Published on
Urgent message: Nontraumatic heel pain is a common presenting complaint in urgent care. Knowing how to accurately diagnose and develop a treatment plan is important, as the course is typically prolonged.
Katty Grand-Pierre, MD, CMSS, Frank Ida, BS, EMT-B, and Vincent D’Amore, MD, FACEP
INTRODUCTION
The heel can absorb 110% of body weight while a person is walking and 200% of body weight during running.1 While the most common cause is plantar fasciitis (PF), accounting for approximately 2 million office-based visits a year,2 the causes and treatments are often confusing. It’s a frustrating fact, for both patient and clinician, that there is no gold standard for treatment and the benefits of common treatments are questionable.
In assessing patients who present with heel pain, the urgent care provider must consider causes beyond PF. In this article, we present the “top 5” most likely culprits:
- Plantar fasciitis
- Achilles tendinopathy and bursitis
- Sever’s disease
- Tarsal tunnel syndrome
- Peroneal tendon pathology
HISTORY
Three key historical questions to ask all patients with heel pain to guide your thoughts:
- Does your heel pain start with the first few steps out of bed? (The most common cause of heel pain, PF, is specific for this complaint.)
- Does it hurt when you’re resting in bed or wake you up from sleep? (Musculoskeletal pain that is occurring at rest is concerning for fracture, osteomyelitis or malignancy. History including duration of symptoms and other associated complaints will direct further workup.)
- Where in your heel does it hurt? (The specific location of the pain and tenderness will often guide the clinician to the correct diagnosis. For example, tenderness at the point of insertion of the Achilles tendon (posterior heel) is specific for pathology at that site and strongly rules out PF as the cause.)
EXAM
General
As with all patients, examination should include having the patient remove shoes and socks of both feet to check for symmetry as well as obvious signs of infection and inflammation (such as redness or swelling). Additionally, neurovascular status must be assessed and documented, and the joint “above” (knee and fibular head) and “below” (midfoot) the area of the patient’s complaint examined. The location of tenderness will guide the clinician to the correct cause of pain:
- Inner medial section of heel surface: Most commonly, the tenderness will be present at the inner medial section of the heel in addition to possible tenderness along the sole of foot. This is consistent with a diagnosis of PF. If the clinician dorsiflexes the toes it will put tension on the plantar fascia and increase the pain of PF.
- Posterior aspect of heel: The “back” of the heel is where the Achilles (calcaneal) tendon inserts, as well as the location of the retrocalcaneal bursa. Inflammation and injury to these structures will manifest here. In children with heel pain, the most common cause is calcaneal apophysitis (Sever’s disease), an inflammation of the growth plate of the calcaneus.
- Bottom of heel: Tenderness to the middle of the heel pad implies an injury of the heel pad, such a contusion of the heel.
- Medial superior aspect of heel (posterior to medial malleolus): The tibial nerve and flexor tendons pass through the tarsal tunnel, a groove along the inner medial calcaneal bone. In cases of prior injury to the foot, bone spurs or fragments can cause pressure on the tibial nerve. This can result in Tarsal tunnel syndrome.
- Lateral superior aspect of the heel (posterior to the lateral malleolus): Posterior to the lateral malleolus are the tendons of the peroneus longus and brevis. Injuries consisting of both acute (tendinitis) and chronic (tendinosis) can occur.
HEEL PAIN CULPRIT #1: PLANTAR FASCIITIS
General
Thankfully, symptoms of this most common heel condition typically present classically. Upon sleeping or sitting for a prolonged period of time, a patient will have a painless heel suddenly and exquisitely hurt on the medial aspect of that heel upon ambulating the first few steps. This will somewhat resolve upon ambulating but return after periods of rest. The pain will lessen throughout the day with activity but increase toward the end of the day, depending on the amount of weight the foot has borne.
Whereas the diagnosis of PF is straightforward, the causes are multifactorial, and treatments confusing.
Anatomy and Presumed Causes
The plantar fascia is an aponeurosis of flattened tendons consisting of poorly vascularized connective tissue (type 1 collagen fibers) from the medial posterior calcaneus to the proximal phalanxes.
Patients tend to have multiple concurrent factors, including anatomical and functional.
Functional causes of PF relate to problems that occur with modern life, such as sitting too long at both our careers and leisure. Accordingly, we develop tight hamstrings, calves, and iliopsoas muscles, causing positional changes in our trunk and lower extremities and resulting in foot pronation which subsequently increases stress on the plantar fascia.
It is easy to see how a 30-minute workout of jumping rope or running on a heavier-than-designed body can cause an injury to the plantar fascia.
Etiology—overuse
Tension and trauma that are too much and/or too sudden and that overwhelm the body’s ability to adapt will cause injury of soft tissues and possibly bone. Running or jumping can cause micro tears at the insertion of the plantar fascia to the heel and cause pain.
A stress fracture of the calcaneus must also be considered if there is an acute significant overuse history, as this diagnosis can present in a similar fashion; consider MRI or bone scan with a concerning history.3
History and Physical
The classic patient with acute PF is a middle-aged, overweight, flat (pronated) footed patient who has recently been exercising more intensely than usual by a running and/or ballistic (bouncing) mechanism or has a career that forces them to stay on their feet for a large portion of the day. Pain follows the classic pattern of being worse on initial ambulation after having been off the foot (such as upon awakening after sleep), no pain while at rest, and tenderness to palpation of the medial inferior portion of the heel with toe dorsiflexion.
Diagnosis
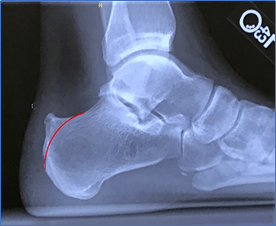
Diagnosis is often made clinically if no concerning history or physical factors exist. Plain x-rays are not necessary to diagnose PF although there are suggestive signs that can be seen on plain x-ray.
- Thickness of the plantar fascia (on lateral films) over 5 mm within 5 mm of the calcaneus is a reliable measure of pathological thickening.
- The triangular-shaped fat pad seen at the calcaneal origin of the plantar fascia may become distorted or absent in those with PF.
- Finally, there may be cortical changes at the plantar fascia attachment site.
Note that bone spurs are not specific for PF and are often seen in asymptomatic patients.4 MRI findings include plantar fascia thickening, edema, and fat pad irregularities below the plantar fascia.
Treatments
Acute
Acute (within the first 6 weeks) treatments commonly prescribed, especially for an acute injury or pain, are rest, ice to the area, stretches, and possibly a short course of NSAIDs.
While a common course of practice adopted by many clinicians is to treat a painful musculoskeletal condition with anti-inflammatory medicines, there have not been strong data to support their use. A randomized, prospective, placebo-controlled study found no difference between celecoxib and placebo at 1, 2, or 6 months.5 Accordingly, the American College of Foot and Ankle Surgeons (ACFAS) does not recommend the routine use of NSAIDs in treating PF.6
Strengthening of intrinsic foot muscles and stretching of the plantar fascia and tight muscle groups such as calves, hamstrings and hip flexors should be encouraged. Specifically stretching the PF with a cold bottle rolled along sole of foot is an often-suggested treatment as it stretches the plantar fascia itself, applies the anti-inflammatory properties of ice, and may “break up” scar tissue.
Therapeutic taping of the foot decreases foot pronation and transfer force to the lateral aspect of foot while ambulating. The tape is often worn for 2–5 days and can be applied by the patient at home or by a physical therapist.
Orthotics and foot splints
Initial treatment often includes a foot orthotic, as an orthotic minimizes the stress placed on the plantar fascia with ambulation and often decreases pain by reducing foot pronation despite not addressing the underlying causes, such as tight calves. While some clinicians may suggest expensive custom orthotics, store-bought orthotics (Figure 1) are found to be as helpful as custom orthotics. It is a reasonable initial treatment but should not be the only treatment.
Padded foot splints, which dorsiflex the ankle and stretch the calves, are also of some help and are often purchased over the counter but often their lack of comfort, they are generally worn while sleeping, limits their use.7
Figure 1.

Physical therapy
Anatomical changes of muscle relationships that result in increased stress on the plantar fascia and weakening of supporting intrinsic muscle strength of the foot, as is often the case, must be addressed.
Muscle mobilization therapy
Forcefully rubbing the muscles of the calves and heel of the foot at the fascia insertion and sole by hand and/or with hard tools to induce a microtrauma and “break up” scar tissue is a common mobilization therapy. The Graston technique is a patented example of this type of treatment.
Local steroid injection
Although no definitive consensus as to when, or exactly how much and which steroid should be used, at some point if initial treatments do not help, referral for local corticosteroid injection should be considered. There are multiple approaches that may, or may not, include sonographic guidance, which theoretically will decrease the likelihood of puncturing the plantar fascia with the needle. There is often short-term benefit, which has been shown to decrease one month after injection when compared to placebo.8 There is no definitive consensus as to how many steroid injections can be given safely.
Multiple injections are given judiciously as they may predispose to heel pad atrophy and/or PF rupture.
These “conservative” options are standard treatment and usually effective in treating the condition effectively in 90% of patients.
Extracorporeal shock wave therapy
The presumed mechanism for this minimally invasive, well-tolerated treatment is that the local shock waves will disrupt scar tissue and induce revascularization and thus enhance intrinsic healing. There are currently no definitive treatment protocols which may influence the reported results of this treatment which has shown a short term (3–6 months) improvement over placebo and suggested benefit over placebo for up to a year.9
Surgery
Conservative treatments are effective in 90% of patients, making surgery unusual.
HEEL PAIN CULPRIT #2: ACHILLES (CALCANEAL) TENDINOPATHY AND BURSITIS
General
Pain at the back of the heel is commonly the result of pathology to the Achilles tendon at the insertion to the calcaneus. Injury at the insertion site is termed enthesopathy. Additionally, bursae exist at the insertion site of the calcaneus that can also become inflamed. The gastrocnemius and soleus muscle together form the calcaneal, or Achilles, tendon. That, as well as the peroneus longus and brevis, allows for plantar flexion of the ankle.
Although not technically the heel, it is imperative to consider and rule out calcaneal tendon rupture, as this may require surgical treatment.
Injury as well as rupture of the tendon tend to occur at an area that has less blood flow to the tendon, roughly 2─6 cm proximal to the insertion at the calcaneus. As with other tendon pathologies, it is presumed this area may have more prior micro injuries that have not healed, resulting in abnormal fibroblastic growth that is vulnerable to acute tear from a shearing stress on activity.
This injury is more common among those who regularly forcefully flex their calves, such as runners and competitive athletes. Age is also a factor, especially as people continue to compete longer.
Historically, the patient will present with an acute pain upon forceful plantar flexion, unlike a sprain, a common incorrect diagnosis, which occurs with trauma. Physical exam for the integrity of the tendon is done by performing a Thompson’s test. The patient lies prone, and squeezing of the calf muscle elicits plantar flexion. This test has been found to be very accurate in diagnosing rupture with a sensitivity and specificity of 96% and 93% respectively.10
Management
All ruptures or potential ruptures should be referred to orthopedic surgery for further testing, treatment, and possible surgical repair (although there is no definitive study demonstrating the superiority of surgical to nonsurgical treatment).
Nonsurgical treatments also vary specifically but attempt to maintain contact between both ends of the injured tendon.
Splinting the patient in plantar flexion will help maintain contact. Weightbearing status will change as the injury heals “when ankle mobility allows it.”11
Assuming that tendon rupture has been ruled out, the clinician can focus on the area in question.
Enthesopathy, or injury, at the posterior section of the calcaneus is the specific location of pain and discomfort felt by patients. The mechanism commonly is a direct pulling of tendon fibers from the bony periosteum. This results in an inflammatory reaction acutely.
As can be expected, those who endure more forceful contractions and tension at this anatomical site are prone to more injuries. Runners, especially if competitive, male, and older, are prone to this entity.
Occasionally an exostosis, or bony outgrowth, of the posterosuperior of the calcaneus will occur. Currently this outgrowth, Haglund’s deformity, is felt to be due to chronic high stress of the calcaneal tendon. It is more common in women and is termed a “pump bump,” as certain shoes will repeatedly cause pressure to the area.
Located at the insertion site both superior and inferior to the tendon are two calcaneal bursa that can also become inflamed by the same mechanisms.
History and Physical
Patients will present with pain and tenderness at the back of the heel. Often it will be the result of increased activity overwhelming the body’s ability to repair itself, as is the case of many acute presentations of heel pain. Furthermore, patient’s will also be older and active, as is the case with other causes of heel pain as well.
Physical exam will reveal tenderness at the posterior heel. There may be signs of inflammation, such as redness and swelling of the site.
It is difficult to definitively differentiate the specific source of pain. Insertional tenderness is usually greatest in the middle of the calcaneus while bursitis tenderness is usually just superior to the bone. Bursitis pain usually is not elicited by only palpating the tendon itself
Diagnosis
The diagnosis is typically clinical with both palpation at the insertion of the Achilles tendon and performing the Thompson test to rule out a tendon rupture as mentioned previously.
Radiological imaging has not been found to be very accurate in diagnosis of tendinopathy.
Ultrasound may help differentiate between bursae or tendon pathology and can see localized inflammation demonstrate fluid in inflamed bursae.
MRI can additionally show tears in the calcaneal tendon and evaluate specifically for stress fractures as well as infection.12
Treatment
A common course of treatment initiated to these patients is one of avoidance of likely precipitating factors. Additionally, ice to the area as well as a heel lift to decrease tension at the insertional site is often provided. Many will consider a short course of NSAIDs to help acutely.
If symptoms persist, patients are often sent to PT which will concentrate on strengthening both in concentric and eccentric fashion which is felt to normalize tendon function. Symptoms may be prolonged and it may be 3-12 months before full strength and function is restored.13
HEEL PAIN CULPRIT #3 (A SCHOOL-AGE PROBLEM): SEVER’S DISEASE
General
In children with heel pain, the most common cause is calcaneal apophysitis (Sever’s disease) an inflammation of the growth plate, or apophysis, of the calcaneus. It usually occurs in active grade school children.
The growth plate of the calcaneus starts to close around 8 years of age and by 14 years is usually fused. There is increased metabolic activity of the apophysis during periods of rapid growth which may make it more susceptible to injury.
It is felt that repetitive injury from activity causes micro trauma and pain to the area. Additionally, both the tibial tendon as well as the plantar fascia insert into the apophysis. Tight muscles may contribute to the pathology as well.
History and Physical
The pain is insidious at onset and worse with activity, especially running and jumping. This can be thought of as Osgood-Schlatter disease of the foot by mechanism, too much stress on a nonfused growth plate, which should resolve as the child ages.
An exam technique that can differentiate this from other causes of heel pathology is the squeeze test. Grasping both sides of the calcaneus avoids the potential anatomical causes of pain of PF as well as tendon pathology. Pain elicited is specific for calcaneal source of pain.
Diagnosis
X-rays are usually not indicated unless symptoms are prolonged or if concern of other pathology exists. MRI imaging can show inflammation within the apophysis as well as exclude other pathology such as stress fracture
Treatment
Treatment consists of rest, calf stretches and strengthening of eccentric calf contraction that will soften landing forces on heel, padding to the heel, ice to affected area and a short course of NSAIDs if pain is severe. NSAIDs should not be given before athletic event as they can mask pain and allow more micro trauma to occur.
HEEL PAIN CULPRIT #4: TARSAL TUNNEL SYNDROME
General
Posterior to the medial malleolus is the tarsal tunnel, which encompasses multiple flexor tendons as well as the posterior tibial artery and nerve that pass through this tunnel bordered by bone on the inside and the flexor retinaculum on the outside. Increased pressure in this canal, often from anatomical causes, will cause pressure on the nerve. Commonly, prior injuries that result in bony fragments or overgrowth, scar tissue, nerve ganglion, etc. can cause this uncommon peripheral neuropathic syndrome.
History and Physical
Patients complain of pain along the nerve path from the inner heel to the sole of the foot. Additionally, a patient can feel tingling and burning “shooting” along the inner sole of the foot. In more pronounced cases, a Tinel’s sign will be present on tapping of the tibial nerve posterior to the malleolus. Often there will have been a prior injury to the talus or medial malleolus that will result in scar formation, bone spurs or cartilage fragments compressing the anatomical canal.
Diagnosis
History of pain posterior to the medial malleolus radiating to the inner sole of the foot is suggestive of this entity.
On physical exam, two tests are helpful:
- The Tinel test, which consists of tapping the nerve to elicit symptoms, is somewhat helpful as sensitivity ranges from 25%-75% and specificity 70%-90%.
- The dorsiflexion-eversion test stretches the canal and possibly compress the nerve. It is performed by passive dorsiflexion and eversion of the ankle as much as comfortably tolerated for 10 seconds. This test is positive in 82% of those patients with tarsal tunnel syndrome.14
Radiologic imaging is not typically necessary with short duration of symptoms.
X-rays can evaluate for bony abnormalities. MRI can evaluate the tarsal tunnel itself to assess for space occupying lesions.
Treatment
As with any nerve compression injury, if left untreated irreversible nerve damage may result. While a short course of NSAIDs and rest is reasonable, referral for further diagnostic testing such as MRI and nerve conduction studies is suggested if symptoms persist. Surgery releasing the nerve may be necessary in severe cases. If the neurological complaints were bilateral, one would consider neuropathy as a cause, especially if the patient were diabetic.
HEEL PAIN CULPRIT #5: PERONEAL TENDON PATHOLOGY
General
Peroneal tendon pathology is an underappreciated condition of those with chronic lateral ankle pain. The peroneus longus and brevis run along the lateral portion of the lower leg. They help in stabilization of the ankle, as well as plantar flexion and eversion. A few centimeters proximal to the lateral malleolus they are surrounded by a sheath that courses posterior to the lateral malleolus to the lateral foot. The tendons are kept from subluxing at the lateral malleolus by the superficial peroneal retinaculum.
Pathology of this area is often of an overuse mechanism with injury to the tendon and/or the retinaculum.
Pain can be felt along the outer heel into the tendon insertions on the lateral aspect of the foot, medial cuneiform, and first metatarsal bone and base of the fifth metatarsal, respectively. This is often seen in athletes who run or are required to make sharp cutting movements while running. Lateral wear on the heel of their shoes may imply additional stress and stretching on those tendons.
An easy-to-make mistake is to simply diagnose a lateral ankle ligament sprain when in fact the ligaments, which are located inferior to the lateral malleolus, are not involved. As the treatment is different, a high index of suspicion should exist.
In one chart review, only 60% of those with peroneal disorders were correctly diagnosed on initial examination.15
History and Physical
Patients will often complain of post-activity lateral ankle pain that resolves with rest. Additionally, and specifically, they may complain of a “popping” or slipping feeling in their ankle. That complaint alone may cause an alert clinician to refer to specialty care.
On physical exam, swelling and thickening of the tendons may be appreciated.
Dorsiflexion and eversion of the ankle may worsen symptoms.
Diagnosis
If a fracture is expected, radiograph imaging needs to be performed; however, that will not show soft tissue injuries.
Ultrasound has emerged as a quick and accurate testing tool for peroneal tendon abnormalities. Tendon pathology is evident if one sees thickening, hypoechoic (darker) swelling, and damage to the tendon fibers. Additionally, abnormal tendon movement may be visible if the retinaculum is damaged. The ability to do contralateral ankle comparison and perform dynamic testing differentiates it from MRI and is commonly performed.
One study using operative results as the gold standard stated ultrasound had a sensitivity and specificity of 90% and 94%, respectively, while MRI only had a sensitivity of 23% although a 100% specificity and accuracy of 66%.16
However, MRI still continues to be an accurate imaging modality as it can “see” tendon pathology (as well as osteochondral lesions, if present) not as easily seen on ultrasound.
Treatment
Acute injuries are often treated as is expected with rest, ice, and immobilization. When the peroneal tendons are acutely injured, many will include a period of non─weight-bearing, often in a walking boot; this is not the common treatment for the misdiagnosis of ankle sprain the patients often are given.
If the injury or pain is significant for a severely torn or stretched tendon, or instability from a retinaculum tear, surgery is recommended to tighten, repair, and stabilize the ankle.
CLINICAL PEARLS
- Many diagnoses are clinical and can be made at the bedside in the urgent care office.
- For many acute injuries, a conservative approach of rest, ice, and consideration of a short course of NSAIDs, if there are no contraindications, is a reasonable approach for many of the most common diagnoses. An additional consideration of peroneal tendon injury should exist for all “common” ankle sprains as the treatment is more conservative: a walking boot over the usual weight-bearing as tolerated
- Clinicians should have a low threshold to send patients to physical therapy.
- For patients with pain over 3-6 months, consider specialist referral for definitive diagnosis and consideration of steroid injections and possibly “restorative therapy” treatments.
Citation: Grandpierre KE, Ida F, D’Amore V. Top 5 causes–and controversial conducts– of heal pain in urgent care. J Urgent Care Med. May 2019. Available at: https://www.jucm.com/top-5-common-causes-and-controversial-conducts-of-heel-pain-in-urgent-care/.
References
- Jozsa LG, Kannus P. Human tendon: anatomy, physiology and pathology. Champaign, IL; Human Kinetics Publisher 1997.
- Tu P, Bytomski JR. Diagnosis of heel pain. Am Fam Physician. 2011;84(8):909-916.
- Mayer SW, Joyner PW, Almekinders LC, Parekth SG. Stress fractures of the foot and ankle in athletes. Sports Health. 2014;6(6):481–491.
- Draghi F, Gitto S, Bortolotto C, et al. Imaging of plantar fascia disorders: findings on plain radiography, ultrasound and magnetic resonance imaging. Insights Imaging. 2017;8(1):69–78. [Epub December 12, 2016.]
- Donley BG, Moore T, Sferra J, et al. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007;28(1):20–23.
- Schneider HP, Baca JM, Carpenber BB, et al. American College of Foot and Ankle Surgeons Clinical Consensus Statement: Diagnosis and treatment of Adult Acquired Infracalcaneal Heel Pain. J Foot Ankle Surg. 2018;57(2):370-381.
- Lewis RD, Wright P, McCarthy LH. Orthotics compared to conventional therapy and other non-surgical treatments for plantar fasciitis. J Okla State Med Assoc. 2015108(12): 596–598.
- Crawford F, Atkins D, Young P, Edwards J. Steroid injection for heel pain: evidence of short-term effectiveness. A randomized controlled trial. Rheumatology (Oxford). 1999;38(10):974-977.
- Aqil A, Siddiqui MR, Solan M, et al. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Clin Orthop Relat Res. 2013;471(11):3645–3652.
- Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998;26(2):266-270.
- Gulati V, Jaggard M, Al-Nammari SS, et al. Management of Achilles tendon injury: a current concepts systematic review. World J Orthop. 2015;18:6(4):380–386.
12. Shah MT, Wong BS. Clinics in diagnostic imaging (170). Singapore Med J. 2016;57(9):517–522.
- Kedia M, Williams M, Jain L, et al. The effects of conventional physical therapy and eccentric strengthening for insertional Achilles tendinopathy. Int J Sports Phys Ther. 2014;9(4):488-497.
- Kiel J, Kaiser K. Tarsal tunnel syndrome. StatPerls (Internet). Available at: https://www.ncbi.nlm.nih.gov/books/NBK513273/. Accessed April 15, 2019.
- Dombek MF, Lamm BM, Saltrick K, et al. Peroneal tendon tears: a retrospective review. J Foot Ankle Surg.2003;42(5):250-258.
- Rockett MS, Waitches G, Sudakoff G, Brage M. Use of ultrasonography versus magnetic resonance imaging for tendon abnormalities around the ankle. Foot Ankle Int. 1998;19(6):604-612.
Katty Grand-Pierre, MD, CMSS, is a physician with CityMD Urgent Care. Frank Ida, BS, EMT-B is senior medical scribe at CityMD Urgent Care. Vincent D’Amore, MD, FACEP is executive vice president of CityMD. The authors have no relevant financial relationships with any commercial interests.
