Differential Diagnosis
- Sinus bradycardia
- Junctional escape rhythm
- Complete heart block
- Hyperkalemia
Diagnosis
The diagnosis is junctional escape rhythm. The ECG reveals narrow escape complexes at a rate of 60 beats per minute. Retrograde p’ waves are visualized immediately following the QRS complexes (Figure 2). Pacemaking cells exist throughout the conduction system, from the atrioventricular node through the distal Purkinje fibers. Inferior pacemakers are suppressed by the most superior (and dominant) one—usually the sinoatrial node. When impulses from the dominant pacemaker fail to conduct distally or an ancillary pacemaker outpaces and usurps control, an “escape” rhythm results.1 When a superior pacemaker fails to generate impulses at a rate faster than an inferior one, then the faster, more inferior, one will “escape.” In our case, the sinus node failed to generate a rate that outpaced the junction, which led to a junctional escape rhythm.
The junction refers to the part of the conduction system involving the atrioventricular node and the proximal His bundle (immediately inferior to the atrioventricular node). It is the only part of the conduction system capable of producing a narrow QRS complex, provided that the bundles remain intact. Junctional escape rhythms generally produce a rate of 40 to 60 beats per minute, whereas more distal ventricular pacemakers are slower and less reliable.2
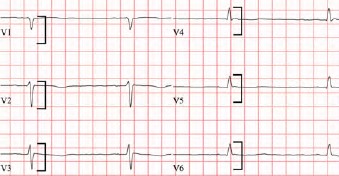
Normally, the atria depolarize from superior to inferior given the superior location of the sinoatrial node in the right atrium. The normal wave of atrial depolarization creates a positive deflection in the inferior leads (ie, II, III, and aVF), and a negative deflection in aVR—the typical morphology of P waves when the impulse originates from the sinoatrial node. Sometimes, when the impulse originates from the junction (or below), the atria will depolarize in the opposite direction (ie, from inferior to superior), and retrograde p’ waves can be seen immediately following the QRS complexes. Retrograde p’ waves are negatively deflected in the inferior leads (ie, II, III, and aVF) and positively deflected in aVR and V1 (Figure 2). Our patients ECG lacks typical P waves, indicating that the sinoatrial node failed to outpace the junction and resulting in a junctional escape rhythm with retrograde p’ waves. In the setting of preexisting heart failure, the decreased cardiac output associated with acute (relative) bradycardia can become symptomatic, as with this patient. Immediate transfer to an electrophysiology-capable facility is indicated.
There is no evidence of complete heart block given the lack of observed sinoatrial activity. While hyperkalemia is possible, there are no features to suggest that is the case (eg, peaked T waves or QRS widening).
What To Look For
- Junctional escape rhythms are narrow, and typically produce rates between 40 and 60 beats per minute.
- Retrograde p’ waves can be seen immediately following the QRS complexes, are upright in aVR and V1, and negatively deflected in the inferior leads.
Pearls For Initial Management And Considerations For Transfer
- Patients with symptomatic bradycardia warrant transfer to an electrophysiology-capable facility.
- If unstable, consider transcutaneous pacing.
References
- Mattu A, Tabas J, Brady W. Electrocardiography in Emergency, Acute, and Critical Care. 2nd ed. The American College of Emergency Physicians; 2019.
- Wagner GS, Strauss DG. Marriott’s Practical Electrocardiography. 12th ed. Lippincott Williams & Wilkins; 2014.
Click Here to download the article PDF

