Published on
Download the article PDF: Insights In Images July August 2025
Differential Diagnosis
- Brugada syndrome
- Left ventricular hypertrophy
- Wellens syndrome
- ST-Elevation myocardial infarction (STEMI)
Diagnosis
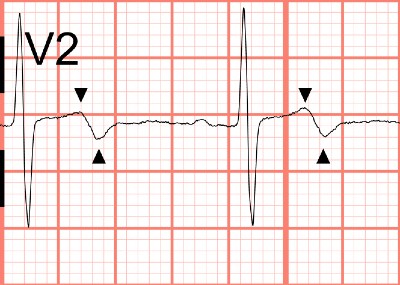
The diagnosis in this case is Wellens syndrome. The ECG demonstrates a normal sinus rhythm at 72 beats per minute. There are biphasic T waves with terminal negativity in V1 and V2. There is no significant ST segment elevation, no precordial Q waves, and preserved R wave progression (R wave >3 mm in V3). Wellens syndrome is suggested in this patient with anginal episodes who is currently chest pain free.1
Discussion
Wellens syndrome refers to an electrocardiographic pattern observed in patients with severe narrowing of the proximal left anterior descending artery (LAD). This pattern is typically seen in the precordial leads (V2 and V3) on the ECG: Type A presents with biphasic T waves and is seen in approximately 25% of cases (Figure 2); while type B has deeply inverted, symmetric T waves and is seen in approximately 75% of cases (Figure 3).2,3

The Wellens pattern is like T waves observed in patients who have recently undergone reperfusion via percutaneous coronary intervention (PCI) (ie, reperfusion T waves). Wellens syndrome is believed to occur when an occluded LAD spontaneously reperfuses.4 Wellens syndrome occurs in patients who are not currently experiencing chest pain. When these patients develop chest pain, the ECG may show “pseudonormalization” of the T waves, where they become upright and appear normal. If the occlusion persists, it can progress to an anterior ST-elevation myocardial infarction.
Unlike in Brugada syndrome or STEMI, the Wellens pattern typically shows minimal or no ST segment elevation. Although this pattern doesn’t meet criteria for STEMI, patients with Wellens syndrome are at high risk for LAD occlusion and require urgent coronary angiography. Patients with Wellens syndrome should be transferred to a PCI-capable facility.
In patients with left ventricular hypertrophy, it is common to see T wave inversion in the left-sided leads (V5 and V6) and ST elevation in the precordial leads. However, it’s crucial to recognize that these changes differ from the distinctive T wave patterns seen in Wellens syndrome and should not be mistaken for them.
What To Look For
- Biphasic (type A) or deeply inverted (type B) T waves in V2-3, which may extend to V1-6
- Minimal or no elevation of the ST segment
- Lack of precordial Q waves
- Preserved R wave progression
- Recent history of chest pain, but chest pain free on evaluation
- May have normal or minimally elevated cardiac enzymes
Pearls For Management, Considerations For Transfer
- These patients have an impending anterior wall myocardial infarction and must be transferred for urgent cardiac catheterization
- Stress test should be avoided, as it will precipitate an acute infarction
- The patient’s condition may change at any time, and they are critical in nature. If they have another episode of chest pain, repeat their ECG and look for an anterior STEMI or “pseudonormalization” of the anterior T waves—this means they are experiencing an acute reocclusion of their LAD
References
- de Zwaan C, Bär FWHM, Wellens HJJ. Characteristic electrocardiographic pattern in-dicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-736. doi:10.1016/0002-8703(82)90480-X
- Mead N, O′Keefe K. Wellen’s syndrome: An ominous EKG pattern. J Emerg Trauma Shock. 2009;2(3):206. doi:10.4103/0974-2700.55347
- Miner B, Grigg WS, Hart EH. Wellens Syndrome. StatPearls. Published online July 31, 2023. Accessed April 8, 2025. https://www.ncbi.nlm.nih.gov/books/NBK482490/
- Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. American Journal of Emergency Medicine. 2002;20(7):638-643. doi:10.1053/ajem.2002.34800

