying/avoiding immediate antibiotics, including financial and logistical burdens for caregivers to pick up the prescription, as well as frustrations and emotional trauma surrounding the administration of eye drops or ointments in younger children.
The wait-and-see approach, for parents who are agreeable, entails writing a prescription for topical antibiotic but recommending that it be filled only if symptoms persist or worsen after 72 hours. While this practice may make some parents nervous, it is highly improbable that this delay will affect any long-term outcome. It has been shown that only half of the delayed antibiotic prescriptions are filled, and there is only an approximately 12-hour difference in time to resolution of symptoms when using this approach. Delayed prescribing options also can allow providers to discuss the clinical course and self-resolving nature of conjunctivitis which has led to improved patient satisfaction and decreased revisits for conjunctivitis.
For patients and families in which the child’s return to school or daycare is the primary concern, it is not unreasonable to start immediate topical antibiotic therapy, though discussion of the limited treatment benefit and self-resolving nature of conjunctivitis is encouraged.
Antibiotic Selection
The most common causative organisms in cases of bacterial conjunctivitis are similar to those expected for otitis media: H influenzae, S pneumoniae, and M catarrhalis. While resistance may exist among these organisms at varying rates depending on geography, the clinical implications of this are uncertain, and resolution does not seem to be meaningfully affected by antibiotic selection in cases of uncomplicated conjunctivitis.17
Outside of special situations (eg, neonatal, contact lens use, etc.) antibiotic recommendations are generally based on expert opinion; therefore, practical considerations should be taken into account. For example, frequency of dosing and ointment vs drop formulation can make a significant impact on both the patient’s and parents’ experience of treating the infection. Additionally, the cost of various ophthalmic antibiotic preparations can vary significantly.
Since most cases of bacterial conjunctivitis will resolve quickly without long-term sequelae, if using an antibiotic, it’s preferable to choose the most logistically practical agent. Reasonable first-line options include trimethoprim-polymyxin B (Polytrim) drops or erythromycin ointment. Ointment is preferred, based mostly on expert opinion, for its ease of administration in smaller children.
Corticosteroids
Many ophthalmic antibiotic preparations exist in combination with a corticosteroid (eg, dexamethasone, prednisolone). It is important to note that ocular steroids can have significant adverse reactions and have no role in treating infectious or undifferentiated conjunctivitis. They may be rarely prescribed by an eye specialist as a later-line treatment for allergic conjunctivitis. These agents are for symptom management only and should be deferred to an eye specialist rather than prescribed from urgent care.
Special Cases And Considerations
Neonatal Conjunctivitis
Conjunctivitis in an infant under 1 month of age is referred to as ophthalmia neonatorum. Vertical transmission of N gonorrhoeae (NG) and C trachomatis (CT) are of concern, though incidence has decreased in the U.S., primarily due to routine screening and treatment of pregnant mothers. Prophylaxis for neonatal conjunctivitis with topical erythromycin administered after birth is considered standard of care, though this is thought to be only effective in reducing gonococcal transmission.
Various other bacterial and viral pathogens may cause conjunctivitis in infants <30 days of age. Epidemiology of various pathogens in such cases varies widely. In general, it is advisable to obtain polymerase chain reaction (PCR) testing for HSV, CT, and NG, as well as gram stain and culture in cases of conjunctivitis presenting in the first month of life. Maternal sexually transmitted infection history should also be obtained.
The Centers for Disease Control and Prevention and American Academy of Ophthalmology recommend treatment of ocular CT, NG, and/or HSV infection in the neonate with appropriate systemic anti-infective agents. , Therefore, if immediate ophthalmologist consultation is not feasible, it is prudent to refer patients immediately to the ED as disseminated infection can occur and real-time identification of pathogens is generally not possible.
Contact Lens Use
Children and adolescents with red eye and history of contact lens use warrant a distinct approach. Contact lens use can cause eye irritation and conjunctival infection due to alterations of tear production/dry eye. However, contact lenses can cause corneal hypoxia, as well, resulting in giant papillary conjunctivitis, corneal ulcer, neovascularization of the cornea, or keratitis. A fluorescein exam with UVB light (eg, Wood’s lamp) is indicated in patients with painful or red eyes and history of contact lens use. Patients with corneal defects require prompt ophthalmology evaluation.
Additionally, the material contact lenses are made of predisposes to gram-negative infection of the conjunctiva and cornea, particularly Pseudomonas. Prolonged use and inappropriate contact lens hygiene increase these risks. This has important implications for antibiotic selection. Fluoroquinolone (eg, ofloxacin, ciprofloxacin) or aminoglycoside (eg, gentamicin) ophthalmic drops are recommended in patients with conjunctivitis. Additionally, it is prudent to err on the side of antibiotic treatment and ensure that patients do not resume contact lens use until symptoms have entirely resolved.9
Bartonella
Approximately 2-3% of patients with cat scratch disease from B henselae develop Parinaud oculoglandular syndrome. Tender lymphadenopathy—especially preauricular, submandibular, and upper cervical lymph nodes—with a usually unilateral follicular conjunctivitis in the setting of recent exposure to cats (especially kittens) is characteristic of this condition. A decrease in visual acuity may suggest neuroretinitis from B henselae. If suspected, obtaining serology is a reasonable first step. For titers, immunoglobulin M (IgM) ≥1:20 or immunoglobulin G (IgG) ≥1:256 are indicative of active disease. These patients should be referred to ophthalmology and/or an infectious disease clinician for close follow-up and continued management.
Herpes Simplex Virus
HSV typically presents as a follicular conjunctivitis with vesicles on the skin or eyelid margin. It is of particular concern in neonates born to a mother with an active genital HSV infection/outbreak. In older children, a history of cold sores can also be suggestive. A dendritic staining pattern on the cornea can be seen in HSV keratitis, but may be present in as few as 15% of cases. Therefore, absence of ulceration or dendritic pattern should not be used to exclude this diagnosis. Oral antivirals (rather than topical) should be initiated in cases in which there is suspicion of HSV conjunctivitis or keratitis. These patients should be followed closely by an ophthalmologist given the potential for corneal scarring that can lead to amblyopia or astigmatism.
Back To School
Once a diagnosis of infectious conjunctivitis has been established, caregivers and clinicians should offer guidance as to when a child may responsibly return to the classroom or daycare. These concerns may be heightened since the COVID-19 pandemic, in which strict return-to-work and school protocols were widely recommended and implemented.
Unfortunately, the wide array of bacterial and viral pathogens that cause infectious conjunctivitis in children make specific or precise guidance difficult. Many common pathogens are spread via hand-to-eye contact (as well as via respiratory droplets) so handwashing, covering coughs, and maintenance of a clean classroom space should be encouraged. Both viral and bacterial causes are highly contagious in a school setting; however, the AAP Redbook recommends against excluding afebrile, otherwise healthy children with conjunctivitis from school or daycare given the mild and self-resolving nature of the illness. More education should be offered to schools and daycares to avoid policies that exclude children with typical cases of infectious or undifferentiated conjunctivitis.
Take-Home Points
- The vast majority of infectious conjunctivitis in children is self-limited, regardless of etiology.
- While many children present with parental concerns for “pink eye,” it is important to maintain a complete differential and perform a thorough exam, as other causes of eye redness and discomfort can be vision-threatening if missed.
- The first step in diagnosing infectious conjunctivitis is excluding noninfectious causes that have distinctly different management pathways.
- Viral conjunctivitis is suggested in patients with prodrome symptoms (eg, fever, pharyngitis, fatigue, etc.), age >6 years, lack of glued eyes, lack of purulent discharge, follicular reaction, preauricular lymphadenopathy, and/or frequent tearing.
- Bacterial conjunctivitis is suggested in patients with copious purulent drainage, young age, papillary reaction, and local suppurative symptoms (eg, otic conjunctivitis).
- Except in cases of contact lens use, antibiotic selection should be guided by practical considerations such as cost and ease of administration.
- In patients with mild bacterial disease or inconclusive infectious disease, a watch-and-wait approach is a reasonable option, depending on return-to-school considerations.
- Special considerations include neonatal conjunctivitis, contact lens use, Bartonella/history of cat scratch exposure, and HSV conjunctivitis, each of which requires specific management, often in conjunction with an ophthalmologist.
Manuscript submitted April 1, 2023; accepted for publication July 3, 2023.
Author affiliations: Julian P. Ponsetto MD, Pediatrics, Legacy GoHealth Urgent Care, Portland, OR. Momoko K. Ponsetto MD, Department of Ophthalmology, Casey Eye Institute, Oregon Health and Science University, Portland, OR.
References
- Amanda Montalbano, Jonathan Rodean, Juhi Kangas, Brian Lee, Matt Hall; Urgent Care and Emergency Department Visits in the Pediatric Medicaid Population. Pediatrics April 2016; 137 (4): e20153100. 10.1542/peds.2015-3100
- La Rosa M, Lionetti E, Reibaldi M, Russo A, Longo A, Leonardi S, Tomarchio S, Avitabile T, Reibaldi A. Allergic conjunctivitis: a comprehensive review of the literature. Ital J Pediatr. 2013 Mar 14;39:18. doi: 10.1186/1824-7288-39-18. PMID: 23497516; PMCID: PMC3640929.
- Dua HS, Ting DSJ, Al Saadi A, Said DG. Chemical eye injury: pathophysiology, assessment and management. Eye (Lond). 2020 Nov;34(11):2001-2019. doi: 10.1038/s41433-020-1026-6. Epub 2020 Jun 22. PMID: 32572184; PMCID: PMC7784957.
- Wong AH, Barg SS, Leung AK. Seasonal and perennial allergic conjunctivitis. Recent Pat Inflamm Allergy Drug Discov. 2014;8(2):139-53. doi: 10.2174/1872213×08666140704113452. PMID: 25000933.
- Abd-El Hakeem MT, Abdallah A, Abdelmoneim R, Khaleel A, Abdallah R. Different Modalities for Management of Pediatric Epiphora. Clin Ophthalmol. 2023 Apr 19;17:1193-1201. doi: 10.2147/OPTH.S406836. PMID: 37155484; PMCID: PMC10122860.
- Shimmura S, Shimazaki J, Tsubota K. Results of a population-based questionnaire on the symptoms and lifestyles associated with dry eye. Cornea. 1999 Jul;18(4):408-11. doi: 10.1097/00003226-199907000-00003. PMID: 10422851.
- Tugal-Tutkun I. Pediatric uveitis. J Ophthalmic Vis Res. 2011 Oct;6(4):259-69. PMID: 22454749; PMCID: PMC3306124.
- Rietveld RP, van Weert HC, ter Riet G, Bindels PJ. Diagnostic impact of signs and symptoms in acute infectious conjunctivitis: systematic literature search. BMJ. 2003;327(7418):789
- Mahoney MJ, Bekibele R, Notermann SL, Reuter TG, Borman-Shoap EC. Pediatric Conjunctivitis: A Review of Clinical Manifestations, Diagnosis, and Management. Children (Basel). 2023 Apr 29;10(5):808. doi: 10.3390/children10050808. PMID: 37238356; PMCID: PMC10217501.
- Patel PB, Diaz MC, Bennett JE, Attia MW. Clinical features of bacterial conjunctivitis in children. Acad Emerg Med. 2007 Jan;14(1):1-5. doi: 10.1197/j.aem.2006.08.006. Epub 2006 Nov 21. PMID: 17119185.
- Leung AKC, Hon KL, Wong AHC, Wong AS. Bacterial Conjunctivitis in Childhood: Etiology, Clinical Manifestations, Diagnosis, and Management. Recent Pat Inflamm Allergy Drug Discov. 2018;12(2):120-127. doi: 10.2174/1872213X12666180129165718. PMID: 29380707.
- Epling J. Bacterial conjunctivitis. BMJ Clin Evid. 2012 Feb 20;2012:0704. PMID: 22348418; PMCID: PMC3635545.
- Bingen E, Cohen R, Jourenkova N, Gehanno P. Epidemiologic study of conjunctivitis-otitis syndrome. Pediatr Infect Dis J. 2005 Aug;24(8):731-2. doi: 10.1097/01.inf.0000172939.13159.3b. PMID: 16094231.
- Meltzer JA, Kunkov S, Crain EF. Identifying Children at Low Risk for Bacterial Conjunctivitis. Arch Pediatr Adolesc Med. 2010;164(3):263–267. doi:10.1001/archpediatrics.2009.289.
- Rose PW, Harnden A, Brueggemann AB, Perera R, Sheikh A, Crook D, Mant D. Chloramphenicol treatment for acute infective conjunctivitis in children in primary care: a randomised double-blind placebo-controlled trial. Lancet. 2005 Jul 2-8;366(9479):37-43. doi: 10.1016/S0140-6736(05)66709-8. PMID: 15993231.
- Honkila M., Koskela U., Kontiokari T., Mattila M.-L., Kristo A., Valtonen R., Sarlin S., Paalanne N., Ikäheimo I., Pokka T., et al. Effect of Topical Antibiotics on Duration of Acute Infective Conjunctivitis in Children: A Randomized Clinical Trial and a Systematic Review and Meta-Analysis. JAMA Netw. Open. 2022;5:e2234459. doi: 10.1001/jamanetworkopen.2022.34459.
- Everitt HA, Little PS, Smith PW. A randomised controlled trial of management strategies for acute infective conjunctivitis in general practice. BMJ. 2006 Aug 12;333(7563):321. doi: 10.1136/bmj.38891.551088.7C. Epub 2006 Jul 17. Erratum in: BMJ. 2006 Sep 2;333(7566):468. PMID: 16847013; PMCID: PMC1539078.
- The Wills Eye Manual, Chapter 5, “Conjunctiva/Sclera/Iris/External Disease,” 4th ed, Kunimoto DY, Kanitkar KD, and Makar MS, eds, Philadelphia, PA: Lippincott Williams & Wilkins, 2004.
- Berger W.E., Granet D.B., Kabat A.G. Diagnosis and Management of Allergic Conjunctivitis in Pediatric Patients. Allergy Asthma Proc. 2017;38:16–27. doi: 10.2500/aap.2017.38.4003.
- Khan A, Anders A, Cardonell M. Neonatal Conjunctivitis. Neoreviews. 2022 Sep 1;23(9):e603-e612. doi: 10.1542/neo.23-9-e603. PMID: 36047752.
- Mallika P, Asok T, Faisal H, Aziz S, Tan A, Intan G. Neonatal conjunctivitis – a review. Malays Fam Physician. 2008 Aug 31;3(2):77-81. PMID: 25606121; PMCID: PMC4170304.
- Centers for Disease Control and Prevention, accessed August 29, 2023, https://www.cdc.gov/conjunctivitis/newborns.html
- American Academy of Ophthalmology, access August 29, 2023, https://eyewiki.aao.org/Neonatal_Conjunctivitis
- Kates M.M., Tuli S. Complications of Contact Lenses. JAMA. 2021;325:1912. doi: 10.1001/jama.2020.20328
- Carithers HA: Oculoglandular disease of Parinaud: a manifestation of cat-scratch disease. Am J Dis Child 1978, 132:1195-1200.
- Omerod LD, and Dailey JP: Ocular manifestations of cat-scratch disease. Curr Opin Ophthalmol 1999;10: pp.209-216.
- Murakami K, Tsukahara M, Tsuneoka H, et al. Cat scratch disease: analysis of 130 seropositive cases. Journal of infection and chemotherapy: official journal of the Japan Society of Chemotherapy. 2002;8(4):349-352.
- Austin A, Lietman T, Rose-Nussbaumer J. Update on the Management of Infectious Keratitis. Ophthalmology. 2017 Nov;124(11):1678-1689. Doi: 10.1016/j.ophtha.2017.05.012. Epub 2017 Sep 21. PMID: 28942073; PMCID: PMC5710829.
- Darougar S, Wishart MS, Viswalingam ND. Epidemiological and clinical features of primary herpes simplex virus ocular infection. Br J Ophthalmol. 1985 Jan;69(1):2-6. doi: 10.1136/bjo.69.1.2. PMID: 3965025; PMCID: PMC1040512.
- Schwartz GS, Holland EJ. Oral acyclovir for the management of herpes simplex virus keratitis in children. Ophthalmology 2000;107:278-282.
- Beneish RG, Williams FR, Polomeno RC, et al. Herpes simplex keratitis and amblyopia. J Pediatr Ophthalmol Strabismus. 1987;24:94–96.
- American Academy of Pediatrics, “Management and Prevention of Infectious Diseases”, Red Book: 2021–2024, Report of the Committee on Infectious Diseases, Committee on Infectious Diseases, David W. Kimberlin, MD, FAAP, Elizabeth D. Barnett, MD, FAAP, Ruth Lynfield, MD, FAAP, Mark H. Sawyer, MD, FAAP.


