Urgent message: Even a seemingly minor hand injury can result in lifelong disability if evaluation and treatment are incorrect.
TRACEY QUAIL DAVIDOFF, MD
Introduction
The hand is a vital part of human anatomy allowing us to interact with our environment in nearly infinite ways. The functional aspects of the hand are a direct extension of the brain, allowing us to initially make stone tools, play musical instruments, make intricate crafts, type, communicate, and appreciate our environment through gestures and touch.1
Our hands are also generally exposed to others, so not only must the hand work properly, it must not appear deformed, lest it be a source of discomfort and embarrassment. For these reasons, injuries to the hand can be seriously disabling. The best possible outcome often depends on accurate initial evaluation and treatment. Proper evaluation and treatment of hand injuries is essential because what often seems like relatively minor injuries can result in lifelong disability. The most common complication of hand injuries is chronic pain and stiffness.2
Hand injuries are very common and account for a large part of urgent care visits. Many of these are work- or sports-related. Hand injuries can be divided into open and closed. Due to constraints of space and different management of these injuries, only closed injuries will be discussed here. Injuries proximal to the carpometacarpal (CMC) joint will not be discussed
Her last article for JUCM was Burns: Their Evaluation and Treatment in Urgent Care (May 2011), available on the JUCM website. This article is adapted from a presentation on closed hand injuries that Dr. Davidoff will deliver at the UCA convention in Las Vegas next April.Tracey Quail Davidoff is a staff physician at Excelcare Medical Urgent Care and Urgent Care by Lifetime Health, both in Rochester, New York. She is board-certified in internal medicine and worked for 18 years as an emergency physician before switching to urgent care four years ago.
Terminology
Accurate charting is essential in the evaluation and treatment of hand injuries. Specialist referrals are com- mon, and subsequent providers need to compare what they currently see with what happened when you first saw the patient. Your chart will communicate to the spe- cialist (and malpractice, disability, and/or workmen’s compensation attorney) the specifics of mechanism of injury, functional impairment, and deformity, as well as treatment you provided. Uniform terminology and ade- quate documentation is key to making sure everyone understands what you have seen and done.
The surfaces of the hand and digits are described as “dorsal” (top) and “volar” (palm). Each side of the hand and finger is described as “radial” and “ulnar,” respectively. The muscle at the base of the thumb is called the “thenar eminence,” and the corresponding opposite side is the “hypo thenar eminence.” The names of the fingers can often be confusing if numbers are used, so it is recommended that each finger be named individually; thumb, index, middle, ring, and pinky, little, or subtle findings may only be seen in one view. Additional views may be ordered to further delineate injuries. Comparison views with the uninjured side may also be helpful in discriminating Salter fractures in children.
Classification and Treatment
Distal phalanx injuries
Distal phalanx fractures represent about one-third of all hand fractures.2 The mechanism of injury is usually crush or shearing force, such as a missed grab during sports. Tendon injuries are common with fractures of the distal phalanx, as both flexor and extensor tendons attach to it. These tendons can easily cause avulsion frac- tures when subjected to excessive stress. On exam, there is loss of function of the tip of the finger, which is easily demonstrated by holding the middle phalanx stable and asking the patient to bend/extend the tip of the fin- ger. On x-ray, only a small avulsion may be seen.
Extra-articular fractures of the distal phalanx usually result from a direct blow to the tip of the finger. The force of the blow determines the severity of the fracture. Comminuted fractures are the most common. On examination, there is typically tenderness and swelling over the distal phalanx. Subungual hematomas are common and indicate a laceration of the nail bed. Complete or incomplete avulsion of the nail plate may also occur with these injuries. AP and lateral views are the best for diagnosing this fracture.
Non-displaced or minimally displaced fractures are best managed with a splint, elevation, and pain medication. A volar or hairpin splint is recommended to accommodate swelling, which can be severe. Typically splinting is required for three to four weeks. Comminuted fractures can remain painful for several months. Fractures with significant displacement or angulation should be reduced. Volar splinting should be applied and the radiographs repeated to confirm reduction. Reduction is often difficult due to severe soft tissue swelling that may lodge between the fragments. If reduction is not satisfactory, a Kirshner wire (K-wire) may be needed to prevent non-union and subsequent loss of function.
Intra-articular fractures of the distal phalanx can be dorsal or volar. Dorsal intra-articular fractures are referred to as “mallet finger” and result from forced flexion with the finger in taut extension. This commonly occurs in sporting injuries (eg, basketball, baseball, and softball players) when the ball accidentally hits the tip of the finger causing forced flexion. It is the most common finger injury in ath- letes.3 If the tendon is completely ruptured the patient will not be able to actively extend the fingertip. The tendon may rupture with- out a fracture being present.Subungual hematomas should be drained for patient comfort. If the nail plate is intact, it need not be removed to repair the nail bed. Trephination using electrocautery or a heated 18-g needle can be used for drainage if the hematoma is greater than 50% and less than 24 hours old. If the nail plate is disrupted, the fracture is considered open, but can still be repaired in the urgent care center (see Assess- ment and Initial Care of Fingertip and Nailbed Injuries [November 2008], posted on the JUCM website).
The tendon may also stretch without being ruptured. In this case, some degree of active extension may still be present. Occasionally, dislocation may also occur. Nail plate injuries may also occur. A lat- eral view of the finger is the best for demonstrating this injury.
Non-displaced or minimally displaced fractures with reliable patients can be treated conservatively with a dorsal splint with the distal interphalangeal (DIP) joint in extension. The finger must be maintained in this position for six to eight weeks continuously. Flex- ion at any point during this period may result in a chronic flexion deformity. If the splint needs to be changed the patient should place his hand on a table to prevent bending. Unreliable patients should have the finger casted. Most patients should be referred to a hand specialist. In some cases, surgical fixation with K-wires may be per- formed. Improper treatment of these fractures may result in a swan- neck deformity from the imbalance between the ruptured extensor tendon and the unopposed distal flexor tendon.
Volar intra-articular fractures are associated with injury to the flexor profundus tendon insertion. This is an uncommon injury resulting from forceful hyperextension while the finger is tightly flexed. The patient will be unable to flex the distal phalanx. There may be tenderness over the volar aspect of the distal phalanx or even the palm due to tendon retraction after injury. Patients with traumatic swelling and tenderness over the volar aspect of the distal phalanx with additional palmar pain should be considered to have a rupture of the flexor profundus tendon until proven otherwise.2 The lateral view is the best for demonstrating this fracture.
In the urgent care setting, the patient should be placed in a volar splint. The patient should be referred to a hand specialist for early surgical fixation. Complications of this injury include non-union and loss of flexion of the distal phalanx.
Middle and Proximal Phalanx
Anatomically, in mechanisms of injury, and in treatment, the middle and proximal phalanx are similar and will be dis- cussed together.
There are no tendons that attach to the proximal pha- lanx. When fractured, unopposed tension of the interosii and extensor tendons causes volar angulation. When middle phalanx fractures occur, it is usually in the thinner shaft. Middle phalanx fractures are relatively uncommon, as axial forces subjected during injury are more likely to be absorbed by the proximal phalanx, making its fracture more common.4 Dislocations at the proximal interphalangeal (PIP) joint are more likely to occur than middle phalanx fractures. Although long tendons do not attach at the middle phalanx, they do lie in close proximity, which needs to be considered when treating fractures and dislocations in this area.
Middle and proximal phalanx fractures should never be immobilized in full extension. They should always be in a position of function to prevent stiffness and con- tractures. If the fracture or dislocation is reduced but can only be maintained in full extension, the patient should be referred to a hand specialist urgently for surgical fixation (Figure 1).
Metacarpal Fractures 2-5
The second and third metacarpals are generally immo- bile; therefore, they should be treated like long-bone fractures with reduction to anatomic position. Since the fourth and fifth metacarpals are mobile, some dis- placement can be tolerated. Patients with metacarpal fractures may also have (CMC) joint dislocations, which can easily be missed on initial presentation.3
Metacarpal fractures can be classified as head, neck, shaft, or base. Head fractures are usually due to direct blow, crush, or penetrating force. They are often com- minuted. Urgent care consists of ice, elevation, and splinting. Referral to a hand specialist is indicated.
The most common metacarpal neck fracture is the fifth metacarpal “boxer’s fracture” (Figure 2), although small, as opposed to one through five.
Anatomy
The hand is a highly mobile set of gliding bones connected by tendons and ligaments to a fixed center. It consists of 27 bones: 14 phalangeal bones, five metacarpals, and eight carpal bones, arranged in five “rays,” atop two rows of four carpal bones each. Each ray contains a metacarpal and three phalangeal bones, except for the thumb, which has only two phalanges. The carpometacarpal joints are mobile at the thumb, ring, and pinky and fixed at the index and middle rays, allowing a grasping motion around a fixed center. Capsular or collateral ligaments of each joint provide stability, and the tendons of the intrinsic muscles of the hand provide mobility.
Their origins and insertions lie within the hand and include the muscles of the the nar and hypothenar eminences, adductor pollicis, the interossei, and the lumbricals. The flexor tendons insert on the volar surface of the hand, originating in the fore- arm, and the extensor tendons insert on the dorsal surface of the hand, also originating in the forearm. For a more comprehensive review of anatomy, please refer to your favorite anatomy text.
History
When a patient presents for a hand injury, the history should include the date and time of injury, the mechanism of injury, the position of the fingers and hand during the injury, and what the patient did immediately after the injury. Other useful facts to note are hand dominance, age, gender, occupation, hobbies that require manual dexterity, whether the injury occurred at work, previous injuries in the same area, and any preexisting diseases such as arthritis or vascular disease.
The mechanism of injury should be detailed, such as crush, forced flexion or extension, or jammed, the direc- tion of force, and whether chronic repetitive trauma is an issue. It is important to know the profession or hob- bies of the patient—eg, surgeon, pianist, or construction worker—as these patients may carry a more significant morbidity than those patients who do not rely on fine motor skills for their income.
Physical Exam
All patients with hand injuries require a thorough phys- ical evaluation. Most providers find it useful to have a standard exam that they perform on all patients so that an occult injury is never missed. This exam should include testing of all tendons and motor, sensory, and vascular components. The injured hand should be com- pared to the uninjured hand. Inspection should start with the hand in neutral position and then balled into a fist. Include any evidence of deformity, bruising, swelling, lacerations, etc. When the patient makes a fist, injury is suspected when the nail beds do not form a straight line or all fingers of the closed hand do not point to the proximal scaphoid. Careful attention should be given to note any rotational malalignment of the fingers out of their normal position.
The bones and joints should be palpated to assess for point tenderness. Range of motion of the fingers should be tested passively, actively, and against resistance. This includes flexion and extension, as well as stability of the collateral ligaments. Abnormal passive range of motion may indicate laxity of joints caused by a complete or partial tendon rupture. Pain in motion against resistance may be the only clue of an occult partial tendon injury. Ask the patient to make a fist and resist your trying to pull his fingers out. Move the injured area passively, then have the patient move it, and then test flexion and extension against resistance. Bending the distal phalanx while holding the middle phalanx stable tests the flexor digitorum profundis. Bending a finger while the others are held in extension against a flat surface tests the flexor digitorum superficialis.
Bending the tip of the thumb while the proximal phalanx is stabilized tests the flexor pollicis longus. Spreading fingers tests the dorsal interossei muscles, and unspreading them tests the palmar interossei. Have the patient oppose his thumb to the tip of the each finger and then resist as you try to separate them. Finally, ask the patient to place his hand palm down on a table and lift the thumb.
Vascular status should be assessed by testing pulses or capillary refill distal to the injury. Capillary refill in most hemodynamically stable patients is <3 seconds. Sensation distal to the injury should be tested grossly to light touch and pain. Finally, two-point discrimination should be tested in the fingertips. Normal two-point discrimination should be <6mm but is often <2mm. This should be tested at least two times on either side of the pad of the affected digit.
A well-planned exam will test all joints; flexor, extensor, and intrinsic muscles; median, ulnar and radial nerves, both sensory and motor; and vascular status.
Imaging
Generally, three views of the hand or injured distal finger should be completed: anteroposterior (AP), lateral, and oblique. Do not settle for suboptimal films, as sub this fracture can occur in the third and fourth metacarpals as well. In the fifth metacarpal, the fracture is usually unstable with volar angulation. Angulation of up to 40 degrees in the fifth metacarpal, 20 degrees in the fourth metacarpal, and 15 degrees in the second and third metacarpals will not result in limitation of function. More angulated fractures should be reduced. The hand should be splinted with the wrist in about 20 degrees of extension and the metacarpals at 90 degrees of flex- ion. Second or third metacarpals may ultimately require fixation to preserve anatomic position.
Metacarpal shaft fractures usu- ally occur from a direct blow. Rotational deformity is common due to the forces of the interossei. Most of these fractures require operative fixation. Urgent care management should include splinting and referral to a hand specialist (see Figure 3).
Metacarpal base fractures are usually due to a direct blow and are commonly associated with carpal fractures as well. Base fractures at the fourth and/or fifth metacarpal can result in paralysis of the ulnar nerve. Urgent referral is recommended.
Thumb Metacarpal Injuries
Because the thumb metacarpal is so mobile, fractures usually occur at the base. Extra-articular fractures are the result of a direct blow or impaction. Twenty degrees of angulation is functionally tolerated; otherwise reduction is required. Treatment is with a thumb Spica splint for four weeks. A spiral fracture may require fixation. Intra-articular fractures can be caused by impaction from striking a fixed object. A thumb Spica splint should be applied and the patient should be referred to a hand specialist.
Dislocations
Dislocations of the DIP are rare due to the firm attachment of the skin and subcutaneous tissue to the bone underneath. Stability is also provided by the flexor and extensor tendons. Most dislocations are dorsal when they occur. Digital block should be performed for pain management. Reduction is accomplished by longitudinal traction and hyperextension followed by pressure on the dorsum of the base of the distal phalanx. The patient should be splinted for 10-21 days.5 Specialist evaluation is only necessary if the dislocation is irreducible. This can occur from entrapment of an avulsion fracture, the profundus tendon, or the volar plate itself.
PIP dislocations are common hand injuries, especially in athletes (Figure 4). Dorsal dislocation is due to rupture of the volar plate. Lateral dislocation occurs when a collateral ligament ruptures—usually the radial collateral—causing ulnar deviation of the finger. Volar dislocations are rare.
Reduction is accomplished in the same manner as for DIP, following a digital block. After reduction, active motion and strength should be tested. If these are normal, the patient should be splinted in 30 degrees of flexion for three weeks. When the joint is irreducible or motion and strength is abnormal, the patient should be referred to a specialist for operative repair.
Metacarpophalangeal (MCP) joint dislocations are due to hyperextension causing disruption of the volar plate. The direction of dislocation is dorsal. Subluxation is actually more common. On exam, the joint appears dislocated but on radiographs the articular surfaces are still intact. Care should be taken when relocating not to hyperextend the joint, which could convert a subluxa- tion into a dislocation. Instead, the wrist should be flexed and then pressure applied to the dorsum of the proximal phalanx in a distal and volar direction. The joint should be splinted in flexion.

CMC joint dislocations are very rare due the extensive connective tissue and ligamentous structures in this area. Significant force is required; therefore, this type of dislocation is only seen in motor vehicle collisions, falls from heights, and crush injury.3 Most of these patients go to the emergency department based on mechanism alone and are rarely, if ever, seen in the urgent care setting. ED referral is warranted.
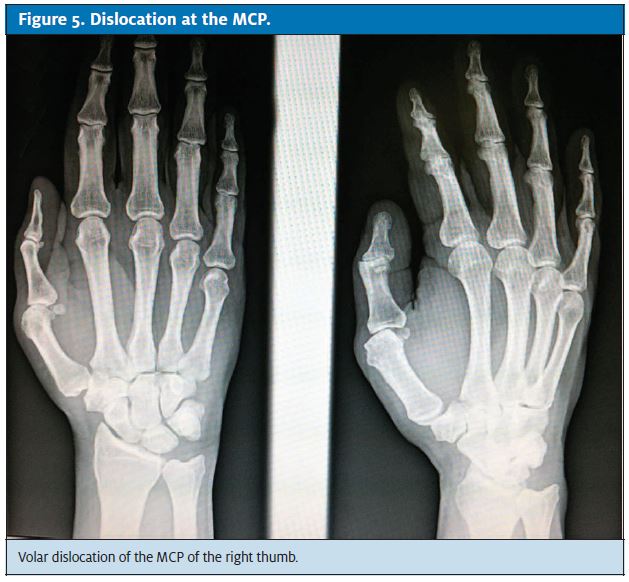
Thumb dislocations are treated differently than the other digits. Dislocation at the DIP is usually open. Dis- location at the MCP (Figure 5) results from a hyperex- tension force causing volar dislocation. The volar plate is usually ruptured. Reduction is completed with pres- sure directed distally on the base of the proximal pha- lanx, with the metacarpal in flexion and abducted.
Rupture of the ulnar collateral ligament of the MCP of the thumb is called “gamekeeper’s thumb” or “skier’s thumb.” The injury is caused by forced radial deviation, such as when a skier falls with the hand firmly grasping the pole. Weakness of pincer function is common in these injuries and can be permanent. In the urgent care setting, the patient should be placed in a thumb Spica splint and referred to a hand specialist.
Closed Tendon Injuries
A ”jersey finger” results when an athlete grabs an opponent’s jersey and the DIP is forcefully extended from the flexed position. The index finger is most commonly involved,2 but any finger can be affected. A subtle flex- ion deformity may be noted on inspection, and the patient will be unable to flex the distal phalanx when the PIP is extended. Contractures may occur in untreated patients. The patient should be placed in a dorsal splint and referred to a specialist for surgical repair.
Rupture of the central slip of the extensor tendon results from three mechanisms: deep contusion of the PIP, forceful flexion of the extended PIP joint, or volar dislocation of the PIP. Loss of complete extension with decreased strength or pain against resistance is suspicious for this injury in conjunction with the correct mechanism of injury. If untreated, the result is a “boutonniere deformity,” which may not occur until seven to 14 days after the injury.6 The PIP joint should be splinted in constant, complete extension. The patient should be referred to a hand specialist to determine the length of time the patient should be splinted or whether operative repair is required.
“Boxer’s finger” occurs from a traumatic blow to the MCP resulting in rupture of the extensor hood, as when punching. There is marked swelling and decreased mobility, and the tendon may relocate when the MCP is extended, causing pain. The radiograph is negative for fracture. The patient should be splinted in extension with the ten- don relocated and referred to a hand specialist for further management.
Be Prepared
Talk to local hand specialists and compile a referral base of several physicians for your patients with hand injuries. Check to ensure that each practice will follow- up with your patients in a timely fashion, not make them wait for weeks before evaluating them. Make sure that your specialist of choice takes the same insurances you do, so that won’t be an obstacle to care. Keep a sup- ply of that doctor’s business cards, printed contact/address information for the doctor, and perhaps driving instructions so the patient can easily find the doctor’s office. Keep the doctor’s fax number on file and fax over your evaluation so the doctor knows what to expect when the patient calls, of course maintaining HIPAA compliance at all times.
Conclusion
Hand injuries are a common presenting complaint in the urgent care center. Loss of function can have a pro- found impact on the remainder of a patient’s life. Improper management can result in permanent dis- ability for the patient and litigation for you. Learning everything you can about hand injuries, developing a process of examination that encompasses all aspects of hand function, and knowing when to refer patients to a specialist is key in successfully treating these injuries and ensuring an optimum outcome for both you and your patients.■
References
- Skinner HB. Current Diagnosis and Treatment in Orthopedics. 4th ed. New York, NY: McGraw-Hill; 2006:535-556.
- Simon, R, Sherman, S, Koenigsknect, Emergency Orthopedics: The Extremities. 5th ed. New York, NY: McGraw-Hill; 2006.
- Tintinalli J, Stapczynski J, Ma OJ, et Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw-Hill; 2010:1796-1807.
- Edwards T, Mayer Urgent Care Medicine. New York, NY: McGraw-Hill; 2002:381-390.
- Wheeless Dorsal Dislocation of the PIP Joint. In: Wheeless’ Textbook of Orthopaedics. Available at: www.wheelessonline.com/ortho/dorsal_dislocation_of_the_pip_ joint. Accessed November 17, 2011.
- Roberts JR, Hedges J, Clinical Procedures in Emergency Medicine. 4th ed. Philadel- phia, PA: Saunders; 2003;924-945, 969-974.