Urgent message: LGBTQ individuals are subject to implicit and explicit bias in our society, ranging from microaggressions and antagonistic legislation to overt discrimination and harassment. This can inhibit willingness to seek medical care—and, subsequently, lead to worse health outcomes. Given the more accessible, episodic nature of urgent care, understanding how word choice and other subtle cues communicate our competency in working with LGBTQ patients can help us engender trust more quickly.
INTRODUCTION
The goals for treating LGBTQ patients (lesbian, gay, bisexual, transgender, and queer or questioning individuals) are the same as for anyone else: to facilitate physical health and social and emotional well-being. However, often due to negative previous experiences in healthcare settings (and even negative expectations for subsequent care) it can be as challenging as it is essential to create a strong, healthy therapeutic relationship with a new LGBTQ patient.
BACKGROUND
Development of sexual orientation and gender identity and expression (SOGIE) is a rite of passage for all individuals, usually coinciding with puberty. This is why it is important to not make assumptions even when working with children and adolescents. In the second decade of life, some individuals may feel something is “different” but not be able to quite put a finger on why (though it may have something to do with attraction, gender identity, or both). In middle adolescence (age 14-17), individuals may experiment sexually, which can lead to self-labeling.1
Sex and gender are frequently conflated. They are, however, separate concepts. Sex is based on genetics and/or anatomic features at birth. Thus, a newborn is commonly labelled as a boy or a girl. Gender, on the other hand, is based on binary sociocultural expectations of what a “feminine” or “masculine” person looks like and does. A cisgender individual has gender identity and/or expression that match societal expectations of the sex assigned at birth; transgender individuals do not. Some individuals do not identify with or express themselves as either gender. To be sure, such concepts are not new; other cultures and groups have recognized gender non-conforming (GNC) or gender diverse individuals for hundreds of years, if not longer.2
Other dimensions of oneself include sexual identity (eg, straight, gay, lesbian, bisexual, pansexual, same-gender-loving), sexual orientation and emotional/physical attraction, and sexual behavior—eg, men who have sex with men [MSM], women who have sex with men [WSM], etc. Sexual behavior—what people do—and identity (how people view themselves and present themselves to the world) are not always the same. Similarly, attraction is not necessarily synonymous with behavior. Further, sexual orientation can be dynamic, especially as a person figures out their identity over time.
As in other arenas, word choice matters; the challenge is that preferred words can change over time. Words fall out of favor or get repurposed. For example, “tranny” and “transgendered” are not accepted, but “queer” has been reclaimed. In fact, queer has become a catch-all term for identities that are not heterosexual or cisgender. Be aware, however, that because the word has a history of being used as a slur, certain generations may still bristle at hearing this.
LGBTQ Population Size
Estimating the size of the LGBTQ population can be difficult. Epidemiologic research often omits explicit questions about sexual orientation and gender identity, especially in younger age groups. Thus, the population may be “invisible” unless you ask the right questions. That said, whether you are aware of it or not, you are seeing patients who meet these descriptions. Approximately 11 million American adults identify as LGBTQ. Such estimates are usually obtained through self-report conducted by advocacy groups. Collecting data like these is important, because if you don’t count someone, you’re telling them they don’t count.3-9
Population Stresses
Social context encompasses a number of areas that lead to negative health outcomes for LGBTQ individuals: lack of positive role models, internalized phobias (ie, self-loathing), social stigma, loss of family support, discrimination, isolation, and even denial of healthcare services. These result in negative physical and emotional outcomes. Higher rates of homelessness, unemployment, victimization, and adverse childhood experiences (ACEs) lead to chronic stress.10
What is ‘normal?’
Ethnocentrism is the belief that one’s own culture is superior to all others. It sows the seeds of bias and preconceived notions, and furthers the idea that one’s own customs are “the only way to do things.” In the context of LGBTQ populations, it can lead to the expectation that heterosexuality is the default—in other words, heteronormativity. (Similarly, if it is expected that everyone is cisgender, cisnormativity develops. Recoil against gay or transgender populations, then, is homophobia or transphobia, respectively.) As humans, we are not defined by just one aspect of our identity. Intersectionality is how race, nationality, sexual orientation, gender identity, religion, disability, and the like play off one another, especially in the context of discrimination.
Health Disparities
The U.S. Centers for Disease Control and Prevention defines health disparities as “Preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially-disadvantaged populations.”11 Though certain aspects of health may actually be promoted by LGBTQ subpopulations, overemphasis can tip the scales into dysfunction—for example, a gay man who values physical fitness and idealizes a certain body type may find himself experiencing body dysmorphia and develop an eating disorder. Alcohol and other drugs—which may be normalized in certain LGBTQ social venues—are sometimes used to self-medicate against loneliness and depression. Substance use is linked to higher-risk sex and sexually transmitted infections, suicide attempts, and motor vehicle accidents.
Parental rejection, such as blaming the child for being bullied, is linked with negative health outcomes, especially depression and attempted suicide. An estimated 20% to 50% of homeless street youth are LGBTQ, and they may engage in “survival sex” for money, food, shelter, and/or drugs. The incidence of new HIV infections is highest in MSM, especially in younger men and men of color.12
LGBTQ seniors also experience health disparities: social and systemic isolation, and increased rates of poverty, for example. Further, older gay, lesbian, bisexual, and transgender men and women are less likely to be offered appropriate screening for cancer.1,3,5,8,12-15
Per recent, biennial Youth Risk Behavior Surveys (YRBS), about a third of LGB students have been bullied on school property, and 15% or more have been threatened or experienced violence in various settings.16 The 2019 Canadian Trans Youth Health Survey reveals even higher numbers.17 Rates may be higher still for those who cannot “hide” or “blend in” as easily. Perpetrators may be peers, of course, but also family members, teachers, coaches, employers, or even police: The victim may not know where to turn (or whom to trust) for help.
Lesbian, gay, and bisexual youth are two-to-three times more likely to attempt suicide than their heterosexual peers. Lack of family/community support, family conflicts, violence/victimization (eg, feeling unsafe at school/bullying), gender nonconformity, early sexual debut, and other mental health issues (eg, substance use) fuel this.14,18 Per the Williams Institute (2014), 45% of trans-identified youth, 46% of transmen, and 42% of transwomen reported at least one suicide attempt, to date. Those who have been rejected by an authority figure reported the highest suicidality, 60%. However, appropriate use of a transgender person’s chosen name is linked to reduced depressive symptoms and suicidal ideation.19
Perhaps surprisingly, despite all of these stressors, LGBTQ individuals tend to be resilient. Not so surprisingly, many LGBTQ individuals have come to dread healthcare visits because they have had poor experiences in the past. This can lead to avoidance and undermine development of a strong patient-provider relationship. Whereas professional societies such as the American Academy of Pediatrics (AAP) have advocated for LGBTQ populations for many years, individual providers and health systems have been slower to consider the unique needs of these groups. To be sure, recent surveys have revealed that one in three transgender respondents have had a negative experience with a healthcare provider in the preceding year. Some report having been verbally harassed or even refused medical treatment. One in four actually had to teach their provider about transgender healthcare. Insurance coverage is often an issue for transgender individuals, made all the more difficult by higher rates of unemployment in this community. Consequently, urgent care clinics (and/or emergency departments) may become their primary places of medical care. When visiting a new provider, it can be upsetting for LGBTQ individuals to have to “come out” all over again, with regard to sexual orientation and/or gender identity, especially if they experienced rejection in the past.3,6,8,14,20
Experiencing discrimination in healthcare settings is associated with delays in testing and treatment, fewer provider visits, decreased preventative health services, delays in filling prescriptions, and decreased patient satisfaction overall.
THE URGENT CARE VISIT
Opportunities to Improve Care
Sex discrimination in federally funded healthcare facilities is specifically prohibited by the Affordable Care Act. But we can do better than simply avoiding discrimination. We can work to make our clinics safe and welcoming to all people. We can train our front desk staff to tactfully navigate potentially awkward situations. We can rewrite inequitable policies.
The clinical space is a domain where we can work to display cultural humility. Two other areas that are not always considered involve follow-up: patient satisfaction surveys (are you doing a good job fixing systemic issues in giving good care?) and tracking health outcomes (such as HIV testing and alcohol misuse). You cannot easily improve what is not measured!21
The front desk
Sometimes there will be a discrepancy between a patient’s presented gender and what is on their identification card, health documentation, or medical chart. Some, but not all, medical records have a place for a patient’s chosen name. Typically it is best to ask someone, “What would you like to be called?” (accepting that this may differ from the patient’s legal name). Most transgender individuals recognize that their legal name needs to be used in certain documents, but calling someone by the name that doesn’t reflect their gender identity is “deadnaming.” This can be very offensive, especially after someone has corrected the speaker.
Additionally, it is typically best to ask someone what pronouns they use. Some medical practices use wearable buttons indicating personal pronouns or have staff simple state their own pronouns before asking. Unfortunately, some medical records are limited in how they list a patient’s chosen name or pronouns, and autogenerated letters may utilize the wrong honorific or pronouns. Misgendering a transgender individual is like a bee sting: It hurts, but the more it happens, the bigger the reaction. Things a cisgender, heterosexual person might take for granted every day are a challenge for LGBTQ individuals, and since they may even expect care to be insensitive, they are already in a defensive position. That said, conversations about names and pronouns should be handled discretely, so as not to “out” someone in the waiting room. Remember, too, that handoffs of care are not just between you and a consultant, but also among your own staff. It can be frustrating for patients when staff fail to communicate already-disclosed gender identity information to one another.5
Public areas
In addition to common areas being clean, include representation of your patients in posters, brochures, and magazines. Visual clues like rainbow pins or equality stickers will be noticed by those who “need to know.” Proactively address confidentiality concerns and post statements on nondiscrimination and visitation rules. Use gender-neutral terms on forms and in addressing individuals.
If possible, have an accessible, single-use, all-gender restroom facility for patients. Many transgender and nonbinary individuals avoid public bathrooms. Consequently, they may avoid eating or drinking at healthy intervals; this can lead to episodes of hypoglycemia, dehydration, urinary tract infections, or other kidney problems.20
Be aware of appropriate and welcoming places to refer patients to when needed for mental healthcare, for example, or management of gender-affirming hormone therapy. OutCare, which also provides continuing medical education for clinicians, has a directory of self-identified LGBTQ-competent healthcare providers. The Gay and Lesbian Medical Association (GLMA) and the Human Rights Campaign’s (HRC) Healthcare Equality Index are other places to look to help expand your network.1,2
The exam room (and beyond)
In the exam room, or even more generally the clinical space (eg, x-ray suite, phlebotomy room), there are several principles of good communication that apply for working with pretty much any patient population. First, make sure the patient is comfortable with whomever else is in the room, and allow them to decline the presence of anyone not directly responsible for their care (for example, trainees).
Providers and other staff can build rapport by setting a respectful and honest tone. In the patient interview, use open-ended questions to avoid simple yes/no responses that may imply there is a “correct” answer. “Tell me more” is a wonderful way to show you are listening and interested. Similarly, normalizing language that makes personal questions seem more general can be helpful.
Again, word choice matters, but it’s sometimes challenging because slang is always changing. If appropriate, echo back the patient’s word choice. If you are not sure what they mean, seek clarification. “Can you explain it to me?” is not meant to preclude your own research and study of, for example, gender-affirming hormone therapy, but a way to further engage with your patient. If you misspeak and misuse a word or make an incorrect assumption, acknowledge it, apologize, and move on. Ignoring the issue won’t make it go away and offering profuse and repeated apologies only amplify the error. Ultimately, patients are seeking medically knowledgeable care, and in some cases, the exam room may be the only place they can ask questions and get accurate information. Less than a third of LGBT adolescents felt they had an adult they could talk to about personal problems, for instance. Remember that you don’t need to know a patient’s sexual orientation or gender identity to create a safe space for them to disclose relevant health information.2,5
Assumptions to try to avoid include misgendering or mis-assuming the nature of a relationship or family structure. Sometimes in urgent care we do have continuity with patients, so remember that some aspects of their identity may change with time. Self-identification does not always align with behavior. For instance, an individual may have had same-sex or opposite-sex “experimentation” when they were younger but determined their sexual orientation later in life. Gender identity and expression do not imply a particular sexual orientation or practice. Similarly, acknowledging one risk (such as not using condoms) doesn’t necessarily imply the patient has other risky behaviors (such as IV drug use).2,6
Difficult Topics
Confidentiality
Confidentiality is often a big worry for adolescents—in general, they fear disclosure of sexual activity, let alone sexuality. But this is also true whenever we’re asking personal information. Some patients don’t want a “paper trail” and may not be truthful on forms. Conversely, they may wonder why they were asked certain questions if their answers are never addressed during the interview. These questions can be framed in the context of risk: “I ask these questions because I’m trying to determine what tests, if any, we should perform today.” Consider mentioning the role of the medical record as well: “Everything you tell me is between you, me, and the computer—unless you tell me you’re going to hurt yourself or someone else.” A patient may express some uncertainty about their sexuality and/or gender identity to you, but not be ready for others to know about their doubts yet, for example. This is a form of “testing the waters.”1
The sexual history
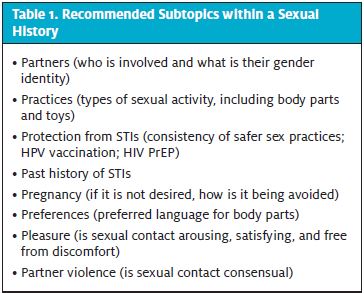
The stated reason for the visit is not always the patient’s real chief concern. LGBTQ health includes, but is not defined by, sexual health. Thus, STI screening should be based on behavior, not identity (ie, names/labels). Seek the patient’s permission to discuss sexual health topics, if appropriate. The CDC has suggested five different elements in taking a sexual history (the so-called “5 Ps”), and the National LGBT Health Education Center has suggested three more, as shown in Table 1.22,23
The physical exam
As with any patient, do not ask about—or perform unnecessary examination of—body parts not relevant to the chief concern. If necessity of an aspect of the exam is not obvious, consider explaining why you are doing what you are doing. Physical examination should be relevant to what anatomy the patient has, regardless of their gender presentation. In most institutions, a staff member chaperones intimate exams. This is probably a good habit to get into, regardless of the sex and gender of the patient and the provider. If possible, allow patients to self-collect or self-swab vaginal and anal/rectal test specimens.
Considerations related to gender affirmation
Though not every transgender individual wants to—or can afford to—undergo medical and surgical treatment (eg, puberty-blockers, onabotulinumtoxin A), knowing trustworthy consultants (eg, endocrinologists) in your area is helpful. Mental health support is probably in needed in all phases of coming out and gender-affirmation.
Social and medical affirmation (previously known as transition) can lead to unique considerations for our transgender patients. Binding one’s breasts to achieve a more masculine contour can lead to skin irritation and breakdown and reduce lung expansion, causing dyspnea or even lung infections. Taping or tucking male genitals can also lead to skin problems or hernias. Injection of silicone or other substances can lead to skin infections or worse, especially when the chemicals are not of medical-grade for humans. In the same way that some people who can’t afford a prescription for an antibiotic may use medications intended for pets, sometimes animal hormones are used. These illicit injections are also unmonitored by healthcare professionals, so supraphysiologic doses could be administered unintentionally. Even appropriately dosed and administered hormones potentially carry risks, such as cardiovascular disease, hypertension, hyperlipidemia, liver dysfunction, breast cancer, and uterine cancer. Further, there is a lack of clinical evidence as to what the long-term health effects of hormone therapy will be.8,14
It bears emphasizing that testosterone is not birth control. One way to broach the topic in a respectful way would be to ask, “I would like to order an x-ray for you. If there’s any chance you could be pregnant, we will need to check a pregnancy test first. Is that OK with you?”
Other Sources of Information
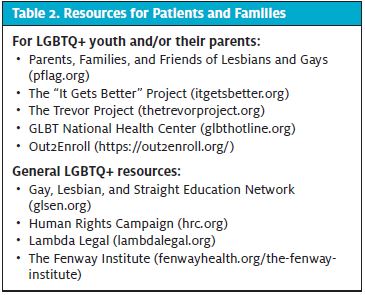
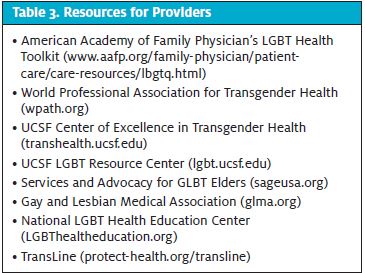
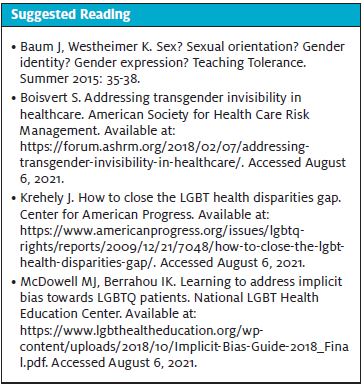
Many professional societies and health entities have their own LGBTQ resources. The American Academy of Family Physicians has an LGBT health toolkit, for example. The World Professional Association for Transgender Health (WPATH) and the UCSF Center for Excellence in Transgender Health are renowned resources for information on transgender health. Services and Advocacy for GLBT Elders (SAGE) is an organization that focuses on older LGBTQ individuals. The National LGBT Health Education Center has free CME on LGBTQ health issues. Resources for patients, their families, and providers are listed in Table 2 and Table 3.
CONCLUSION
Whether you identify as an LGBTQ individual or an ally, be engaged in your community. Allow its members to tell you what it needs. Healthcare providers can often dictate what happens in their own practices. Self-evaluation is important, as you work at every level of the socioecological model (ie, individual, interpersonal, organization, community, and societal levels) to improve care. As you would with any other group, keep learning so you can provide timely, relevant health information. Lead by example: Challenge offensive language and learn if you yourself have misspoken. We can do better to be inclusive of all our patients.
Adapted and updated from “Providing the Best Care for LGBTQ+ Patients in UC,” presented electronically for the Urgent Care Association’s 2020 annual conference.
Benjamin Silverberg, MD MSc FAAFP FCUCM, is an Associate Professor in the Departments of Emergency Medicine and Family Medicine at West Virginia University, and the Medical Director of the Division of Physician Assistant Studies in the Department of Human Performance at West Virginia University. He reports no relevant financial relationships with any commercial interests.
REFERENCES
- Garofalo R (adapted by The Fenway Institute). Caring for LGBTQ Youth, 2015. The Fenway Guide to LGBT Health. Module 4.
- Quallich SA, ed. Manual of Men’s Health: A Practical Guide for APRNs and PAs. New York, NY: Springer Publishing Company; 2018.
- Caceres BA, Streed CG, Corliss ML, et al. Assessing and addressing cardiovascular health in LGBTQ adults. Circulation. 2020;142(19):e321-e332.
- Goodman M, Adams N, Corneil T, et al. Size and distribution of transgender and gender nonconforming populations. Endocrinol Metab Clin N Am. 2019;48(2):303-321.
- Gorton RN, Berdahl CT. Improving the quality of emergency care for transgender patients. Ann Emerg Med. 2018;71(2):189-192.
- Jalali S, Sauer LM. Improving care for lesbian, gay, bisexual, and transgender patients in the emergency department. Ann Emerg Med. 2015;66(4):417-423.
- Pantalone DW, Haldeman DC, Martell CR. Health care issues facing lesbian, gay, bisexual, and transgender individuals. In: Sahler QJZ, Carr JE, Frank JB, Nunes JV, eds. The Behavioral Sciences and Health Care. 4th ed. Boston, MA: Hogrefe; 2018.
- Rosendale N, Goldman S, Ortiz GM, Haber LA. Acute clinical care for transgender patients. JAMA. 2018;178(11):1535-1543.
- Samenow CP, Salas-Ramirez KY. Sexuality and sexual disorders. In: Sahler OJZ, Carr JE, Franks JB, Nunes JV, eds. The Behavioral Sciences and Health Care. 4th ed. Boston, MA; Hogrefe; 2018.
- Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. 2018. Henry J Kaiser Family Foundation, Issue Brief.
- Centers for Disease Control and Prevention. Adolescent and School Health. Health disparities. Available at: https://www.cdc.gov/healthyyouth/disparities/index.htm. Accessed August 4, 2021.
- Gayles TA, Garofalo R. Exploring the health issues of LGBTQ adolescents. In: Schneider JS, Silenzio VMB, Erickson-Schroth L, eds. The GLMA Handbook on LGBT Health. 1st ed. Santa Barbara, CA: Praeger; 2019.
- Davidson A. Social Determinants of Health: A Comparative Approach. Ontario: Oxford UP; 2014.
- Lapinski J, Covas T, Perkins JM, et al. Best practices in transgender health: a clinician’s guide. Prim Care Clin Office Pract. 2018;45(4):687-703.
- Skidmore WC, Simone JM, Eskildsen MA, et al. The health of LGBT elders. In: Schneider JS, Silenzio VMB, Erickson-Schroth L, eds. The GLMA Handbook on LGBT Health. 1st ed. Santa Barbara, CA: Praeger; 2019.
- Johns MM, Lowry R, Haderxhanaj LT, et al. Trends in violence victimization and suicide risk by sexual identity among high school students – youth risk behavior survey, United States, 2015-2019. MMWR. 2020;69(1):19-27.
- Taylor AB, Chan A, Hall SL, et al. Being safe, being me 2019: results of the Canadian Trans and Non-binary Youth health Survey. Available at: https://apsc-saravyc.sites.olt.ubc.ca/files/2020/12/Being-Safe-Being-Me-2019_SARAVYC_ENG_1.2.pdf. Accessed August 4, 2021.
- Kann L, McManus T, Harris WA, et al. Youth Risk Behavior Surveillance – United States, 2017. MMWR: Surveillance Summaries. 2018;67(SS-8):1-114.
- Haas AP, Rodgers PL, Herman JL. Suicide Attempts among Transgender and Gender Non-Conforming Adults. Available at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/Trans-GNC-Suicide-Attempts-Jan-2014.pdf Accessed August 4, 2021.
- Headley M. Improving transgender patient care. patient safety & quality healthcare. Available at: https://www.psqh.com/analysis/improving-transgender-patient-care/ Accessed February 7, 2020.
- Bruessow D, Ng H, Wilson-Stronks A. When a welcoming health care environment matters most. In: Schneider JS, Silenzio VMB, Erickson-Schroth L, eds. The GLMA Handbook on LGBT Health. 1st ed. Santa Barbara, CA: Praeger; 2019.
- Centers for Disease Control and Prevention. A Guide to Taking a Sexual History. Available at: https://www.cdc.gov/std/treatment/sexualhistory.pdf. Accessed August 28, 2020.
- Cavanaugh T. Sexual Health History: Talking Sex with Gender Non-Conforming and Trans Patients. Available at: https://fenwayhealth.org/wp-content/uploads/Taking-a-Sexual-Health-History-Cavanaugh-1.pdf. Accessed August 4, 2021.
Read More LGTBQ JUCM Articles
- Update: The Civil Rights Act Applies To LGBTQ Employees; What Does This Mean For Urgent Care Centers?
- Making Your Urgent Care Center Welcoming For LGBTQ Patients

