Urgent message: Patients often present to urgent care with symptoms associated with urticaria and angioedema. Identifying the probable cause can provide relief of symptoms and abate patient concerns.
Urticaria and angioedema are rarely life threatening, but they are extremely disruptive to quality of life and sleep. In addition, hives may be alarming and lead patients to wonder if something serious is afoot. Swelling of the tongue or throat is particularly likely to be the source of some concern.
Small wonder, then, that patients with acute urticaria and angioedema are often first evaluated in an urgent care center.
In this article, we will discuss urticaria and angioedema from my perspective as director of the Allergy and Asthma Center at University Hospitals in Cleveland, OH and as presented in three distinct patients who were treated in an urgent care setting. I will also offer some perspective on when to refer to a specialist and will provide a few illustrative cases along the way.
Patients can adapt to many symptoms (including even moderate pain), but pruritis is not among them. Scratching is a response built into the nervous system; it cannot be denied and should be taken seriously.
The goals of management are to identify the likely cause(s), and to eliminate the urticaria or, when that is not possible, to alleviate the symptoms. It may not be practical or even necessary to make a definitive diagnosis in the urgent care setting, but you should be able to make a reasonable educated guess and create a treatment plan.
In most cases, the goal for urgent care is to initiate treatment and prescribe sufficient medications to get the person to their primary physician. It is when patients return to urgent care because of treatment failure and are still uncomfortable that diagnostic testing is indicated.
There are five provable etiologies of urticaria including allergy, infection, autoimmune processes, medication induced, and physical forms of urticaria. Most cases of idiopathic urticaria are probably autoimmune in nature.
It is not my purpose here to give an exhaustive review, but rather to provide some helpful background information, my personal strategy for a differential diagnosis when evaluating urticaria, and a framework for treatment. The bibliography contains some recent reviews that provide other points of view.
Case 1
C.R. is a 43-year-old woman who was referred to a specialist by an urgent care physician because of the new onset of urticaria and angioedema of four weeks duration. She was in urgent care six months earlier, in the spring, because of acutely worsened sinus pressure and mucopurulent drainage.
She had a long history of sinus symptoms and a strong family history of allergy. The physician prescribed amoxicillin and a steroid nasal spray. The patient improved and had no further problems until she presented with urticaria. At her initial visit for urticaria, she was given a Medrol Dosepak and an antihistamine; initially, she showed improvement but then worsened and returned to urgent care.
On her second visit, she had generalized urticaria and facial angioedema. She was given a two-week tapering course of prednisone. By the time she got in to see me she was hive free, but kept the appointment because she wanted to find out what caused the urticaria and swelling. What would be your differential diagnosis?
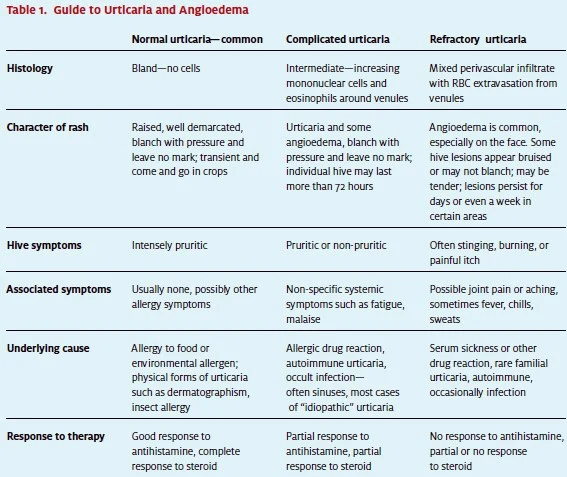
Although most hives look similar on exam, biopsy results show a spectrum of histological findings. (See Table 1.) Most of the time the tissue simply looks like saline was injected intradermally—
devoid of signs of inflammation—and on the other extreme it reveals an intense mixed perivascular infiltrate with extravasation of red cells from small venules.
Often, there is an intermediate picture with several perivascular mononuclear cells and perhaps a few eosinophils. This cell infiltrate (or lack thereof) correlates with benign forms of urticaria to progressively more aggressive forms of urticaria and, at worst, to urticarial vasculitis—the most severe form of urticaria with a moreserious differential diagnosis and prognosis.
So, how does this help us? The presence of a cellular infiltrate is associated with relative resistance to antihistamine therapy and increasing resistance to corticosteroid therapy, especially that element of the anti-inflammatory effect which occurs within hours or up to a few days. Table 1 shows the causes of some of these histological patterns, and we will find that certain skin symptoms and various associated systemic symptoms can lead us to a reasonable differential and treatment plan.
If we look at patient C.R. in light of Table 1, we see that her response to antihistamines and steroids place her in the complicated or refractory category, and that her history of sinusitis suggests the need to consider underlying infection as a cause. There may also be an allergic component based on her family history.
One could empirically prescribe an antibiotic, but if a limited CT of the sinus is readily available it would be very helpful. The treatment of infection-related urticaria is treatment of the underlying infection; usually, the hive response abates in 48 to 72 hours. I performed skin tests and found allergy to seasonal and perennial allergens. I elected to restart the nasal steroids and follow up with her in four weeks.
In retrospect, it seems likely that her urticaria and angioedema were related to both allergy and sinusitis. I believe that the steroids suppressed the allergic swelling in the sinuses and nasal passages and she was able to recover from infection on her own, but this is not the rule. She would have been better sooner and with fewer days of steroids if antibiotics had been prescribed on her second urgent care visit. In most patients with steroid refractory urticaria you should think of occult infection, usually in the sinuses. The patient may be unaware of infection, at least in part because the medications prescribed for urticaria suppress but do not alleviate the sinusitis symptoms.
Case 2
S.B. is a 32-year-old female who presented to urgent care with a two-week history of urticaria. Her hives were generalized but not particularly itchy, and occasionally mildly stinging. S.B. had a history of intermittent urticaria for the last year, but the symptoms never lasted more than a few days. On one occasion, she had slight swelling of her lower lip. There was no history of gastrointestinal or respiratory symptoms. She was postpartum 18 months with uneventful pregnancy and delivery. There was no history of any other medical problems or food allergy. She had taken loratidine regularly with little or no relief of the rash. She had no family history of allergy, urticaria, or eczema, but there was a maternal history of thyroid disease. She was taking only oral contraceptives and prenatal vitamins, and denied over-the-counter drugs, including NSAIDs.
Two days prior to this recent episode she had eaten a “shrimp fest special” at a seafood restaurant. There was no known allergy to medication. Exam showed well-demarcated, typical urticaria lesions measuring 1cm to 2 cm which blanched with pressure. The physician told her to change her laundry detergent and to avoid shellfish and gave her prescriptions for fexofenadine 180 mg and ranitidine 300 mg, both to be taken daily. A week later, S.B. returned complaining of worsening urticaria and swelling of her face on the right side. The physician ordered a CBC, sed rate, ANA and a C1 esterase inhibitor level. She also ordered a medrol dosepak in addition to the prior medications.
A week later the patient was back with some improvement but then another relapse, and all lab work was within normal limits. What would be your differential diagnosis?
The scenario described here reveals several errors and misconceptions.
First, laundry detergent is virtually never a cause for hives, although it may possibly produce a flat, slightly red irritant reaction. There are only a few causes of contact urticaria; they include latex, benzoyl peroxide, and some make-ups.
Secondly, hereditary angioedema is a rare disease, and when it does occur urticaria is never part of the syndrome. In other words, if angioedema is accompanied by urticaria, C1 esterase inhibitor deficiency is never in the differential diagnosis.
Also, food allergy causes urticaria by an immediate hypersensitivity reaction which occurs minutes to hours after exposure, but never days later. Therefore, we can rule out contact, food, and C1 esterase deficiency as causes.
There is no evidence for drug allergy or physical forms of hives. Refractoriness to antihistamine and steroid suggests autoimmune or infectious etiology. In the event of poor or no response to antihistamines, it is pointless to add an H2 blocker.
In the absence of anything to suggest infection, I would make a tentative diagnosis of autoimmune urticaria. S.B. has a family history of thyroid disease and a sputtering onset of hives, leading me to suspect thyroid autoimmunity. This is sometimes seen postpartum, or even during pregnancy.
Urticaria is frequently the presenting sign, even before thyroid function is abnormal. This may be documented by the presence of serum anti-thyroid peroxidase antibodies. The levels of auto-antibodies over time may correlate with the severity or urticaria. This form of urticaria can be difficult to control, but maybe helped by treating hypothyroidism if present, and may spontaneously remit over months or years.
I usually bargain with the patient for 80% control of symptoms by means of a daily antihistamine and/or a small dose of oral corticosteroid on an every-other-day basis and hope it just goes away. This patient needs to be followed up by a specialist.
Case 3
Our last patient, J.B., is a 4-year-old Amish girl brought in by her father on a beautiful early September afternoon because of swollen face and eyes. J.B. had no prior history of hives, swelling, or allergy. She had taken no medicines and eaten no new foods. The family had come from the Geauga County Fair where they had purchased a horse. J.B. was experiencing very slight nasal congestion and generalized pruritis, but no respiratory or other symptoms. On exam, she was in no acute distress, but was scratching her forearms. Her left upper lip was swollen, but mouth and tongue were normal. Upon opening the eyes there was moderate conjunctivitis.
The rest of the exam was normal, but where she was scratching there were linear welts. She responded in an hour to diphenhydramine and injected corticosteroids. She was referred to me for follow-up, and skin testing showed a strong positive test to ragweed, and horse was negative. Her father and teenage sibling reported a history of hayfever, but no family member had hives or swelling.
This case illustrates the occasional presentation of acute seasonal allergy with exclusive skin manifestations, along with conjunctivitis here.
Another variation is generalized hives or dermographism presenting along with respiratory manifestations of environmental allergy. A possible clue, as was the case here, is presentation during the peak of a pollen season, or after exposure to a very potent allergen such as dust mite or animal dander. Apparently, enough environmental allergen can be inhaled and ingested to cause a generalized hive reaction.
In the Midwest, the ragweed season peaks in the first week of September, and usually Labor Day weekend has high pollen counts. Some cases of chronic urticaria are purely allergic in nature and respond to avoidance and antihistamines on a regular basis.
Summary
As can be seen from the preceding cases, treatment with antihistamines is the first step for treating urticaria, and the response to antihistamine may have diagnostic implications, as well. Oral antihistamines should never be prescribed for prn use, since they are preventative by occupying the H1 histamine receptor.
Patients often assume that antihistamines are to be used prn unless they are specifically instructed to take them on a daily basis, even if they have no hives.
Similarly, oral corticosteroids are usually very effective for treating urticaria and angioedema, and their failure implies a complicated or severe form of the disease. You may have noticed absence of discussion of the role of epinephrine in the treatment of urticaria and angioedema.
Epinephrine is the first-line treatment for anaphylaxis, and there may be some difficulty at times determining whether severe hives and angioedema actually are the presenting signs for anaphylaxis. Of course, in that case epinephrine should be administered. Epinephrine is never a routine choice in most cases of hives, however, because first there is some risk involved in giving the drug and, secondly, because it has a duration of action of only a few hours at best. Dermatographism is a frequent feature of many patients with urticaria, and has no special diagnostic implications. Other physical forms of hives, such as pressure-induced, solar, and cold-induced urticaria are usually self evident. Likewise, angioedema has no special significance unless it presents without hives, and even then I see it mostly in patients taking ACE inhibitors. There is no pressing need to have a definitive diagnosis at the urgent care level, except in the case of underlying infection, which usually responds only to antibiotic treatment.
It is appropriate for the urgent care provider to refer the patient on oral antihistamines or a short burst of corticosteroid back to their primary physician. If an allergic cause is strongly suspected, then referral to an allergist may be appropriate. I hope that these insights, gleaned over 20 years of practice, and Table 1 will provide a framework for managing urticaria and angioedema.
These may also help you with patient communications. On a daily basis, you deal with many serious medical conditions, but none that beg the question “why?” more than urticaria. Patients literally lie awake at night wondering what caused their hives. It is very helpful to reassure them that much of the time a cause can be found and it is usually benign—and, more importantly, that the symptoms can be controlled.