Published on
Differential Diagnosis
- ST-elevation myocardial infarction (STEMI)
- Right bundle branch block (RBBB)
- Trifascicular block
- Hyperkalemia
- Digoxin toxicity
Diagnosis
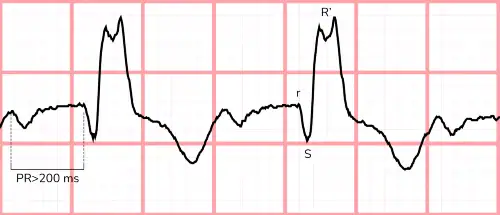
The diagnosis in this case is RBBB, left anterior fascicular block (LAFB), and first-degree atrioventricular (AV) block (ie, trifascicular block). The ECG shows a regular, wide-complex sinus rhythm with a rate of 100 beats per minute. The PR interval is prolonged (ie, greater than 200 msec), consistent with a first-degree AV block. The QRS duration is wide (ie, greater than 120 ms), with an atypical rSR′ pattern in V1 and a broad S wave in V5, V6, I, and aVL, consistent with a RBBB (Figure 2). There is marked left-axis deviation as evidenced by a dominant S wave in the inferior leads, suggesting the presence of LAFB.
Discussion
The infranodal conduction system is comprised of 3 fascicles: the right bundle; the left anterior fascicle; and the left posterior fascicle. The left anterior and posterior fascicles facilitate the rapid and coordinated contraction of the left ventricle while the right bundle does the same for the right ventricle. These 3 fascicles form the framework for the trifascicular conduction system. Any single fascicle or combination of fascicles can fail for various reasons including (but not limited to) primary degenerative disease, metabolic disturbances like hyperkalemia, ischemic heart disease, myocarditis, or long-standing hypertension. When all 3 fascicles fail, a ventricular escape rhythm ensues (ie, complete heart block). When 2 of 3 fascicles fail, it is termed a bifascicular block.1–4
The term “trifascicular block” refers to a bifascicular block with evidence of disease in the remaining fascicle. This term is somewhat misleading, as a true block (ie, failed conduction) of all 3 fascicles results in complete heart block. When 2 fascicles fail, as with this patient (ie, right bundle branch block and left anterior fascicular block), delayed conduction through a diseased third (and only functioning fascicle) will manifest electrocardiographically as a prolonged PR interval (ie, first-degree AV block). A first-degree AV block is often caused by delayed conduction within the AV node itself and can be benign, but when present concomitantly with a bifascicular block, it more likely represents delayed conduction through a diseased third (and only functioning) fascicle. For this reason, it is preferred to describe each individual abnormality rather than using the term “trifascicular block.”2
Due to extensive conduction involvement, patients with trifascicular disease are at high risk for progression to complete heart block (when the remaining functional, yet diseased, fascicle fails).5 Failure can occur transiently, therefore, patients presenting with complaints suggesting bradycardia or a bradycardic episode like syncope, weakness, confusion, or fatigue should be evaluated for permanent pacemaker placement even if the current ECG does not show bradycardia.
This patient’s symptoms are concerning for intermittent complete heart block and, therefore, transfer for monitoring, further testing, and pacemaker placement is warranted.
What to Look For
- Trifascicular block is an outdated term that describes a bifascicular block and a first-degree atrioventricular block.
- Look for the presence of a right bundle branch block, a left anterior (or posterior) fascicular block, and a prolonged PR interval.
- Patients with bi- or trifascicular conduction disease are at high risk for progression to complete heart block.
Pearls For Initial Management, Considerations For Transfer
- Patients with electrocardiographic evidence of bi- or trifascicuclar conduction disease with presenting complaints suggestive of bradycardia should be transferred to a facility with electrophysiology capabilities.
- Place pacing pads on the patient if available in preparation for transfer.
- Asymptomatic patients with bi- or trifascicular conduction disease are suitable to follow up with electrophysiology in the outpatient setting.
References
- Costa D Da, Brady WJ, Edhouse J. Bradycardias and Atrioventricular conduction block. Br Med J. 2002;324(March):535-538. doi:10.1136/bmj.324.7336.535
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhyth. Circulation. 2019;140(8):e382-e482. doi:10.1161/CIR.0000000000000628
- Elizari M V., Acunzo RS, Ferreiro M. Hemiblocks revisited. Circulation. 2007;115(9):1154-1163. doi:10.1161/CIRCULATIONAHA.106.637389
- Rosenbaum MB, Elizari M V., Lazzari JO, Nau GJ, Levi RJ, Halpern MS. Intraventricular trifascicular blocks. Review of the literature and classification. Am Heart J. 1969;78(4):450-459. doi:10.1016/0002-8703(69)90478-5
- McAnulty JH, Rahimtoola SH, Murphy E, et al. Natural history of “high-risk” bundle-branch block: final report of a prospective study. N Engl J Med. 1982;307(3):137-143. doi:10.1056/NEJM198207153070301
