Urgent message: It is common for transgender patients to have a history of poor experiences with healthcare providers. As such, they may be less likely to have an ongoing clinical relationship with a primary care provider, making urgent care a likely destination when a need arises. Familiarity with issues facing adolescent transgender patients, in particular, can benefit both the provider and the patient.
Timothy McGinnis and Emily Montgomery, MD
THE CASE
A 15-year-old transgender male (pronouns he/him/his) reports to urgent care with left lower quadrant abdominal pain. The pain was initially intermittent but has been constant for the past hour. He has associated nausea and vomiting. He denies fever, chills, vaginal bleeding, vaginal discharge, diarrhea, constipation, and urinary symptoms. He has no past medical history, and states that he has not had any gender-affirming surgeries. His only medication is intramuscular testosterone. He is not sexually active. Vitals show a BP of 125/76, HR of 112, RR 16, and temp 98.6°F. Chest exam shows a chest binder in place. Lungs are clear to auscultation. He is tachycardic with a regular rhythm and no murmurs. Abdominal exam demonstrates LLQ tenderness with guarding. He consents to a pelvic exam, which reveals a left adnexal mass and tenderness, but no bleeding or discharge.
INTRODUCTION
An estimated 150,000 adolescents (age 13-17) in the United States are transgender or gender nonconforming.1 Multiple health disparities exist between transgender and cisgender adolescents.2 For example, transgender youth are more likely to attempt suicide, less likely to have health insurance, and are more likely to be homeless.2,3 Additionally, transgender patients often report poor experiences with healthcare professionals, including harassment and denial of care.3,4 Given these health disparities, urgent care and emergency clinicians are often the de facto primary care providers for the transgender population. Therefore, it is important for all urgent care providers to understand the specific clinical considerations of this population and to know and employ methods to make the healthcare experience more comfortable.
HISTORY AND EXAM PEARLS
Developing trust between a patient and provider is one of the most important aspects of healthcare is. Given the likelihood that a transgender patient has had poor interactions with healthcare providers, creating a comfortable environment can be an essential step in developing that trust.5 For example, displaying trans-friendly symbols in patient rooms or on ID badges, and providing documents/brochures for LGBTQ health concerns is a good first impression that can provide patients with some assurance that they’re in a welcoming space.2,5,6
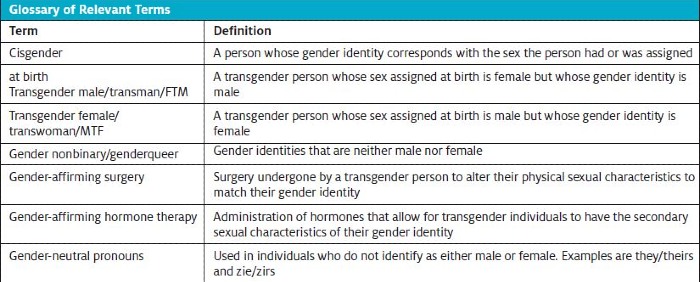
Next, recognize that it is essential to take the medical history of a transgender patient in a gender-affirming way.4 As with cisgender patients, the use of open-ended and nonjudgmental questions is paramount.2 The use of the patient’s correct pronouns is also essential.2,5 Intake forms that include questions about gender identity and pronouns can ensure providers and other staff address and refer to the patient in the manner they prefer.2 If the provider is unsure of the patient’s pronouns, asking “What is your gender identity?” or “What pronouns do you use?” can be simple and effective.7 This will also show that you respect and value their gender identity.
A special consideration of the medical and surgical history in transgender patients is taking an anatomic/organ inventory.2,7 While it is less likely that pediatric patients will have undergone gender-affirming surgery, this knowledge is important as it may influence the differential diagnosis. However, it is important to know that some transgender patients may feel uncomfortable disclosing this information due to fear of judgement or discrimination.4 If this happens, providers can explain that this is information is necessary to make medical decisions and will remain confidential.7 A simple question to elicit this information is “Have you undergone any gender-affirming surgeries?” If they answer yes, a more in-depth history can be taken.7
Another unique consideration in the transgender population is asking about gender-affirming hormone therapy. Hormone therapy and puberty-blocking medications are more common than gender-affirming surgery in the pediatric population. Gonadotropin-releasing hormone (GNRH) analogs (leuprolide and histrelin) are often used in transgender and gender-diverse adolescents.8 These medications delay the onset of puberty, allowing adolescents more time to determine gender identity and research medical transition therapy, like hormones.2,8 This effect is reversible. Common side effects to be aware of in this medication class are hot flashes, gynecomastia (which may or may not be desired), weight gain, and fluid retention.9 There is an increased risk of osteoporosis with long-term use of these medications.9
Estrogen, progestogen preparations, and antiandrogens (spironolactone, cyproterone acetate, or 5α-reductase inhibitors) are the mainstay of feminizing gender-affirming hormone therapy.7,10 The main concern in patients on estrogen therapy is the increased risk of venous thromboembolism.10 This is an important consideration in transgender female patients who present with signs and symptoms concerning for deep vein thrombosis and pulmonary embolism. It is also necessary to assess for any contraindications to the use of estrogen, such as migraine headaches or history of hypercoagulable disease.11
Testosterone preparations are the mainstay of masculinizing gender-affirming hormone therapy.10 Testosterone use can cause erythrocytosis and elevated liver transaminases.2 Although erythrocytosis can cause an elevation in blood pressure, the risk of hypertension in transgender males on testosterone therapy is equal to that of cisgender males.2 It is also important to keep in mind that testosterone can induce amenorrhea.12
Providers should obtain a menstrual history in all adolescent transgender males. Additionally, sexual history should be elicited when deemed clinically necessary. Transgender males with an intact uterus can still become pregnant, so a thorough sexual history will help with clinical decision-making. Keep in mind that these may be sensitive topics for some patients, so the use of open-ended, nonjudgmental questions will be beneficial.
Lastly, providers should screen for mental health issues such as anxiety and depression. The transgender population has high rates of depression, anxiety, eating disorders, and suicide ideation/attempts.2 One study found that 30% of transgender patients had attempted suicide and 42% reported self-injurious behaviors.13
It is necessary to do a physical exam of all transgender patients, just as you would in a cisgender patient. However, there are a few considerations the provider should be aware of. One, is that many transgender individuals are survivors of sexual and physical assault.4 Therefore, the physical exam may be a triggering event for some individuals. Explaining the importance and reasoning behind a physical exam to the patient can be beneficial. Clinicians should perform the physical exam in a gender-affirming manner.For example, use general terms for anatomy and ask patients if they have preferred terms for certain body parts.10 Perform a focused physical exam when possible.
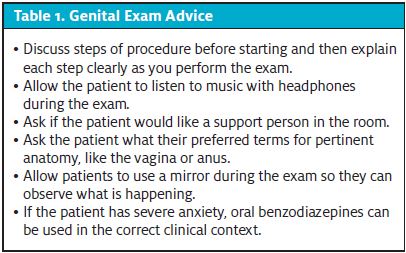
Examination of genitalia can be highly distressing to some transgender individuals, as they may have anatomy that does not align with their current gender identity. If the patient has significant anxiety about the exam or denies the exam, it can be deferred.10 Some methods to make the procedure less distressing for patients are detailed in Table 1.10
Special Considerations
Pelvic and abdominal pain
The workup and differential for abdominal and pelvic pain in pediatric transgender patients is going to be like that of cisgender patients. However, there are some special considerations in the transgender population.
In transgender males with a uterus and ovaries, it is necessary to remember to include uterine/ovarian/vaginal causes of pain in the differential (PID, uterine fibroids, ovarian torsion, etc.). The use of testosterone in transgender males can induce atrophy of the vaginal mucosa, similar to a postmenopausal cisgender female.10,15 This can lead to dyspareunia and atrophic vaginitis as causes of abdominal pain.10 Additionally, atrophy of the vaginal mucosa increases the risk for bacterial vaginosis, cervicitis, and urinary tract infections.16 Abdominal pain in transgender males on testosterone may also be associated with cyclic testosterone dosing.10 This pain is often described as cramping.
In transgender females with a penis and testes, conditions such as testicular torsion, epididymitis, and torsion of the appendicular testes should remain in the differential. A rare condition to keep in mind in transgender females is estrogen-induced hypertriglyceridemia. Exogenous estrogen use can lead to hyperlipidemia, and there are some case reports of transgender females and cisgender females who have developed pancreatitis secondary to hypertriglyceridemia while on estrogen therapy.11, 17-19
Heavy or persistent vaginal bleeding
Heavy or persistent vaginal bleeding in transgender males can be a distressing complaint.20 The differential for abnormal uterine bleeding (AUB) is the same as it is in cisgender females. The American College of Gynecology recommends the mnemonic PALM-COEIN to create a differential for AUB (Table 2).21
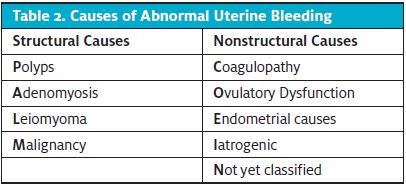
Initial workup should consist of complete blood count, pregnancy test, and possibly pelvic ultrasound based on clinician judgement.21 Additional work-up can include PT, PTT, TSH, and LFTs to assess for other causes of bleeding.21 The treatment of acute heavy vaginal bleeding in transgender males is different from that of cisgender females. Treatment options such as IV estrogen or high-dose oral contraceptives should be avoided due to the feminizing effects. If the patient is not already on testosterone, this can be started in order to induce amenorrhea.22 There are multiple testosterone formulations, but the majority use biweekly intramuscular or weekly subcutaneous forms.22 In patients already on testosterone therapy, increasing the dose may be beneficial as there is a dose-dependent response to inducing amenorrhea.22 Tranexamic acid should be used with caution in patients on testosterone, as there is a possible increased risk of thrombogenesis.23,24
Additional medical management of persistent or heavy vaginal bleeding in transgender males can include aromatase inhibitors, selective estrogen receptor modulators (SERMs), progestogens, and GNRH-agonists.22 Referral to endocrinology is also an option.
Skin breakdown and soft tissue infections
Some transgender males may use chest binders to help diminish body dysphoria. Although chest binders are relatively safe, they can cause skin breakdown or other skin issues, like infection secondary to skin breakdown.14 Therefore, if a provider has clinical suspicion for a soft tissue infection or a fever of unknown origin, remember to check for skin issues beneath chest binders. Some patients may feel uncomfortable removing binders, so providing an explanation can be beneficial.2 Providers should also be aware of tucking, a technique that allows individuals to hide any outward evidence of the penis and testes. One method involves pulling the penis backwards between the legs and then raising the testes into the inguinal canal. Another technique is employing the use of binding tape to hold the penis and testes against the perineum. Tucking is relatively safe, but there is a risk of penile pain, inguinal hernias, and skin breakdown.2
TAKE-HOME POINTS
- Many transgender patients have had poor past experiences with the healthcare system. As such, the care of transgender and nonbinary adolescents in the urgent care setting starts with creating an environment of inclusion and safety. Use of the correct pronouns and displaying outward signs of an LGBTQ-friendly environment (signs, stickers, pins) is a great start.
- When collecting past medical and surgical history, ask about puberty-blocking medications, gender-affirming hormone therapy, and gender-affirming surgeries.
- The physical exam can be distressing for some transgender patients, so explaining its importance and talking through exam maneuvers can be helpful.
- When developing a differential, consider the patient’s anatomy and whether hormone therapies are contributing to their symptoms.
- Bear in mind that transgender and nonbinary patients will often have the same complaints and diagnoses as their cisgender adolescent counterparts.
CASE CONCLUSION
CBC showed Hgb of 12.5, WBC of 7.6, and platelet count of 225. BUN was mildly elevated at 25 and Cr was 1.12. Ultrasound demonstrated a large left ovarian cyst and absence of blood flow to the left ovary on color doppler, consistent with ovarian torsion. OB/GYN was consulted and the patient was transferred for detorsion and ovarian cystectomy. He recovered without incident.
REFERENCES
- Herman JL, Flores AR, Brown TNT, et al. Age of individuals who identify as transgender in the United States. UCLA School of LawWilliams Institute. 2017. Available at: williamsinstitute.law.ucla.edu/publications/age-trans-individuals-us. Accessed November 6, 2021.
- Lapinski J, Covas T, Perkins JM, et al. Best practices in transgender health: a clinician’s guide. Prim Care. 2018;45(4):687–703.
- National Center for Transgender Equality. 2015. U.S. Transgender Survey. December 2016. Available at: http://www.ustranssurvey.org. Accessed August 18, 2021.
- Grant J, Mottet L, Tanis J, et al. National transgender discrimination survey; report on health and healthcare. National Center for Transgender Equality and National Gay and Lesbian Task Force. 2010:1–23.
- Eliason MJ, Schope R. Original research: does “don’t ask don’t tell” apply to health care? Lesbian, gay, and bisexual people’s disclosure to health care providers. J Gay Lesbian Med Assoc. 2001;5:125–134.
- American Medical Association. Creating an LGBTQ-friendly practice. Available at: www.ama-assn.org/delivering-care/population-care/creating-lgbtq-friendly-practice. Accessed
- Rosendale N, Goldman S, Ortiz GM, Haber LA. Acute clinical care for transgender patients. JAMA Internal Medicine. 2018;178(11):1535.
- Rew L, Young CC, Monge M, Bogucka R. Review: puberty blockers for transgender and gender diverse youth—a critical review of the literature. Child Adolesc Ment Health. 2020;26(1):3–14.
- LiverTox: Clinical and research information on drug-induced liver injury [internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.
- UCSF Transgender Care. Department of Family and Community Medicine, University of California San Francisco. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2nd ed. Deutsch MB, ed. June 2016. Available at: transcare.ucsf.edu/guidelines. Accessed November 6, 2021.
- Delgado BJ, Lopez-Ojeda W. Estrogen. [Updated 2021 Apr 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; January 2021. Available at: https://www.ncbi.nlm.nih.gov/books/NBK538260/.
- Unger CA. Hormone therapy for transgender patients. Transl Androl Urol. 2016;5(6):877–884.
- Peterson CM, Matthews A, Copps-Smith E, Conard LA. Suicidality, self-harm, and body dissatisfaction in transgender adolescents and emerging adults with gender dysphoria. Suicide Life Threat Behav. 2016;47(4):475–482.
- Vancouver Costal health. Transgender health information program. Binding. Available at: http://transhealth.vch.ca/social-transition-options/binding-packingtucking/binding.
- Perrone AM, Cerpolini SC, Salfi NCM, et al. Effect of long‐term testosterone administration on the endometrium of female‐to‐male (FtM) transsexuals. J Sex Med. 2009;6(11):3193–3200.
- Stika CS. Atrophic vaginitis. Dermatol Ther. 2010;23(5):514–522.
- Aljenedil S, Hegele RA, Genest J, Awan Z. Estrogen-associated severe hypertriglyceridemia with pancreatitis. J Clin Lipidol. 2017;11(1):297–300.
- Hashmi A, Smith EI, Ciutac A, Smith JC. Lesson of the month: acute pancreatitis due to hypertriglyceridaemia in a transgender woman: a complication of high-dose oral oestrogen therapy? Clin Med. 2021;21(3):228–230.
- Chaudhry A, Yelisetti R, Millet C, et al. Acute pancreatitis in the transgender population. Cureus. 2021;13(7):e16140.
- Frank SE. Queering menstruation: trans and non‐binary identity and body politics. Sociological Inquiry. 2020;90(2):371–404.
- ACOG committee opinion no. 557: management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol. 2013;121(4):891–896.
- Carswell JM, Roberts SA. Induction and maintenance of amenorrhea in transmasculine and nonbinary adolescents. Transgend Health. 2017;2(1):195–201.
- Chauncey JM, Wieters JS. Tranexamic acid. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; January 2021.
- Glueck C, Goldenberg N, Wang P. Testosterone therapy, thrombophilia, venous thromboembolism, and thrombotic events. J Clin Med. 2018;8(1):11.
Author affiliations: Timothy McGinnis, School of Medicine, University of Kansas School of Medicine. Emily J. Montgomery, MD, MHPE, FAAP Children’s Mercy Kansas City; Clinical Assistant Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine.
View Similar Articles
- Best Practices For LGBTQ-Friendly Urgent Care
- Best Practices For LGBTQ-Friendly Care In Urgent Care
- Making Your Urgent Care Center Welcoming For LGBTQ Patients
