Published on
Urgent message: Patients with recurrent symptoms should have an expanded history—including a genitourinary history in premenarchal girls.
Lavanya Boddu, MD, MBA
PRESENTATION
The patient is an 11-year-old female brought by her mother to urgent care, with a chief complaint of back pain. The patient was pushed down at school about 2 weeks ago playing ball, landed on her buttocks, and is complaining of back pain radiating to BL hips. She is still able to walk and carry out her regular activities with some pain. No fever, recent illnesses, abdominal pain, nausea, or vomiting. No dysuria, increased frequency or urgency, but at times she has to push on the pelvic area to urinate and have bowl movements.
- Past medical history: Neg
- Allergies: None
- Meds: None
- FH: Not significant
- Surgical history: None
Social
Lives with parents. Nothing has changed at home. She does not eat well, is not gaining weight, and misses school quite a bit, stays in bed with pain some days—more in the past year. Patient has been to her primary care for these issues many times in this last year; all tests were normal.
She also had GI referral, labs done—abdominal panel, gluten, urine—all of which were negative. She was referred to psychiatry secondary to recurrent abdominal pain in light of normal labs and missing school quite a bit.
Physical Exam
Vital signs normal except for tachycardia, with HR of 115.
- Appearance: Thin build. Uncomfortable, appears in pain, trying to rest her buttocks very lightly on the end of the examination table, frequently raising the buttocks up as if it hurts by putting pressure on hands
- CVS: Tachycardia, regular rhythm
- Lungs: Clear
- Abdominal exam: NT/ND, BS+. Soft, abdomen. No HSM. No BL CVA tenderness
- MS: Tenderness on L spine and BL paralumbar spinal areas, radiating to sacrum, BL hips and BL greater trochanteric area. No tenderness to palpation in the buttock region
- Gait: Widespread legs, hunched over gait, taking wide slow steps
- Neurologically: CN 2-12 intact
- Psych: A/O x 3. Tearful secondary to moderate pain in back
Labs
UA: neg
X-ray: L spine and Bl hips normal
Differential Diagnosis
- Trauma: Consider x-ray for fracture, though the time span of 2 weeks makes this less likely musculoskeletal pain. If imaging is negative, consider musculoskeletal pain for a strain or sprain; however, that does not explain patient’s out-of-proportion pain or the wide-based abnormal gait 2 weeks after her injury.
- UTI: UTI symptoms are not always typical. Some patients present with back pain, abdominal pain, dizziness, weakness, or even, in the elderly, hallucinations. Our patient complains of having to “push” on the abdomen to get urine out. She may have an epidural compression/cauda equina syndrome and should have bedside evaluation including strength, sensation, and straight leg raise testing.
- Constipation: It is very common in this age group and remains on the differential diagnosis, but more serious things need to be considered first.
- Abdominal pathology: Abdominal pathology like appendicitis must be considered; note that it can present with or without fever, abdominal pain, decreased appetite, nausea, vomiting. Thought gastroenteritis is common, our patient does not fit this diagnosis.
- GERD can present with early satiety, nausea, abdominal pain. H pylori infection would be unusual in this age group.
- Attention-seeking: Should be a diagnosis of exclusion; should be considered with questions about home and school situation and relation of abdominal pain to social stressors.
Summary
None of our patient’s symptoms are typical of the differential above. Her problem list includes:
- Low back pain
- Musculoskeletal Injury
- Abnormal gait
- Tachycardia
An MRI L spine is ordered to look for musculoskeletal or soft tissue abnormalities. The patient is sent home from the urgent care center with recommendation for OTC symptomatic analgesics.
Diagnosis
Hematocolpos
Imperforated hymen
Outcome
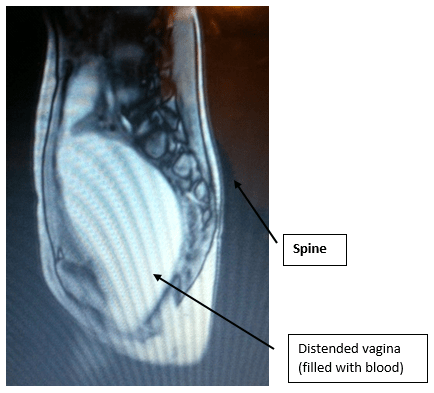
After MRI results showed distended vaginal area, tugging on the back in lumbosacral region, filled with blood/fluid (Figure 1), patient was referred to the ED, with OB/GYN consulted. Gynecological exam revealed normal labia but a small bluish mass (about 3 cm) pushing out through the vagina. Patient was transferred to the children’s hospital. Patient evaluated by pediatric GYN specialist, taken to surgery. Patient underwent hymenotomy and drained approximately 350 cc of old blood that had accumulated due to retrograde menses in the past year.
DISCUSSION
Diagnosis and Management of Congenital Anomalies of the Vagina
Embryology
The development of the female genital tract begins at 3 weeks of gestation and continues into the second trimester of pregnancy.1-3
Hymen
The vaginal lumen is separated from the urogenital sinus by the hymenal membrane. The hymen usually ruptures before birth due to degeneration of the central epithelial cells. However, a thin fold of mucous membrane persists around the vaginal introitus.3
Anomalies of the Hymen
The hymenal membrane consists of fibrous connective tissue attached to the vaginal wall. Hymenal anomalies are derived from incomplete degeneration of the central portion of the hymen.
Imperforate hymen
An imperforate hymen is one of the most common obstructive lesions of the female genital tract. At birth, infants may have a bulging introitus due to mucocolpos from vaginal secretions stimulated by maternal estradiol.1,4-6 If the diagnosis is not made in the newborn period and the hymen remains imperforate, the mucus will be reabsorbed and the child usually remains asymptomatic until menarche. At that time, the adolescent girl may present with a history of cyclic abdominal or pelvic pain and hematocolpos, which may give the hymenal membrane a bluish discoloration. Marked distension of the vagina may also result in back pain, pain with defecation, or difficulties with urination.7,8
Differential diagnosis includes imperforated hymen, agenesis of lower vagina, or a low transverse vaginal septum.
Treatment
Repair of the hymen can be performed at any age, but is ideal in the newborn, postpubertal, or premenarchal time periods.4,7,8
Incomplete hymenal fenestration
Incomplete fenestration of the hymenal opening (microperforate, septate, or cribriform) is often asymptomatic. Patients may seek gynecologic evaluation because of inability to insert tampons, douches, or vaginal creams, or because of difficulty with coitus.9 In addition, women with microperforate hymens may present with postmenstrual spotting or malodorous discharge due to partial obstruction and poor drainage. If menstrual products are not fully evacuated from the vagina, the retained blood may become infected and lead to tubo-ovarian abscesses.10
Treatment of microperforate, septate, and cribriform hymens involves resection of the excess hymenal tissue to create a functional hymenal ring, as described above. The excess hymenal tissue is excised with the use of electrocautery and interrupted sutures are placed to reapproximate the tissue.
Conclusion
- Include a menstrual history in adolescent girls, keeping in mind age of menarche may occur as early as 8 years.
- A GU exam may make the diagnosis.
- In menarche age-group girls with chronic recurrent abdominal pain, back pain, bowel problems, and bladder problems, consider imperforate hymen and hematocolpos.
Citation: Boddu L. An 11-year-old girl with back pain and chronic poor appetite. j Urgent Care Med. May 2019. Available at: https://www.jucm.com/an-11-year-old-girl-with-back-pain-and-chronic-poor-appetite/.
References
- The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, müllerian anomalies and intrauterine adhesions. Fertil Steril. 1988;49(6):944-955.
- Garcia RF. Z-plasty for correction of congenital HYPERLINK “file:///C:/contents/diagnosis-and-management-of-congenital-anomalies-of-the-vagina/abstract/6″transverseHYPERLINK “file:///C:/contents/diagnosis-and-management-of-congenital-anomalies-of-the-vagina/abstract/6” vaginal septum. Am J Obstet Gynecol. 1967;99(8):1164-1165.
- Jenny C, Kuhns ML, Arakawa. F. Hymens in newborn female infants. Pediatrics. 1987; 80(3):399-400.
- Saxena AK. Pediatric Imperforate hymen treatment & management. Medscape. Available at: https://emedicine.medscape.com/article/954252-treatment. Accessed April 10, 2019.
- MacLaughlin DT, Donahoe PK. Sex determination and differentiation. N Engl J Med. 2004;350(4):367-378.
- Berenson A, Hager A, Andrews S. Appearance of the hymen in newborns. Pediatrics. 1991; 87(4):458-465.
- Vainio S, Heikkilä M, Kispert A, et al. Female development in mammals is regulated by Wnt-4 signalling. Nature. 1999;397(6718):405-409.
- Biason-Lauber A, Konrad D, Navratil F, Schoenle EJ. A WNT4 mutation associated with Müllerian-duct regression and virilization in a 46,XX woman. N Engl J Med. 2004;351(8):792-798.
- Tardieu SC, Appelbaum H. Microperforate hymen and pyocolpos: a case report and review of the literature. J Pediatr Adolesc Gynecol. 2018;31(2):140-142.
- Evans TN, Poland ML, Boving RL. Vaginal malformations. Am J Obstet Gynecol. 1981;141(8):910-920.
Lavanya Boddu, MD, MBA serves as physician and medical director at Memorial Express Cares, Memorial Medical Center in Springfield, IL. The author has no relevant financial relationships with any commercial interests.
