Published on
Download the article PDF: Blocking The Pain Nerve Block In The Treatment Of Headache In Urgent Care
Urgent Message: Although greater occipital nerve block has demonstrated positive effectiveness and few risks as a treatment for acute headache, it is not commonly used. With more familiarity, urgent care clinicians may consider it a useful treatment modality.
Elizabeth Reynolds, PA-C, MS
Key Words: Migraine, Headaches, Nerve Block
Abstract
Headaches are a common presentation in urgent care clinics. Various medication options are available but can sometimes be limited for use due to allergies, side effects, poor prior treatment response, and contraindications. Multiple studies have shown high success and low risk with a greater occipital nerve block (GONB) for headache, however, this intervention is not commonly used. This article reviews the anatomy, pathophysiology, and recommended techniques for GONB in the treatment of acute headaches.
Introduction
Headaches are one of the most prevalent and disabling neurological complaints globally.[1],[2] Patients often have tried home treatments and interventions before seeking medical attention for an acute headache. Clinicians can use first-line treatments to address migraine headaches, such as metoclopramide, prochlorperazine, or sumatriptan.[3] However, the literature suggests that first-line therapies do not provide sufficient relief for more than 25% of patients.3,[4],[5]
Opioids and barbiturates are more commonly prescribed in the emergency department for headaches than non-opioid treatments, even though guidelines recommend not treating headaches with opioids.[6],[7] As such, clinicians can consider alternative treatment options, such as GONB, which has shown notable success in several studies.3,4,5,[8],[9],[10] A GONB is an injection of local anesthetic in the region of the greater occipital nerve on the back of the occipital scalp region.
Greater Occipital Nerve Block
The GONB remains an underutilized treatment option for acute headaches, likely due to a lack of knowledge or experience about the procedure.1,[11] The GONB has consistently shown a clinically significant reduction in pain in more than 80% of patients.7,[12] Specifically, patients were noted to experience more than 80% significant pain relief within 30 to 60 minutes after the procedure.5,8,[13],[14] A separate study showed substantial pain improvement in more than 58% of patients within 30-60 minutes.14 Several randomized controlled trials have demonstrated that GONB is statistically significant in reducing headache pain within 20 minutes with improvements in headache severity lasting up to 24 weeks.11,[15],[16],[17],[18] Studies have also shown a decrease in headache recurrence and frequency, which lasts significantly longer than the effect of local anesthesia.8,9,11,[19]
Another randomized controlled trial did not yield significant findings for prolonged headache relief; however, compared to the placebo, participants experienced a reduction in headache frequency and intensity.5,15 A number of patients experienced a decrease in migraine pain from baseline after multiple GONB treatments.14 Additionally, GONB has also been highly successful in treating pediatric headaches, in which other treatment options may be limited. It has reduced headache intensity by more than 50% in pediatric patients with headaches, with minimal to no side effects.16,[20],[21]
GONB can be considered a simple and cost-effective treatment modality for headaches in clinical settings.8,13 The procedure is minimally invasive and does not require specialized equipment, advanced training, or a post-procedure observation period. Patients can often return to their everyday lives immediately, experiencing reduced pain and no restrictions on driving or activity.18
Potential concerns specifically for urgent care (UC) clinicians may include unfamiliarity with the procedure, optimizing the location of the injection, patient tolerance, or concerns about potential side effects. However, side effects such as local pain, tenderness, or bruising at the injection site are uncommon and mild if they occur. Side effects from GONB using local anesthetics were no different than those of a saline placebo used among a number of studies.11 Additionally, there were no long-term adverse effects from GONB using local anesthetics as noted among studies.11,14
Interestingly, minimal guidelines exist for GONB, despite its use in treating primary headaches dating back to the 1930s.2,8,9,[22]
In previous studies, the choice of local anesthetic drug, drug dose, volume, pattern, addition of corticosteroids, and frequency of administration have been variable, making it difficult to establish specific recommendations.8 More studies have recently been conducted, however, and others are ongoing to further evaluate the evidence.[23],[24],[25],[26]
The American Headache Society (AHS) last published guidelines in 2016, which did not discuss nerve blocks.4 Subsequent publications by the AHS have found nerve blocks strongly efficacious,3,8 and the AHS is developing new guidelines that are anticipated to include recommendations regarding nerve blocks.4
Pathophysiology Review
Patients presenting with headaches may often have a trigger point caused by compression of a cranial nerve.[27] Abnormal stimulation or triggering of the trigeminal nerve, which sends nociceptive signals to the trigeminocervical complex (TCC), can sometimes cause headaches. The greater occipital nerve is a convenient conduit to the trigeminal and TCC nerves.[28]
The TCC is one of the neural processing areas in the brainstem, responsible for processing pain signals from the head and neck.11 The intertwined nature of the trigeminal, occipital, and cervical nerves often results in a cause-and-effect cycle that further stimulates abnormal nociceptive signals to the trigeminocervical complex. The pain signals may trigger an inflammatory response around the trigeminocervical complex and brain arteries.[29]
Functional magnetic resonance imaging studies have shown that GONB reduces nociceptive signals, reducing pain transmission from the trigeminocervical complex to the brainstem.29,[30],[31] This reduction of signals causes a decrease in neuroinflammatory processes, quickly stopping the pain and the underlying central sensitization.16,30,31,[32] The nerve block is thought to break the cycle of pain, allowing the nervous system to return to its normal level of neural sensitivity. The prolonged effect of headache pain relief after a nerve block is not well understood or studied but is thought to be due to the interruption of pain modulation.8,14
Indications
GONB is proven effective in the treatment of cervicogenic, acute, and chronic migraine, as well as tension, post-dural puncture, occipital neuralgia, and cluster headaches.10,13 GONB can also benefit both pediatric and adult headache patients who may have contraindications to other treatment options, such as patients of older age, patients with vascular disease, pregnancy,[33]patients with kidney disease, or medication allergies.13
It is important to note that studies have not found GONB to be an effective intervention for medication overuse headaches and chronic tension headaches.17
Use of Corticosteroids In Nerve Block
GONB can be administered with only a local anesthetic or with a combination of local anesthetic and steroids.8 The results of studies for headaches with the addition of corticosteroid use in GONBs have been conflicting, with some studies showing it may help prolong the pain nerve signal-blocking effect.1,9 However, limited evidence exists on the effect of adding corticosteroids for varying headache types, with equivocal results.13,15,17,[34] Evidence is strongest to support the treatment of cluster headaches with the addition of corticosteroids.1,9,13,16,17,[35]
GONB Technique
Equipment
- Gloves
- Alcohol pad, povidone-iodine, or chlorhexidine for skin prep
- 5 mL syringe with 25-, 27-, or 30-gauge needle (½-1 inch length) for injection8
- Topical spray anesthetic or topical anesthetic cream, if available and desired
- 2×2 gauze to apply pressure after injection
- Local anesthetic (can combine lidocaine and bupivacaine 50/50 mix or use individually), total volume should be about 4 mL
- Lidocaine 1% without epinephrine
- Bupivacaine 0.5% (avoid in pregnancy)
- If steroids are used, see Table 1 for steroid options and dosing
| Medication | Dose ranges (total volume 1.5-4 mL per nerve) | Recommended average dose | Half-life (biological) | Notes |
| Lidocaine 1-2% | 1-2 mL | 1 mL if used with steroids 2 mL if only local anesthesia | 1.5-2 hours | Local anesthetics can be used in combination. Use 1:1 or 1:3 ratio of lidocaine:bupivicaine. |
| Bupivicaine (0.25-0.5%) | 1-2 mL | 1 mL if used with steroids 2 mL if only local anesthesia | 2.7 hours | |
| Dexamethasone 2 mg/mL | 4 mg | 4 mg (2 mL) | 36-54 hours | Can pass through the brain-blood barrier. Non-particulate corticosteroid. |
| Methylprednisolone (40 mg/mL) | 20-160 mg | 40 mg (2 mL) | 18-36 hours | Particulate corticosteroid. |
| Triamcinolone (40 mg/mL) | 5-40 mg | 18-36 hours | Particulate corticosteroid. | |
| Betamethasone (4-6 mg/mL) | 18 mg | 36-54 hours | Particulate corticosteroid. |
| Condition | Recommendation |
| • Open skull defect craniotomy • Burr holes • Arnold-Chiari malformation •Shunts • Surgical/nerve stimulators • Inability to sit or lie still | Contraindicated |
| Anticoagulation | • Individualized for risk vs benefit. • Aspirate before injection to ensure no vasculature involvement. Direct pressure after injection for 5-10 minutes. |
| Pregnancy | • Use lidocaine only: pregnancy class B. • Bupivacaine and mepivacaine are contraindicated in pregnancy. • Do not use steroids due to the potential risk for fetal effects. |
| Pain with injection | • Use a topical anesthetic cream or spray. • Avoid moving the needle once inserted. • Use a finer gauge needle. |
| Dizziness, lightheadedness, syncope | • Consider a reclined or decubitus position for injection. |
| Allergy to lidocaine | • Use corticosteroids only. |
Set-up
GONB can be performed on the side of the head or on the bilateral greater occipital nerve areas.
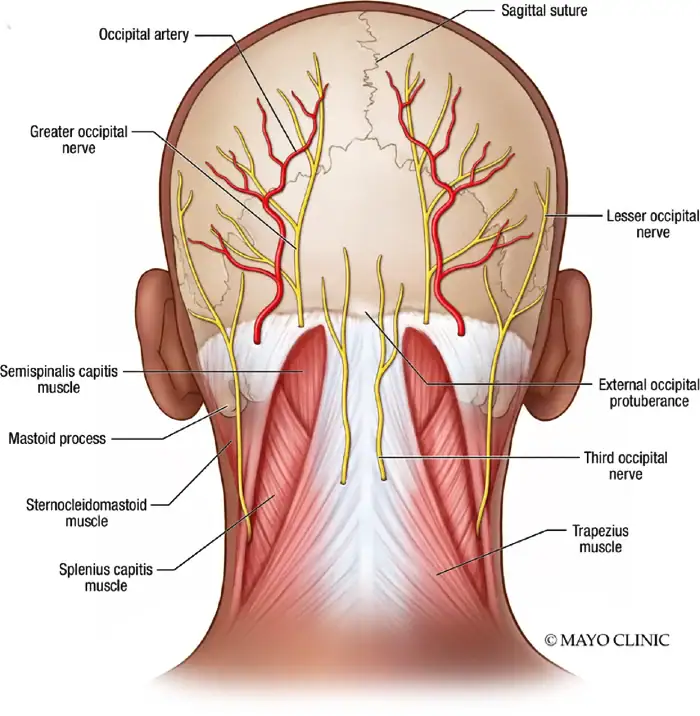
Credit: Mayo Clinic (Permission obtained)
- Evaluate for risk or contraindications (Table 2)
- Obtain informed consent from the patient. Include potential risks such as ineffective response, local pain, tenderness, or bruising at the injection site, in addition to accidental injection into an artery, infection, and other possible complications
- Position the patient upright in a chair or on the exam table, leaning forward with the head resting on a table or pillow. The patient can also lie supported in a prone position or lateral decubitus with the back of the head easily accessible to the clinician. Studies indicate no significant difference in position on the effect of treatment but find that a sitting position may slightly improve outcomes.[36] Some patients may benefit from a supported position or can lie down after the procedure for monitoring if they are prone to vasovagal reactions.
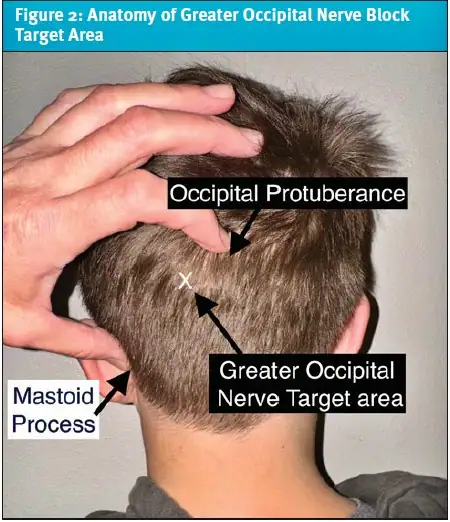
- Identify the area of the greater occipital nerve (GON), which can be found by palpating the occipital protuberance and the mastoid process (Figure 1). Draw an imaginary line between the 2 areas, and the GON can be found about one-third of the way down from the occipital protuberance along this line (Figure 2).[37] The GON is often about 2 cm lateral and 1.5-2 cm below the occipital protuberance.2,37 If needed, this area can be marked with a skin marker for visual reference. The occipital artery can sometimes be palpated lateral to this area.32
- Some clinicians also will palpate to find areas of tenderness, which can also indicate the region of the GON. The nerve block can still be done even if the area is not tender to palpation. Focal pain does not predict a better response to the nerve block.[38]
Procedure
- Once the area of GON has been identified, apply topical anesthetizing cream if using. Allow it to penetrate for 5-10 minutes, depending on the formulation’s specific instructions.39
- Prepare the area with a topical cleanser, such as an alcohol pad, chlorhexidine, or povidone-iodine wipe.
- If using a topical numbing spray, apply it to the area. Insert a needle perpendicular to the skin until it encounters firm resistance (periosteum) at approximately 3-4 mm.8 If there is no bone contact within 1 cm of needle insertion, redirect the needle slightly toward the top of the head.37
- Once bone contact is noted, withdraw the needle slightly, approximately 1 mm, and pull back on the plunger to ensure it is not in an artery. Then inject slowly in a fan-like distribution towards the areas of increased pain.7,8,37 There might be a burning sensation as the anesthetic is injected, which should subside in a few minutes or less.10
- There is variability in the path of the GON, so a fanning of the needle to cover a larger area or a higher volume of local anesthesia can increase the success of the GONB.7,8
- Remove the needle, apply pressure to the area, and gently massage the anesthetic to distribute it evenly throughout the nerve area.20
- There will often be subsequent numbness in the distribution of the greater occipital nerve with a successful block.32
Post-Procedure Monitoring
After the procedure, monitoring is case-specific. Many patients will note rapid pain improvement. Most patients will not require post-procedural monitoring, however, it can be helpful to assess the response to determine the presence of side effects. Numbness may be noted in the area of the nerve dermatome and can indicate a successful nerve block. The lack of dermatomal numbness does not necessarily indicate a failed block.10,32 Side effects from the injection are uncommon, but patients can be cautioned about the rare potential for dizziness, syncope, worsening headache, nerve or arterial injury, hematoma, pain, swelling, or redness at the injection location.8,[39]
Patients often experience a long-term reduction in pain beyond the duration of anesthetics and corticosteroids, as well as decreased frequency of headaches and need for rescue medications.11,17,26,39
Hypothetical Case Scenarios
Case 1
History: An otherwise healthy 32-year-old female with a history of migraine headaches presented to urgent care for a left-sided migraine headache for 24 hours. She had taken zolmitriptan and ibuprofen 4 hours earlier without relief. She had no new or worrisome symptoms different from prior migraines. She reported accompanying symptoms of photophobia, nausea, phonophobia, and dizziness. Her headache pain scale was 5/10.
Her past medical history is notable in that she has never had GONB. Her usual migraines last about 12 hours and are often improved with sleep. She has been seen in the clinic a few times prior for migraine headache treatment.
Physical exam: Her vital signs were as follows: blood pressure, 136/72 mmHg; pulse, 78 beats per minute; respiratory rate, 18 breaths per minute; temperature, 97.2°F/36.2°C; and SpO2, 99% on room air.
She was sitting in a dark room, looking uncomfortable. She had some tenderness along the left posterior scalp and occipital insertion. She did not have any temporal artery tenderness or temporomandibular joint pain. No scalp swelling or abnormality was present. Her pupils were equal and reactive to light. Fundoscopic examination showed a normal appearance of the retina, without papilledema. No neck stiffness or midline cervical neck pain was present. Cranial nerves 2-12 were intact, and bilateral upper and lower deep tendon reflexes were normal. She had no notable motor or neurological deficits on the exam. She demonstrated normal gait and movement.
Treatment: A left-sided GONB using 2 mL of 1% lidocaine and 2 mL of 0.5% bupivacaine was administered, with significant improvement in her pain within 15 minutes. She did not require further intervention.
Case 2
History: A 24-year-old female presented to urgent care with a history of episodic migraines, which progressed to daily headaches for the past 2 weeks. She is currently 6 weeks pregnant. Her headache was over the right occipital and temporal region, with tenderness noted in the affected area. She was experiencing nausea, vomiting, and photophobia. She had previously been on topiramate for migraine prophylaxis but discontinued use due to her current pregnancy. She did not exhibit any new symptoms from her typical migraine. Her pregnancy had not had any complications or concerns.
Physical exam: Her vital signs were: blood pressure of 118/68 mmHg; pulse of 82 beats per minute, respiratory rate of 16 breaths per minute, temperature was 98.4°F/36.8°C; and SpO2 was 100%. She was holding an emesis bag and appeared uncomfortable, holding her head. She had a normal physical exam with no temporal artery tenderness, no temporomandibular joint pain, and no scalp swelling or abnormality. Her pupils were equal and reactive to light. Fundoscopic examination showed a normal appearance of the retina without papilledema. There was no neck stiffness or midline cervical neck pain, however, she noted tenderness along the paracervical neck muscles. Cranial nerves 2-12 were intact, and bilateral upper and lower extremity deep tendon reflexes were normal. She had no notable motor or neurological deficits on the exam. She demonstrated normal gait and movement.
Treatment: After discussion of various treatment options, she was given a bilateral GONB using 4 mL of 1% lidocaine without epinephrine with successful relief of her pain within 30 minutes.
Case 3
History: A 58-year-old male with a history of cluster headaches presented to urgent care for an ongoing right-sided severe headache for the past hour. He had 2 prior cluster headache attacks over the past 3 days. His pain was over the right peri-cranial area, and he described stabbing pains. He is on verapamil for prophylaxis. Prior intracranial imaging has been normal.
Physical exam: His vital signs were: blood pressure of 146/88 mmHg; pulse of 98 beats per minute; respiratory rate of 22 breaths per minute, temperature of 98.2°F/36.7°C, and SpO2 of 97%. He was restless, pacing the room, and appeared very uncomfortable. He was noted to have conjunctival injection, eye watering, and right-sided nasal congestion. He was tender over the right peri-cranial and GON area.
Treatment: He was placed on high-flow oxygen therapy and received a right GONB with 1.5 mL of 1% lidocaine, 1.5 mL of 0.5% bupivacaine, and 1 mL of 40 mg/mL methylprednisolone. He had notable relief of his headache within 30 minutes and was discharged home in stable condition.
Takeaway Points
- The GONB is a simple and minimally invasive procedure for treating headaches with minimal side effects.
- Patients who cannot tolerate other therapies (or for whom different treatments are contraindicated) can often receive a nerve block.
- GONB has been proven through randomized controlled trials to reduce headaches within a short period with minimal systemic effects.
- Patients often experience a long-term reduction in pain beyond the duration of anesthetics and corticosteroids, as well as decreased frequency of headaches and need for rescue medications.
- Clinicians are encouraged to consider this technique as an effective treatment option for headaches in acute care settings.
Manuscript submitted December 10, 2024; accepted May 21, 2025.
References
- [1]. Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34. doi:10.1186/s10194-022-01402-2
- [2]. Hasırcı Bayır BR, Gürsoy G, Sayman C, et al. Greater occipital nerve block is an effective treatment method for primary headaches? Ağrı. 2022;34(1):47-53. doi:10.14744/agri.2021.32848.
- [3]. Kazi F, Manyapu M, Fakherddine M, Mekuria K, Friedman BW. Second‐line interventions for migraine in the emergency department: A narrative review. Headache J Head Face Pain. 2021;61(10):1467-1474. doi:10.1111/head.14239
- [4]. Robblee J, Zhao X (Rachel), Minen MT, et al. The 2023 protocol for update to acute treatment of adults with migraine in the emergency department: The American Headache Society evidence assessment of parenteral pharmacotherapies. Headache J Head Face Pain. 2024;64(7):869-872. doi:10.1111/head.14744
- [5]. Li W, Tang L. Influence of greater occipital nerve block on the relief of acute migraine: A meta-analysis. Medicine (Baltimore). 2024;103(42):e39955. doi:10.1097/MD.0000000000039955
- [6]. Ahmed ZA, Nacopoulos DA, John S, Papesh N, Levine D, Bamford CC. An Algorithm for Opioid and Barbiturate Reduction in the Acute Management of Headache in the Emergency Department. Headache J Head Face Pain. 2017;57(1):71-79. doi:10.1111/head.12961
- [7]. Vanterpool SG, Heidel RE, Rejoub LR, Rejoub LR. Targeting Occipital Headache Pain: Preliminary Data Supporting an Alternative Approach to Occipital Nerve Block. Clin J Pain. 2020;36(4):289-295. doi:10.1097/AJP.0000000000000802
- [8]. Stern JI, Chiang C, Kissoon NR, Robertson CE. Narrative review of peripheral nerve blocks for the management of headache. Headache J Head Face Pain. 2022;62(9):1077-1092. doi:10.1111/head.14385
- [9]. Blumenfeld A, Ashkenazi A, Napchan U, et al. Expert Consensus Recommendations for the Performance of Peripheral Nerve Blocks for Headaches – A Narrative Review. Headache J Head Face Pain. 2013;53(3):437-446. doi:10.1111/head.12053
- [10]. Fernandes L, Randall M, Idrovo L. Peripheral nerve blocks for headache disorders. Pract Neurol. 2021;21(1):30-35. doi:10.1136/practneurol-2020-002612
- [11]. Mustafa MS, bin Amin S, Kumar A, et al. Assessing the effectiveness of greater occipital nerve block in chronic migraine: a systematic review and meta-analysis. BMC Neurol. 2024;24(1). doi:10.1186/s12883-024-03834-6
- [12]. Ebied AM, Nguyen DT, Dang T. Evaluation of Occipital Nerve Blocks for Acute Pain Relief of Migraines. J Clin Pharmacol. 2020;60(3):378-383. doi:10.1002/jcph.1528
- [13]. Castillo-Álvarez F, Hernando de la Bárcena I, Marzo-Sola ME. Greater occipital nerve block in the treatment of headaches. Review of evidence. Med Clin (Barc). 2023;161(3):113-118. doi:10.1016/j.medcli.2023.04.001
- [14]. Allen SM, Mookadam F, Cha SS, Freeman JA, Starling AJ, Mookadam M. Greater Occipital Nerve Block for Acute Treatment of Migraine Headache: A Large Retrospective Cohort Study. J Am Board Fam Med. 2018;31(2):211-218. doi:10.3122/jabfm.2018.02.170188
- [15]. Velásquez-Rimachi V, Chachaima-Mar J, Cárdenas-Baltazar EC, et al. Greater occipital nerve block for chronic migraine patients: A meta-analysis. Acta Neurol Scand. 2022;146(2):101-114. doi:10.1111/ane.13634
- [16]. De Freitas Dias B, Robinson CL, Villar-Martinez MD, Ashina S, Goadsby PJ. Current and Novel Therapies for Cluster Headache: A Narrative Review. Pain Ther. 2025;14(1):1-19. doi:10.1007/s40122-024-00674-7
- [17]. Wahab S, Kataria S, Woolley P, et al. Literature Review: Pericranial Nerve Blocks for Chronic Migraines. Health Psychol Res. 2023;11:74259. doi:10.52965/001c.74259
- [18]. Arata WH, Midha RK, Varrassi G, et al. Occipital nerve block for headaches: a narrative review. J Oral Facial Pain Headache. 2024;38(2):1-10. doi:10.22514/jofph.2024.010
- [19]. Chowdhury D, Datta D, Mundra A. Role of Greater Occipital Nerve Block in Headache Disorders: A Narrative Review. Neurol India. 2021;69(Supplement):S228-S256. doi:10.4103/0028-3886.315993
- [20]. Esparham A, Boorigie M, Ablatt S, Connelly M, Bickel J. Improving Acute Treatment of Pediatric Primary Headache Disorders With a Novel Headache Treatment Center: Retrospective Review of Preliminary Outcomes. J Child Neurol. 2021;36(1):54-59.
- [21]. Hassan R, Gudiwala V, Dawn P, Jeynes L. Greater Occipital Nerve Block as an Effective Intervention for Medically Refractory Pediatric Migraine: A Retrospective Study. Cureus. Published online February 13, 2023. doi:10.7759/cureus.34930
- [22]. Go D, Gould M, Ganti L. History of the Nerve Block. Orthop Rev. 2024;16:125260. doi:10.52965/001c.125260
- [23]. Friedman B. A randomized, sham-controlled trial of greater occipital nerve block as second line therapy for ED patients with acute migraine. ClinicalTrials.gov. Accessed February 3, 2025. https://clinicaltrials.gov/ct2/show/NCT02665273
- [24]. Moazzam A. Efficacy of GONB in patients of migraine. ClinicalTrials.gov. Accessed February 3, 2025. https://clinicaltrials.gov/ct2/show/NCT05679765
- [25]. Merry S, Mayo Clinic. Efficacy of nerve blocks for episodic migraine. ClinicalTrials.gov. 2024;identifier: NCT05734625. Accessed February 3, 2025. https://clinicaltrials.gov/cts/show/NCT02665273
- [26]. Children’s Hospital of Philadelphia. Occipital blocks for acute migraine. ClinicalTrials.gov. 2024;identifier: NCT03526874. Accessed February 3, 2025. https://clinicaltrials.gov/cts/show/NCT03526874
- [27]. Evans AG, Joseph KS, Samouil MM, et al. Nerve blocks for occipital headaches: A systematic review and meta-analysis. J Anaesthesiol Clin Pharmacol. 2023;39(2):170-180. doi:10.4103/joacp.JOACP_62_21
- [28]. Shauly O, Gould DJ, Sahai-Srivastava S, Patel KM. Greater Occipital Nerve Block for the Treatment of Chronic Migraine Headaches: A Systematic Review and Meta-Analysis. Plast Reconstr Surg. 2019;144(4):943-952. doi:10.1097/PRS.0000000000006059
- [29]. Hoffmann J, Mehnert J, Koo EM, May A. Greater occipital nerve block modulates nociceptive signals within the trigeminocervical complex. J Neurol Neurosurg Psychiatry. 2021;92(12):1335-1340. doi:10.1136/jnnp-2021-326433
- [30]. Love SM, Hopkins BD, Migdal CW, Schuster NM. Occipital Headache Evaluation and Rates of Migraine Assessment, Diagnosis, and Treatment in Patients Receiving Greater Occipital Nerve Blocks in an Academic Pain Clinic. Pain Med. 2022;23(11):1851-1857.
- [31]. Alis C, Abbaszade H, Uygunoglu U, Kiziltan ME, Gunduz A. Sensorimotor gating in chronic migraine and its association with bilateral greater occipital nerve block. Pain Med. 2023;24(8):1001-1004. doi:10.1093/pm/pnad016
- [32]. Jankovic D, Peng P, eds. Regional Nerve Blocks in Anesthesia and Pain Therapy: Imaging-Guided and Traditional Techniques. Springer International Publishing; 2022. doi:10.1007/978-3-030-88727-8
- [33]. Hamilton KT, Robbins MS. Migraine Treatment in Pregnant Women Presenting to Acute Care: A Retrospective Observational Study. Headache J Head Face Pain. 2019;59(2):173-179. doi:10.1111/head.13434
- [34]. Kashyap PV, Chabri S. Steroids in Headache: A Comprehensive Review of Recent Research. Ann Neurosci. 2023;30(4):256-261. doi:10.1177/09727531231173286
- [35]. Benzon HT, Elmofty D, Shankar H, et al. Use of corticosteroids for adult chronic pain interventions: sympathetic and peripheral nerve blocks, trigger point injections – guidelines from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, the American Society of Interventional Pain Physicians, the International Pain and Spine Intervention Society, and the North American Spine Society. Reg Anesth Pain Med. Published online July 16, 2024:rapm-2024-105593. doi:10.1136/rapm-2024-105593
- [36]. Vanderpol J, Kennedy G, Ahmed F, Jonker L. Efficacy of greater occipital nerve block treatment for migraine and potential impact of patient positioning during procedure: Results of randomised controlled trial. Clin Neurol Neurosurg. 2024;239:108210. doi:10.1016/j.clineuro.2024.108210
- [37]. Ganti L. Atlas of Emergency Medicine Procedures. 2nd ed. Springer International Publishing AG; 2023.
- [38]. Schwarz A, Ziegeler C, Daneshkhah S, May A, Luedtke K. Predicting the outcome of the greater occipital nerve block – an observational study on migraine patients with and without musculoskeletal cervical impairment. Cephalalgia Int J Headache. 2021;41(1):78-89. doi:10.1177/0333102420954518
- [39]. Fernandes L, Khan N, Dobson J, Randall M, Idrovo L. Multiple Cranial Nerve Blocks as an Alternative Preventative Therapy for Chronic Migraine Headache J Head Face Pain. 2020;60(5):981-987. doi:10.1111/head.13792
Author Affiliation: Elizabeth Reynolds, PA-C, MS, A.T. Still University and Confluence Health, Moses Lake, Washington. Author has no relevant financial relationships with any ineligible companies.
Read More
- Postpartum Presentations: When Risk Arises After Delivery – Headache
- A 30-Year-Old Female with Headaches of Increasing Frequency
