Urgent Message: Patients with tooth-related complaints increasingly are presenting to urgent care centers. Managing these cases can be a challenge because physicians often receive limited training in this area.
KATHERINE HURST MSC, MD, and RICHARD E. WALTON DMD, MS
Tooth or tooth-related complaints are common presenting issues in patients seen at urgent care centers because of the limited availability of dental services in the evenings and on weekends. More patients also are seeking emergency dental treatment in hospitals or similar facilities as the U.S. population continues to age and the number of individuals who are uninsured (or underinsured) increases.1
Urgent care providers, therefore, need to have some working knowledge of the management of common dental emergencies but they may not because physicians typically receive limited training about these problems. To meet the challenge of diagnosing and managing dental problems likely to be seen in an urgent care setting, providers should understand the disease process, be familiar with the presentation and diagnosis, and be able to design, a treatment protocol to manage a patient’s injury, relieve his or her pain, and prevent the spread of the infection.
Oral-related issues often after caused by hard- and soft-tissue injuries, pain, or infection.2 Most dental emergencies are localized, but some may spread to involve fascial spaces (cellulitis), possibly requiring hospitalization and more extensive and expensive systemic treatment.2
Severe dental infections tend to occur in individuals from lower socioeconomic groups who have limited access to dental care. Therefore, they are more commonly seen in an emergency or urgent care setting than in the average dental practice. Such presentations may also be further complicated because patients with dental emergencies often have other medical issues related to existing dental and systemic diseases or chemical addictions, or they suffer from poor nutrition.
Although comprehensive dental procedures are not within the scope of practice of most urgent care providers, therapies are available in the clinic to provide patients with some degree of relief from acute pain and to minimize adverse reactions to infection and tooth injuries. The article briefly describes common and less common, treatable dental emergencies. Background information as to pathosis, clinical findings, basic diagnostic procedures and a treatment plan for each diagnosis is included. Also described are conditions that may be interpreted as an emergency by the patient, but that do not require immediate treatment. Another consideration is non-dental conditions that can mimic toothache because of referral from other structures. In this category are sinusitis, temporomandibular dysfunction, (muscles of mastication pain), herpetic lesions, margarine or cluster headaches, and neuralgias. These conditions must be differentiated from odontogenic problems and treated (or not treated) accordingly.
Pulpal and Periapical Pathoses
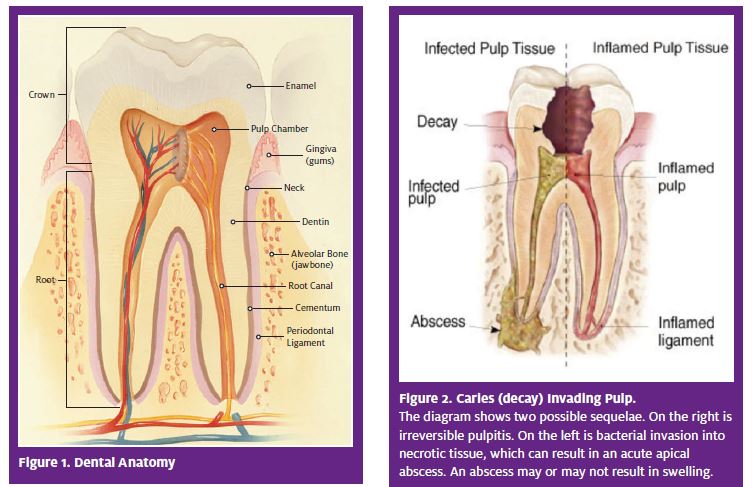
The most common causes of emergency visits for dental companies are pulpal and periapical pathoses.3 These presentations represent progression of disease from the crown of the tooth to the pulp (if untreated) and then eventually to the periapex, which is the medullary bone in the region of the root tip. Because the root is surrounded by alveolar bone, disease in this region has the potential to involve the overlying soft tissues (Figure 1).
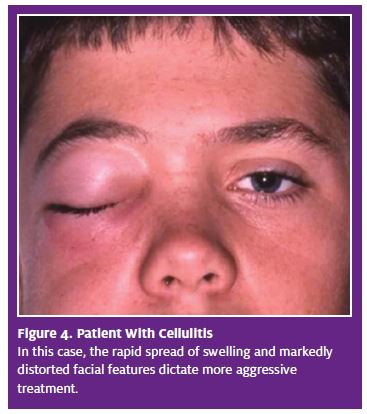
Pulp injury has many etiologies, but the most common initiator of pulp disease is dental caries, commonly known as a “cavity.” Caries is a disease of hard tissues that involves bacterial invasion from surface plaques (bacterial masses). The bacteria, in combination with a carbohydrate and invade the enamel, then the dentin. If the decay process is not corrected by the dentist with removal and restoration, bacteria will continue to demineralize tooth structure and eventually reach the vital tissues of the pulp (Figure 2). Caries confined to hard tissues results in the reversible pulpitis, which is localized immune response in the pulp. This inflammatory process is usually asymptomatic, but can cause sharp, brief pain, particularly in response to cold. This condition is not a significant pathosis or an emergency and does not require immediate treatment.
Most emergency room or urgent care visits for dental issues are for either irreversible pulpitis or a cute apical abscess.
Irreversible Pulpitis
Pathosis.
When dental caries, with the attendant bacteria, invade the pulp, the result is a localized tiny area of liquefaction necrosis (microabscess), confined to the coronal pulp, and colonization of bacteria. Other injuries, such as extensive restorations or fractures, also can cause severe pulp injury, or irreversible pulpitis (Figure 2). By definition, this condition cannot resolve by itself; either root canal treatment or extraction is required. If neither is performed, the microabscess will progress, either rapidly or slowly, to involve the entire pulp. Again, the resultant inflammation is primarily an immune response to bacterial byproducts and to leukocytic enzymes and chemical mediators. It is not a true infection.
Clinical presentation and diagnosis. Irreversible pulpitis typically is asymptomatic, although it can be extremely painful. For unknown reasons, occasionally the inflammation becomes very active, producing an excess of fluid transudates and exudates and mediators. Because the pulp space is non-compliant (cannot swell), fluid pressures increase and stimulate C-fibers. The pulp is richly innervated with sensory nerves with an abundance of receptors. The pain tends to be exaggerated by thermal stimuli and is often referred and poorly localized; that is, the patient cannot identify the offending tooth. Significant pain on biting or pressing on the tooth or overlying tissues is unlikely. Intraoral examination usually (but not always) enables identification of the problem and the offender, that is, a tooth with deep decay or with a large restoration or fracture.
Treatment plan. The preferred treatment is either immediate removal of the inflamed pulp by root canal treatment and preparation of the tooth for restoration, or extraction, if the tooth cannot be saved. In an urgent care setting, it may not be feasible to implement either of these treatment options. Therefore, the best temporary measures are local anesthesia and analgesics to maintain the patient until he or she can visit a dentist.
Pain control. The preferred anesthetic agent is articaine, which penetrates bone best. Infiltration of the maxilla over the tooth apex will provide 1 to 2 hours of relief, enough time for oral analgesics to take effect and ease the pain. (Total relief is unlikely.) Infiltration on the mandible is less successful, but will give some relief. On the mandible, the preferred injection is an inferior alveolar block. Video tutorials on the inferior alveolar nerve block (IANB) are available at http://www.youtube.com/watch?v=sZgLtbNe6ek and http://www.youtube.com/watch?v=Yhu4ROEP4ZA.
The best analgesic approach is a combination of narcotics (oxycodone or hydrocodone) with nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen. Antibiotics are of no benefit and are contraindicated, because irreversible pulpitis is not an infection and does not have systemic effects.4 Hospitalization is not required, and while the condition can be very painful, it is not serious. Follow-up. Instruct the patient to visit a dentist for definitive care, which will be either root canal treatment or extraction.
Acute Apical Abscess
Pathosis. In this situation, as a result of complete necrosis of the pulp, inflammation reaches the alveolar bone at the root tip and an abscess often develops in the bone. The abscess may be confined to noncompliant bone (very painful), or spread to the soft tissues on the lateral (facial) or lingual (medial) sides, with resultant swelling (less painful). Infrequently, the abscess may move into the fascial spaces, which is potentially more serious, and in rare cases, life-threatening.
The acute apical abscess (AAA) seldom has systemic manifestation. A localized AAA, with or without swelling, does not result in elevated temperature, malaise, altered pulse rate or blood pressure changes because it has effectively been localized by the body’s defenses.5 Cellulitis also does not usually produce major systemic complications. Swelling and distortion of the face and/or neck may be diffuse and extensive, but elevated temperature or malaise may not occur. No reports exist of sepsis or other consequences of cellulitis on other systems.
Clinical presentation and diagnosis. As previously stated, if an abscess is confined to bone, there will be no swelling. The pain tends to be intense and localized to the offending tooth, which is very tender to biting and pressure. The discomfort is a result of fluid accumulation and pressure related to the abscess per se and because of inflammatory mediators stimulating receptors.
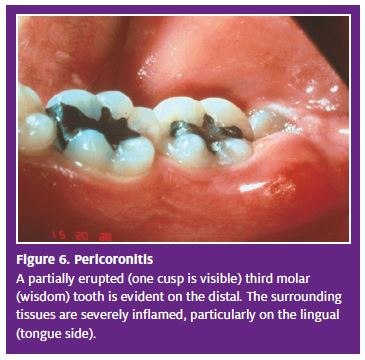
Swelling often is present but usually confined to overlying mucosa, either buccal (commonly) or lingual (occasional) (Figure 3). Localized swelling often is accompanied by facial edema that is noticeable extraorally. Again, the localized swelling does not have systemic manifestations or complications because it has been effectively controlled by the body’s defenses. After a time, it may develop into cellulitis (seldom) or may regress spontaneously if untreated with drainage and/or debridement. After regression, the swelling eventually will recur because the underlying cause – the necrotic pulp – has not been removed. The patient will report that the “swelling comes and goes.”
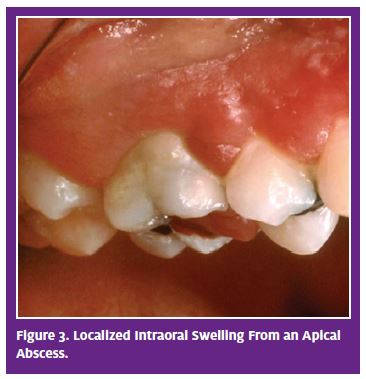
Cellulitis is uncommon, but can occur, particularly in compromised individuals. It is a rapidly spreading, facially distorting swelling, suggesting (though undemonstrated) that bacteria are no longer confined to the abscess and have invaded regional tissues (Figure 4). Cellulitis can result in such systemic signs as elevated temperature, lymphadenopathy, and malaise. Patients with the condition will be understandably distressed.
Cellulitis seldom leads to dangerous systemic events. If sepsis does occur (there are no reported, well-documented cases), it is very rare. The major danger is airway closure from swelling of pharyngeal spaces or in sublingual spaces (Ludwig’s angina). The source is mandibular molars. Patients who are experiencing such airway closure events will have severe swelling in the lower face and may report difficulty in breathing or swallowing. Oral examination likely will show drooping of the soft palate, displacement of the uvula, and possibly trismus (“lockjaw”). Closure of the airway requires immediate and aggressive treatment, usually hospitalization to establish an airway (intubation or tracheostomy) and intravenous administration of antibiotics.
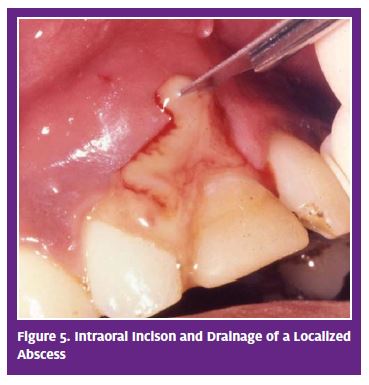
Treatment plan. For resolution, two modalities are critical: 1) removal (debridement) of the necrotic tissue and bacteria from the pulp space; and 2) drainage of the abscess. Without both, the abscess will resolve poorly, or not at all. Removal of the source of the problem can be accomplished by initiating root canal treatment or extracting the tooth. Debridement of the pulp space usually is not an option in an urgent care setting, unless managed by a dentist with appropriate instrumentation. However, when indicated, drainage alone will help relieve symptoms and result in some resolution. Drainage is implemented via either intraoral or extraoral incision. Intraoral incision of a swelling can be performed by a dentist or physician with the patient under local anesthesia. Hospitalization often is considered for patients with cellulitis who have systemic signs and symptoms.6 Management of such cases requires more aggressive treatment, usually under the care of an oral surgeon.
Pain control. This is primarily accomplished with local anesthesia, and if convenient, by incision for drainage to relieve pressure, supplemented by analgesics. Local anesthesia and oral analgesia are the same as for irreversible pulpitis.
Antimicrobial control. Antibiotics have very limited application, depending on whether the abscess is localized or involves cellulitis. Clinical studies7,8 and specialty organization guidelines suggest that antibiotics are not useful and are not indicated for the localized abscess. Although there are no data as the benefit, an antibiotic is recommended for cellulitis.9 The pathogenic organisms responsible for the rapid spread through soft tissue are most likely to be gram-negative anaerobic streptococci. Empirically, the preferred antibiotic is potassium penicillin-allergic patients, clindamycin, 300 mg qid is the next choice.
9
Follow-up. The patient should be instructed to seek dental care as soon as possible. Root canal treatment is required if the tooth is to be saved, otherwise, extraction is necessary.
Pericoronitis
Pathosis. Pericoronitis is a localized abscess associated with a partially erupted tooth; nearly all occurrences involve mandibular third molars (wisdom teeth) that have insufficient space for complete eruption. A remnant of gingival tissue (operculum) partially overlays the tooth surface and becomes traumatized by the maxillary molars during chewing or closing. Bacterial plaque and other debris invade this space and cause further injury.10
Clinical presentation and diagnosis. Pericoronitis is a painful, localized, angry, fluctuant swelling surrounding the third molar (Figure 6). Edema of the adjacent cheek often occurs. (Note: Because of the region of the extraoral swelling and pain, this condition is often mistaken for parotitis). The patient may exhibit trismus and lymphadenopathy of the submandibular and cervical nodes. Pressing on the swollen tissues often produces purulence from under the flap. Systemic signs, such as elevated temperature or malaise, seldom are present. Rarely with this condition progress to more serious manifestations such as peritonsillar abscess or cellulitis.
Treatment. In an urgent care setting, at a minimum, after infiltration with local anesthetic, the space under the flap should be irrigated with normal saline to reduce plaque and debris. The patient should be instructed to rinse with hot salt water (1 tsp in a cup of water as hot as can be tolerated).
Pain control. Local anesthetics and over-the-counter (OTC) analgesics should be administered.
Antimicrobials. Antibiotics are not indicated unless there are significant systemic signs and/or cellulitis. If so, penicillin would be the medication of choice, as previously recommended for cellulitis.
Follow-up. The only definitive treatment is extraction, which should be performed as soon as is feasible for the patient and the dentist. If the offending tooth is not removed, the abscess will continue to form repeatedly.
Acute Necrotizing Ulcerative Gingivitis
Patients occasionally present to emergency departments with various periodontal diseases.11 The most dramatic of these is acute necrotizing ulcerative gingivitis (ANUG). Most emergency periodontal problems can be managed as described below for ANUG, that is, with debridement and lavage.
Pathosis. During World War I, ANUG was known as “trenchmouth” because it was common in soldiers who spent long, stressful periods in battlefield trenches and often had poor nutrition and no oral hygiene. ANUG results from impaired host response. Causative factors can include inadequate sleep, poor nutrition, tobacco use, AIDS, and psychological stress. The overriding etiology is poor oral hygiene, resulting in gross plaque accumulation. Spirochetes and other bacteria abound in the necrotic gingival tissue.12
Clinical presentation and diagnosis. The most obvious and immediate finding is a strong, fetid malodor, which may be detectable from across the room. Intraoral findings are readily apparent and include gingival inflammation, with beet-red, swollen tissues at the margins of the teeth and a gray, pseudomembranous slough of gingiva, particularly of the interdental papillae (Figure 7). A patient with ANUG will report constant radiating, gnawing pain with a foul taste. Systemic complications are infrequent.
Treatment. Systemic signs, such as elevated temperature, malaise, and lymphadenopathy, should be evaluated. Although ANUG is unpleasant, these patients do not necessarily require immediate treatment in an urgent care setting. Treatment can be delayed until a patient can see a dentist, preferably as soon as is convenient. If the decision is made to render treatment, topical anesthetic can be applied to the inflamed tissues. After several minutes, gently swab the gray pseudomembrane and remove it with moistened cotton swabs or pellets to reduce irritants and the microbial load. Hemorrhage will be copious. Use each pallet in a limited area and then discard it. Then rinse with warm water or saline.
Instruct the patient to avoid alcohol and tobacco and to rinse with 3% hydrogen peroxide every 2 hours. Rest is required. Brushing can be done gently with an ultrasoft brush and also flossing, if it is not too painful. The patient must be informed that the tissues will bleed readily.
Pain medication. Conventional OTC analgesics, usually NSAIDs or acetaminophen, are appropriate for pain management. Narcotics usually are not needed. Antimicrobials. Antibiotics are of no benefit for ANUG, unless systemic signs and symptoms are significant, which is unlikely. With systemic signs, the choice is amoxicillin, 1000 mg stat, then 500 mg every 6 hours for 7 days.9
Follow-up. Patients with ANUG should be encouraged to follow up with a dentist as soon as possible. The dentist will completely remove the local irritants and perform prophylaxis (thorough cleaning) and instruct the patient in appropriate oral hygiene measures.
Conclusion
Dental emergencies are an emerging chief complaint for patients presenting in an urgent care setting. A systematic approach that includes a good physical exam of the gums, teeth, and throat; a correct diagnosis; and proper treatment plan can provide pain relief and avoid further complications. The treatment protocol for such emergencies usually ends in a dental referral, which is often not feasible on weekends and evenings. The goals of treatment in the urgent care setting are to relive pain, and occasionally, swelling, and to educate the patient on home management and the importance of seeking dental care as soon as possible. Some urgent care providers may want to consider seeking further training in dental emergency procedures to meet the increasing need for after-hours dental care.
References
- Lewis C, Lynch H, Johnston B. Dental complaints in emergency departments a national perspective. Ann Emerg Med. 2003; 42(1): 93-99.
- Nalliah RP, Allareddy V, Elangovan S, et al. Hospital emergency department visits attributed to pulpal and periapical disease in the United States in 2006. J Endod. 2011; 37(1): 6-9.
- Portman-Lewis S. An analysis of the out-of-hours demand and treatment provided by a general dental practice rota over a five-year period. Prim Dent Care. 2007; 14(3): 98-104.
- Keenan JV, Farman AG, Fedorowicz Z, Newton JT. A Cochrane systematic review finds no evidence to support the use of antibiotics for pain relief in irreversible pulpitis. J Endod. 2006; 32(2): 87-92.
- Campanelli CA, Walton RE, Williamson AE, et al. Vital signs of the emergency patient with pulpal necrosis and localized acute apical abscess. J Endod. 2008; 34(3): 264-267.
- Kim MK, Nalliah RP, Lee MK, Allareddy V. Factors associated with length of stay and hospital changes for patients hospitalized with mouth cellulitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Mar 31.
- Fouad AF, Rivera EM, Walton RE. Penicillin as a supplement in resolving the localized acute apical abscess. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 81(5): 590-595.
- Matthews DC, Sutherland S, Basrani B. Emergency management of acute apical abscesses in the permanent dentition: a systemic review of the literature. J Can Dent Assoc. 2002; 69(10): 660.
- American Association of Endodontists Guidelines. Colleagues in Excellence, Publications and Research Web page. http://www.aae.org/guidelines. Accessed April 2, 2012.
- klokkevoid PR, Newman MG, Carranza FA, Takei HH. Carranza’s clinical periodontology. 12th ed. St. Louis, MO: Saunders Elsevier. Chapter 41: Treatment of Acute Gingival Disease pp 440-441.
- Elangovan S, Nalliah R, Allareddy V, Karimbux NY. Outcomes in patients visiting hospital emergency departments in the United States because of periodontal conditions. J Periodontal. 2011; 82: 809-819.
- Klokkevoid PR, Newman MG, Carranza FA, Takei HH. Carranza’s clinical periodontology. 12th ed. St. Louis, MO: Suanders Elsevier. Chapter 41: Treatment of Acute Gingival Disease. pp 437-440.