Urgent Message: Fever plus back pain should alert a provider to a potentially serious condition that warrants further workup.
ERICA MARSHBURN, BS, BA, and JOHN SHUFELDT, MD, JD, MBA, FACEP
Many high-risk conditions can present as back pain and back pain is a very frequent presenting complaint in urgent care medicine. When the back pain is associated with fever of unknown etiology or if it occurs in someone with a history of receiving intravenous (IV) medicine or in an IV drug abuser, consider epidural abscess as a high-risk rule out.
Case Presentation
A 36-year-old employed mother of two presents with a complaint of back pain radiating around her side to her chest and a low-grade fever over the last 2 days. She was recently discharged from the hospital after a stay in the intensive care unit for a closed head injury resulting from a motor vehicle accident.
Pertinent Physical Exam
The patient’s pulse is 115, blood pressure 160/94, respiratory rate 18, and temperature 39.5°C. On exam, she has some mild tenderness over the lower thoracic spine. Extensor plantar responses are positive and lower extremity strength is RLE (right lower extremity) 4/5, LLE (left lower extremity) 4+5/ Deep tendon reflex is +4 or hyperactive with clonus. The rest of the patient’s exam, other than her vital signs and deep tendon reflexes, is completely normal.
Labs/Imaging
Laboratory:
CBC: WBC 17,500 with a left shift.
I-stat: Lytes, BUN and creatinine are normal.
Urine: Normal
Blood Cultures: Sent to lab, pending
ESR: 36
C-reactive protein: Elevated
The complete blood count reveals leukocytosis, which is present in about two-thirds of patients with spinal epidural abscess. Blood cultures are positive in 60% of cases and erythrocyte sedimentation rate (ESR) may be highly elevated in cases of spinal epidural abscess. Leukocytosis and ESR elevation are nonspecific laboratory findings and are not the degree of laboratory abnormality is specific for spinal epidural abscess.
Lumbar puncture is relatively contraindicated if spinal epidural abscess is suspected because of the risk of introducing purulent material into the subarachnoid space. However, lumbar puncture (LP) done under fluoroscopy may be essential to exclude meningitis from the differential diagnosis.
Imaging:
Immediate imaging of the spine and spinal cord is imperative when a diagnosis of spinal epidural abscess is suspected based on clinical findings. Such patients should be transferred to the emergency department for further imaging and admission. Magnetic resonance imaging (MRI) with and without gadolinium is the modality of choice because it has the greatest diagnostic accuracy and affords much more better differentiation of soft tissue densities than does computed tomography (CT) imaging.
If MRI is unavailable, CT myelography can reveal a spinal epidural abscess. CT scan is inadequate, however, for showing soft tissue structures adequately. Conventional myelography also can be used, but may underestimate the size of the abscess and like LP, risks contaminating the entire spinal cord.
The only possible value of plain films would be if osteomyelitis were suspected initially or with any injury to the lumbar spine. Plain radiographs are never sufficient to establish a diagnosis of spinal epidural abscess.
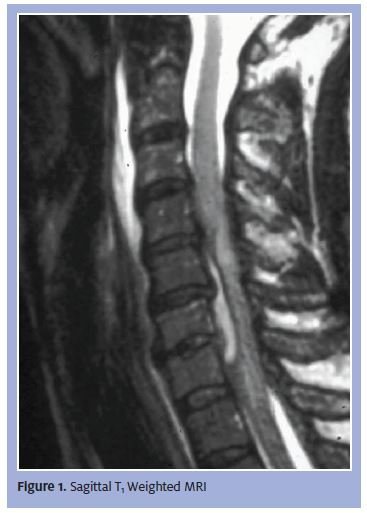
This patient’s epidural abscess is causing a transverse myelopathy, requiring surgical decompression (Figure 1). The spinal cord is also vulnerable to encroachment by benign/malignant tumors, infectious disease of the bony vertebra and disk spaces, stenosis of the neural foramen, vascular malformations with and without bleeding, and posterior herniation of disc material.
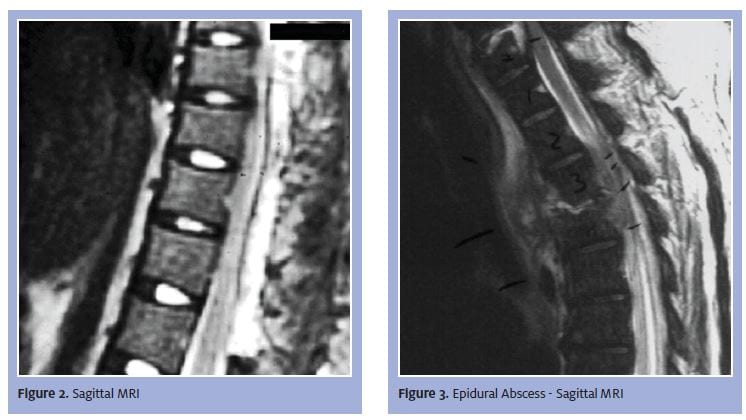
Depending on the type of images generated (T1 or T2 weighted), spinal fluid may be seen as a bright or dark signal. In Figure 2, starting at the low levels, we can follow the spinal cord upward. The spinal fluid appears white. At the level of the pathology the dura, spinal cord, and epidural abscess are all clearly seen.
The sagittal view in Figure 3, of the same disease process, shows fluid collection and the cord as two separate densities. Looking at the sagittal MRI at the level of the pathology, we can clearly see a density difference between the abscess and the spinal cord.
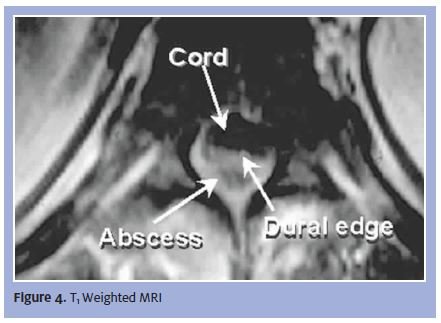
An axial rather than sagittal reconstruction above the level of the abscess shows a normal spinal cord, vertebral body, and posterior elements (Figure 4). A large epidural abscess is impinging upon the spinal cord, which is diagnostic for an epidural empyema. With an axial scan sequence, we can see the difference between the cord and the fluid collection compressing the cord and jeopardizing spinal cord function.
Diagnosis
A spinal epidural abscess is a rare, but potentially fatal, condition that requires early detection and proper management to optimize neurological outcomes. Spinal epidural abscess is an infectious process usually confined to the adipose tissue of the posterior epidural space, where there is a rich venous plexus. Major risk factors include diabetes, intravenous (IV) drug abuse, chronic renal failure, alcoholism, and immunosuppression.
Presentation begins with backache that progresses to localized back pain associated with tenderness to percussion. Fever, sweats, and rigors are common (30% – 75% of cases), and marrow edema in facet articular processes and adjacent laminae are often seen. Table 1 lists differential diagnosis that should be considered.
Table 1. Differential Diagnosis of Spinal Epidural Abscess |
|
| Arteriovenous malformations | Metastatic disease of the spine and related structures |
| Brain abscess | Multiple sclerosis |
| Cervical spondylosis | Psoas abscess |
| Diskitis | Spinal cord hemorrhage |
| Endocarditis | Spinal cord infarction |
| Epidural hematoma | Tropical myeloneuropathies |
| Herniated nucleus pulposus | Vertebral osteomyelitis |
| HIV-1-assocaited vacuolar myelopathy | Vitamin B12-associated neurological diseases |
Course and Treatment
Treatment most often consists of both medical and surgical therapy. Emergent surgical consultation should be sought for decompression and drainage of purulent material. Blood and abscess culture results guide definitive medical therapy. Antibiotic treatment with CT-guided aspiration of the epidural space is increasingly used in patients who are at prohibitively high risk of surgery or who have a presumably irreversible fixed paralysis. Successful treatment with a combination of abscess aspiration and antibiotic treatment has been reported and its use seems to be increasing. Resolution of the abscess with antibiotics alone has been reported in patients who are not candidates for surgery because of spine instability or coexisting medical problems. Deterioration of clinical and functional status while undergoing antibiotic therapy alone has been observed and may dictate emergent surgical decompression.
Empiric antibiotic coverage should include antistaphylococcal antibiotics. With the increasing incidence of methicillin-resistant staphylococcus (MRSA) infections, coverage that includes antibiotics effective against MRSA is recommended. If a patient remains neurologically stable and has a mechanically stable spine, some clinicians recommend that antibiotic treatment be delayed until material is obtained for a culture. Coverage should be tailored if culture data are available or if a suspected precursor to the infection is established.
If a patient’s infection follows a neurosurgical procedure, an antistaphylococcal penicillin, a third-generation cephalosporin, and an aminoglycoside should be prescribed in combination. Patients with spinal epidural abscess may be clinically unstable because of concomitant systemic infection, shock, complications of diabetes mellitus, or other complications. As a result, the increased surgical risk often must be weighed against the risk of using antibiotic therapy alone.
Discussion
Most symptoms of spinal epidural abscess are a result of enlargement of the abscess and inflammation in the surrounding area, which leads to tissue compression and ischemia of the spinal cord. Most cases of spinal epidural abscess are caused by Staphylococcus aureus, but a range of other bacteria can also bring about infection.
Clinical presentation can be quite variable. The clinical triad of fever, back pain, and neurologic defect is not present in most patients, and should not be relied upon for diagnosis. Early presentations may be subtle, and atypical presentations are not unusual. Reflexes may vary from absent to hyperreflexia with clonus and extensor plantar (Babinski) responses. Areflexia may indicate spinal shock with transient inhibition of spinal reflexes. Nuchal stiffness or rigidity may be present, most notable with cervical epidural abscesses. Ten percent of patients with spinal epidural abscess present with encephalopathy.
A four-phase sequential evolution has been described in the literature: 1. Localized spinal pain, tenderness, and possibly fever; 2. Radicular pain and reflex abnormalities; 3. Muscular weakness, sensory loss, and sphincter dysfunction; and 4. Paralysis.
The virulence of the infecting organism and the mode of infection contribute to the tempo of this progression. Hematogenous abscesses tend to progress rapidly, whereas abscesses from osteomyelitis or discitis may evolve over weeks or months with a slower progression of symptoms. Localized back pain often is the first symptom and patients frequently give a history of back strain or mild injury. A source of infection in skin or soft tissue also may be found, and radiculopathy with radiating or lancinating pain, including chest or abdominal pain, is a common symptom.
IV drug users are a high-risk group for spinal epidural abscess, and even patients with a remote history of IV drug abuse are at risk. Cases are frequently reported in patients with spinal trauma, alcoholism, conditions involving chronic immunosuppression, and diabetes mellitus, a risk factor in 50% of reported patients. Hematogenous IV lines, urinary catheters, or implantable devices.
Epidural abscesses at the level of the cauda equine cause symptoms consistent with cauda equine syndrome rather than a spinal cord syndrome, and can involve paraparesis with prospective progression to a paraplegia as well as sphincter dysfunction, including incontinence or increased residual urine volumes. Central cord syndrome from epidural abscess also has been reported and is marked by disproportionate impairment of motor function in the upper extremities compared with the lower ones.
Physical findings vary with the degree of spinal cord compression or dysfunction. In the most advanced cases, a transverse cord syndrome is seen with motor and sensory levels found with neurologic examination. Localized tenderness to percussion or palpation at the site of the abscess may be noted. Paraspinal muscle spasm also may be present.
Most cases of spinal epidural abscess arise from hematogenous seeding of the epidural space from a distant source of infection, but a few cases are the result of direct extension of infection from the spine or paraspinal tissues. Common sources of infection are listed in Table 2.
Table 2. Common Sources of Spine or Paraspinal Tissue Infection |
Hematogenous infection of skin and soft tissue
Contiguous spread
|