Urgent message: When a patient presents to urgent care after a syncopal event, the clinician’s charge is to determine whether the episode was of benign or potentially life-threatening etiology and whether the patient should be transferred for further evaluation.
Introduction
Syncope is a sudden, transient loss of consciousness with a loss of postural tone (typically, falling). It results from an abrupt, transient, and diffuse cerebral malfunction and is quickly followed by spontaneous recovery. The term syncope excludes seizures, coma, shock, or other states of altered consciousness. Many patients will ascribe their syncopal episode to a situationally mediated vasovagal episode.
Despite this, the goals in the urgent care setting include the following:
- Determining whether the patient’s episode was actually a syncopal or presyncopal event, and if it could have a life-threatening etiology
- Stabilizing the patient
- Transferring those patients who need further diagnostic studies or therapeutic interventions
Epidemiology
Syncope accounts for up to 3% of emergency department (ED) visits and up to 6% of hospital admissions each year in the United States.1,2 At some time in their lives, up to about half the population (12% to 48%) of people may experience syncope.3 Syncope occurs in all age groups, but it is most common in adults. Non-cardiac causes tend to be more common in young adults, while cardiac syncope becomes increasingly more frequent with advancing age.4 The chance of having at least one syncopal episode in childhood is between 15% and 50%.5 Though a benign cause is usually found, syncope in children warrants prompt detailed evaluation.6 With advancing age comes an increased frequency of coronary artery and myocardial disease, arrhythmia, vasomotor instability, autonomic failure, polyneuropathy, and the use of polypharmacy—all of which can contribute to syncope. Therefore, advanced age is an independent risk factor for both syncope and death.7
Pathophysiology
Regardless of specific cause, on the most basic level syncope results from the sudden reduction in the delivery of a vital substrate (usually oxygen) to both cerebral hemispheres or to the brainstem’s reticular activating system.Most often, this is due to a localized or systemic reduction (35% or more) in blood flow to these areas. Since brain tissue cannot store energy, cessation of cerebral perfusion lasting only three to five seconds will result in syncope. This is most frequently caused by a transiently diminished vagal tone or autonomic nervous system disorders (such as in patients with diabetes). Patients who experience vasovagal reactions have subnormal vagal baroreflexresponses with a disappearance of muscle sympathetic nerve activity.8
Syncope can, however, also be due to transient hypoglycemia, toxins, metabolic abnormalities, failure of autoregulation, and primary neurological derangements.
The causes of syncope may be categorized into three broad groups: cardiovascular, non-cardiovascular, and unknown. This categorization stratifies the patient’s future risk for serious associated illnesses and death; generally, cardiovascular syncope is associated with higher mortality than syncope due to non-cardiovascular or unknown causes.
Cardiovascular Syncope
Cardiovascular syncope may be due to autonomic dysfunction, orthostatic hypotension, obstructive lesions, and dysrhythmias. Each of these has its own etiology.
At all ages, the most common cause of syncope is autonomic dysfunction, which results from a slowing of the heart and decreased cardiac output due to increased vagal tone. This is often described as “fainting.” Any number of factors, such as the bradycardia often seen in athletes, may cause increased vagal tone, and some individuals seem more prone to these episodes than others. Emotional stress, hot or crowded conditions, the sight of blood, and pain may often precipitate these events. Diabetics and the elderly often have disruption of their autonomic systems leading to syncope. In all these cases, a good history may help determine whether a syncopal event was vasovagal or due to a more serious cause. (While tilt-testing may eventually suggest that a syncopal event from unknown cause was vasovagal, no real “gold standard” for vasovagal syncope exists.)9
Orthostatic hypotension is a clinical syndrome indicating diminished intravascular volume. A commonly encountered cause of syncope that often requires treatment, it is often caused by dehydration (often secondary to acute gastroenteritis), and is also seen with excess intake of medication and acute anemia from hemorrhage.
Dysrhythmias may have multiple causes but, if they cause syncope, are usually of acute onset. Such dysrhythmias may arise from any focus (supraventricular, nodal, or ventricular) and be bradycardic, tachycardic, or unorganized (e.g., ventricular fibrillation). Pacemaker failure results in syncope when the underlying rhythm cannot sustain a sufficient cardiac output. Severe bradycardia, caused by minimal pressure on the carotid, causes carotid sinus syncope. It can be exacerbated by carotid lesions or digitalis toxicity.
Obstructive lesions result from a diminished effective cardiac output due to structural abnormalities. Most commonly, these are in or around the heart—either acquired or congenital lesion—but can also occur with outflow obstruction due to a pulmonary embolus or aortic dissection.
Non-Cardiovascular Syncope
Non-cardiovascular syncope may be due to metabolic derangements, neurologic abnormalities, or psychiatric disease. Again, establishing the root of the suspected cause of the syncope may help clarify management options.
Metabolic derangements can develop slowly (e.g., alcoholism, hypothyroidism) or rapidly (e.g., hypoglycemia, hypoxia). Syncope is the sudden, final common pathway for these disorders. On occasion, they may lead to seizures or coma, rather than syncope.
Neurologic abnormalities are a relatively rare cause of syncope. Instead, atypical seizures may initially be described as syncope. Without extensive testing, the two may be difficult to differentiate.
Psychiatric disease or medications may cause syncope due to a vagal effect, hyperventilation, or a drug effect. However, it is dangerous to ascribe a syncopal episode to a psychiatric cause without some investigation, including a good history and physical examination.
Diagnostic Evaluation
History and physical examination are the most specific and sensitive ways to evaluate syncope. Cursory review of the literature shows that diagnosis can be made with a thorough history and physical examination in 50% to 85% of patients.7 No single laboratory test has greater diagnostic efficacy.
History
Proper diagnosis, or at least correct patient disposition, requires combining patient and bystander history with risk factors (age, cardiac history, and significant other medical history—including medication/drug/alcohol use) and the limited information that can be gained from the physical examination and diagnostic tests.
Witnesses to the syncopal event can often describe its character and time course far better than the patient (who, by definition, was unconscious). Key historical clues include:
- Setting (activities preceding syncope)
- Prodrome (aura, chest pain, dyspnea, vertigo, diaphoresis, graying of vision)
- Abruptness of onset (gradual or sudden)
- Position when it occurred (standing, sitting, supine)
- Movement during/after syncope (tonic-clonic or myoclonic movements)
- Duration (seconds, few minutes, longer)
- Rate or recovery (rapid, slow, incomplete/prolonged)
Presyncope, where there is no loss of consciousness, requires the same evaluation as syncope. While patients with syncope do not remember actually hitting the ground, those experiencing presyncope have the same symptoms, but the event terminates prior to loss of consciousness. Presyncope can still cause the patient to lose postural tone, however.
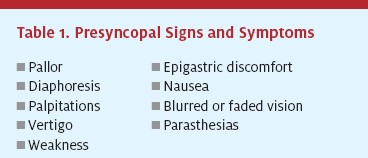
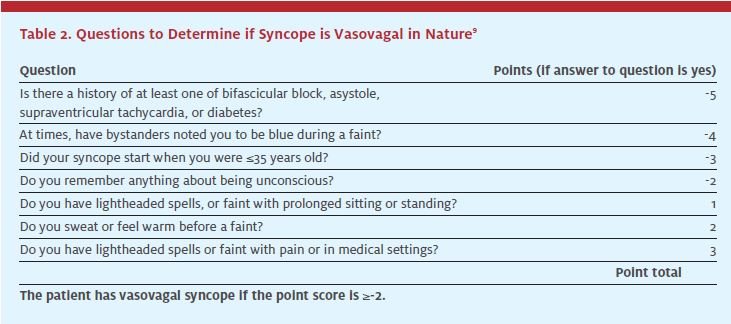
Prior faintness, dizziness, or light-headedness occurs in 70% of patients experiencing syncope; other presyncopal signs and symptoms may also occur, alone or in combination (Table 1), whether syncope actually follows or not. In dysrythmia-related syncope, presyncopal symptoms last only seconds, though in vasovagal events they can last about 2 1⁄2 minutes.7 A group at the University of Calgary, Canada, developed a set of historical questions that can help determine if the patient’s syncope was due to a vasovagal episode or something more sinister (Table 2). If the patient experiences typical pre seizure aura, this suggests a seizure rather than syncope.
Red Flags
Some specific symptoms or activities associated with the syncopal event should raise concern about life-threatening causes.
- Chest pain, with or without palpitations or dyspnea, may accompany myocardial ischemia or infarctions, aortic dissections, or dysrhythmias. These symptoms may be present as a presyncopal prodrome, following syncope, or both. Ventricular and supraventricular dysrhythmias may not be present on an initial ECG; prolonged monitoring may be necessary. Bradyarrhythmias and pacemaker malfunctions can usually be seen immediately.
- Dyspnea may accompany cardiac-related syncope, or may be a symptom of pulmonary embolus or congestive heart failure, both of which may cause syncope.
- Severe headache or new neurological deficits may indicate a neurological cause for the syncope or a serious consequence of the syncopal event. Neurological syncope may have prodromal symptoms such as vertigo, dysarthria, diplopia, and ataxia.
- These may suggest a stroke or transient ischemic attack. If symptoms appeared following a fall associated with syncope, trauma should be considered.
- Abdominal or back pain may suggest a source of acute bleeding, such as from a ruptured abdominal aortic aneurism, or in the pregnant patient, an ectopic pregnancy or placental abruption.
- Strenuous exertion just before syncope, especially in young athletes with a cardiac murmur, suggests syncope due to cardiac outflow obstruction. In any group, syncope can be very worrisome if it is due to aortic stenosis, hypertrophic obstructive cardiomyopathy, mitral stenosis, pulmonary stenosis, pulmonary embolus, left atrial myxoma, or pericardial tamponade.
Certain predisposing events may suggest more benign causes of syncope. Even here, however, care should be taken to avoid missing serious underlying disease. A variety of events can increase vagal tone and cause syncope. In these cases, syncope occurs from decreased peripheral vascular resistance due to stimulation of efferent vasodepressor reflexes. Asking about the patient’s activity prior to syncope may suggest the etiology. These often self-limiting problems are the most common cause of syncope in young adults; behavioral changes may help to avoid a recurrence.
In elderly patients, 45% of orthostatic syncope cases are related to medications. Medications may increase vagal tone and incite these events. In those cases, the dosage may need to be adjusted or the medication changed. Dehydration and decreased intravascular volume can also lead to syncope, but consideration should be given to underlying heat illness, blood loss, or other more serious causes for this condition.
Syncope or Seizure?
A common challenge for the clinician is distinguishing syncope from seizures. While this may require extensive testing in some patients, there are some historical clues that can help. If witnesses note convulsive activity or, especially, postictal confusion, this probably indicates a seizure. Post-syncopal confusion occurs, but rarely lasts more than 30 seconds; confusion following a seizure usually lasts much longer. In addition, patients should be asked if they remember being confused about their surroundings after the event and whether they have oral trauma, incontinence, or myalgias. Witnesses may also be confused by the myoclonic jerks that sometimes accompany syncope, although these usually last only a very short time.
Medication, drug, and alcohol use are relatively common precipitants of syncope, so this history should be taken in detail. Medications that reduce blood pressure (e.g., antihypertensive drugs, diuretics, nitrates), affect cardiac output (e.g., beta-blockers, digitalis, antiarrhythmics), prolong the Q-T interval (e.g., tricyclic antidepressants, phenothiazines, quinidine, amiodarone), or alter the sensorium (e.g., sedating analgesics, hypnotics, anxiolytics) may all cause syncope, for example. Clinicians should ask about any recent changes in medication dosage, new medications, and anything that may have changed the body’s level of the medication, such as food, illness, or dieting. Illicit drug and alcohol use may also cause syncope and, on occasion, may presage serious events (e.g., cocaine-induced myocardial infarction, delirium tremens).
Finally, the clinicians must also inquire about other serious personal and family medical conditions, especially cardiovascular disease. Patients with a history of myocardial infarction, arrhythmia, structural cardiac defects, cardiomyopathy, or congestive heart failure fall into a high-risk group for death and disability. Those with a family history of sudden death or serious cardiac disease should also be considered in this category.
Physical Examination
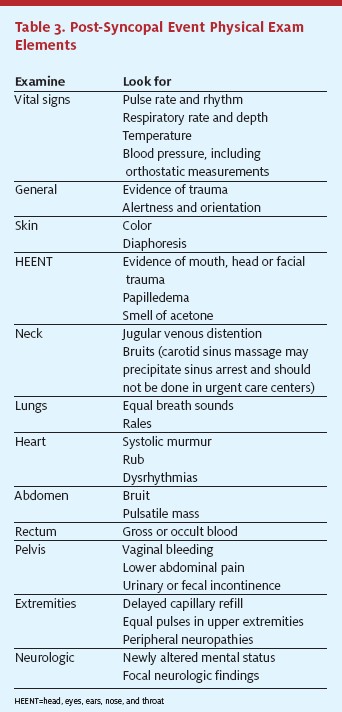
The physical examination supplements clinical opinions formed from the patient and bystander history. While it may confirm suspicions or add new information, it should only be considered a supplement to the clinical history. During the physical exam, it is important to recognize signs of trauma, since syncope from any cause can result in injury with significant morbidity and mortality, especially in the elderly10 (Table 3).
Laboratory/Imaging
Ancillary testing rarely provides additional useful information. The exception is the ECG, which can be diagnostic for acute myocardial ischemia or infarction, dysrhythmias, prolonged Q-T intervals, bundle branch blocks, pacemaker malfunction, and other cardiac disease. Most patients presenting with syncope or presyncope should have an ECG. Patients should be referred if they require prolonged cardiac monitoring to identify intermittent dysrhythmias.
Although diagnostic in less than 2% of syncopal patients, the rapid and inexpensive fingerstick blood glucose always should be checked. In those patients with hypoglycemia, rapid therapy may immediately be instituted. If hyperglycemia is found, a diabetic complication may be considered (ketoacidosis, neuropathy, and autonomic dysfunction). For similar reasons, a dipstick urinalysis should be performed, especially on all elderly patients, since a urinary tract infection may precipitate syncope and can be easily treated.7
Likewise, a chest radiograph should be considered in all patients, especially the elderly. It may demonstrate evidence of infectious or aspiration pneumonia, congestive heart failure, a pleural effusion, a lung mass or a widened mediastinum.7 Except in unique circumstances, serum electrolyte levels with renal function tests and the complete blood count are of scant utility in making a diagnosis or determining disposition, although one predictive model, the San Francisco Syncope Rule, does use the hematocrit as one factor.11 Fecal occult blood testing and testing for significant abdominal pain during the physical exam is a far better way of identifying occult blood loss. Electrolyte testing may be needed only if seizure is being seriously considered. If the patient is on antiepileptic medications, those levels may also need to be drawn after consulting with the patient’s neurologist. If the patient warrants having cardiac enzymes or creatine kinase (for a prolonged seizure or period of unconsciousness) drawn, he or she should be sent to the emergency department, and probably admitted to the hospital.
Those patients requiring more intensive imaging (e.g., head CT scan, chestabdomen scan, pelvic ultrasound, MRI, echocardiography, EEG, or tilt testing) should be referred to an ED or their personal physician, depending upon the urgency of the situation. Criteria to Transfer/Refer Patients Two decision rules have been published that help to identify those at most risk after syncope. However, patients not meeting these criteria still were at significant risk for untoward events in the subsequent year. One model demonstrated that between 58% and 80% of patients with at least three of the following risk factors suffered identifiable dysrhythmias or death within one year:
- Abnormal ECG findings
- History of ventricular arrhythmia
- History of congestive heart failure
- Age>45 years
Incidence of dysrhythmias or death was 4%-7% among patients with no risk factors, and was 58%-80% for patients with three or four risk factors.12 Another model identified patients who are at immediate risk for serious outcomes within seven days, with a 96% sensitivity. Its criteria was the presence of abnormal ECG findings, a history of congestive heart failure, dyspnea, a hematocrit less than 30%, and a blood pressure less than 90 mm Hg.,sup>11 The question is, will a 4% short-term serious outcome rate be acceptable?
Prognosis
The differential diagnosis (Table 4)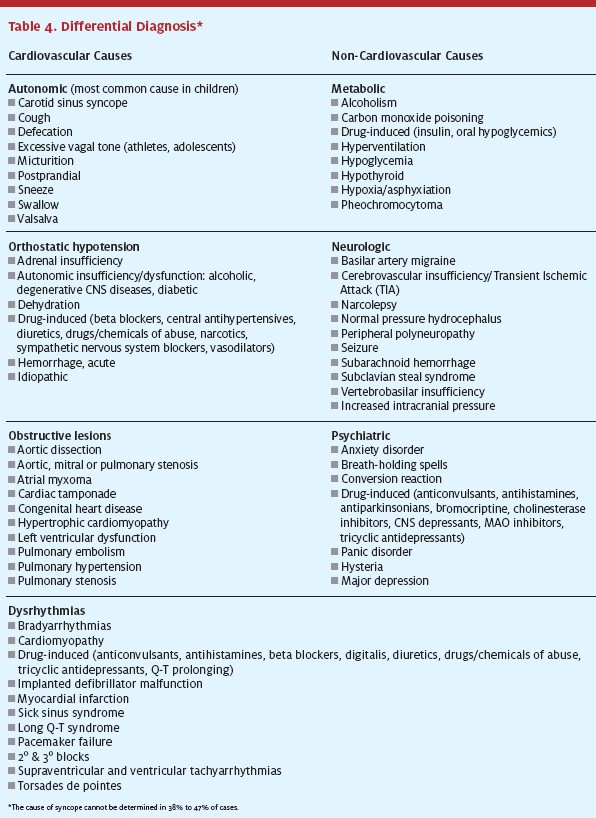 includes many life-threatening conditions. The clinician’s primary goal is to distinguish life-threatening etiologies—mainly due to cardiovascular causes—from those that are more benign. The most common serious causes of syncope are dysrhythmias and myocardial ischemia. Less common serious causes include cerebrovascular events, toxicmetabolic abnormalities, and critical aortic stenosis. Rarely seen, but life-threatening, causes are thoracic aortic dissections, massive pulmonary emboli, and subarachnoid hemorrhages. Young, healthy patients with a clearly benign cause of the syncopal episode are the only ones that can be discharged safely without a more intense evaluation or additional treatment. Even so, it should be noted that 30% of athletes dying during exercise had syncope as a sentinel event.13
includes many life-threatening conditions. The clinician’s primary goal is to distinguish life-threatening etiologies—mainly due to cardiovascular causes—from those that are more benign. The most common serious causes of syncope are dysrhythmias and myocardial ischemia. Less common serious causes include cerebrovascular events, toxicmetabolic abnormalities, and critical aortic stenosis. Rarely seen, but life-threatening, causes are thoracic aortic dissections, massive pulmonary emboli, and subarachnoid hemorrhages. Young, healthy patients with a clearly benign cause of the syncopal episode are the only ones that can be discharged safely without a more intense evaluation or additional treatment. Even so, it should be noted that 30% of athletes dying during exercise had syncope as a sentinel event.13
Most causes of syncope are benign. Hence, persons with non-cardiovascular causes or syncope of unknown origin have a relatively benign prognosis, with a one-year mortality rate of 12% and 6%, respectively.2,14 Vasovagal and orthostatic syncope do not increase mortality, though orthostatic syncope often recurs. Typically, syncope of unknown etiology has a favorable prognosis, with one-year follow-up data showing a low incidence of sudden death (2%), a 20% chance of recurrent syncope, and a 78% remission rate.7 However, patients with preexisting cardiovascular disease have a greater risk of short- and long-term mortality after a syncopal episode from any cause. Syncope caused by a cardiac disorder carries a one-year mortality rate of 20% to 30% and a 33% incidence of sudden death over five years.2,3,14,15 Risk is higher in older patients and those with serious comorbidities, with mortality rates significantly increased within both four weeks and one year after presentation.
1 Elderly patients have a 30% incidence of a recurrent syncopal episode.13
Syncope of any etiology in a cardiac patient (to be differentiated from cardiac syncope) has also been shown to imply a poor prognosis. Patients with NYHA functional class III or IV who have any type of syncope have a mortality rate as high as 25% within one year.7
Summary
Syncope has a long differential diagnosis that includes many life-threatening conditions. History, from the patient and bystanders, is the key diagnostic tool in urgent care to determine whether a patient needs further evaluation and treatment. Physical examination plays an important, but lesser, role. Except for the ECG, fingerstick glucose, dipstick urinalysis, and chest radiograph, laboratory and imaging do not play an important role in urgent care decisions about patient disposition or treatment after syncope. Any abnormal cardiac findings or potentially serious suspected cause of the syncopal event warrants transfer to an ED. If a life-threatening condition is suspected, patients should be transported immediately via the EMS system.
REFERENCES
1. Colivicchi F, Ammirati F, Melina D. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J. 2003;24:811-819.
2. Hayes OW. Evaluation of syncope in the emergency department. Emerg Med Clin North Am. 1998;16: 601-615, viii.
3. Kapoor WN. Evaluation and management of the patient with syncope. JAMA. 1992:268:2553-2560.
4. Sun BC, Emond JA, Camargo CA Jr. Characteristics and admission patterns of patients presenting with syncope to U.S. emergency departments, 1992-2000. Acad Emerg Med. 2004;11:1029-1034.
5. De Lorenzo RA. Syncope. In: Marx JA, Hockberger RS, Walls RM, eds. Rosen’s Emergency Medicine. 6th ed. St. Louis, MO: Elsevier Mosby; 2006:193-199.
6. Pratt JL, Fleisher GR. Syncope in children and adolescents. Pediatr Emerg Care. 1989; 5:80-82.
7. Morag R, Brenner B. Syncope. Emedicine. Available at: www.emedicine.com/emerg/topic876.htm. Accessed August 26, 2006.
8. Morillo CA, Eckberg DL, Ellenbogen KA, et al. Vagal and sympathetic mechanisms in patients with orthostatic vasovagal syncope. Circulation. 1997;96:2509-2513.
9. Sheldon R, Rose S, Connolly S, et al. Diagnostic criteria for vasovagal syncope based on a quantitative history. Eur Heart J. 2006;27:344-50.
10. Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141-158.
11. Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43:224-232.
12. Martin TP, Hanusa BH, Kapoor WN. Risk stratification of patients with syncope. Ann Emerg Med. 1997;29:459-466.
13. Silverstein MD, Singer DE, Mulley AG, et al. Patients with syncope admitted to medical intensive care units. JAMA. 1982:248:1185-1189.
14. Soteriades ES, Evans JC, Larson MG. Incidence and prognosis of syncope. N Engl J Med. 2002;347:878-885.
15. Junaid A, Dubinsky IL. Establishing an approach to syncope in the emergency department. J Emerg Med. 1997:15:593-599.
22. The Journal of Urgent Care Medicine | October 2006 www.jucm.com
