Urgent Message: Better understanding of tympanic membrane/middle ear conditions can inform more accurate diagnoses at the point of care.
Citation: LaCour J. Tympanic Membrane Conditions Beyond Otitis Media in Urgent Care Practice. J Urgent Care Med. 2023;18(3):15-19
Author Affiliation: Jeff LaCour, MD, Compassio Medical Education.
Video: Watch a video featuring Jeff LaCour, MD, that further explains tympanic membrane conditions with supplemental images. WATCH VIDEO
Urgent care providers are often tasked to determine the source of a patient’s otalgia, muffled hearing, or ear fullness. Unfortunately, general medical education and training regarding normal and abnormal conditions of the tympanic membrane (TM) and the middle ear is often inadequate for appropriate risk stratification of many conditions affecting the TM. In one study, pediatricians averaged 50% incorrect responses when distinguishing between acute otitis media, serous otitis media, and a normal tympanic membrane.1
In this article, we will review the normal anatomy of the tympanic membrane as well as common tympanic membrane/middle ear conditions urgent care (UC) providers are most likely to encounter.
Anatomy
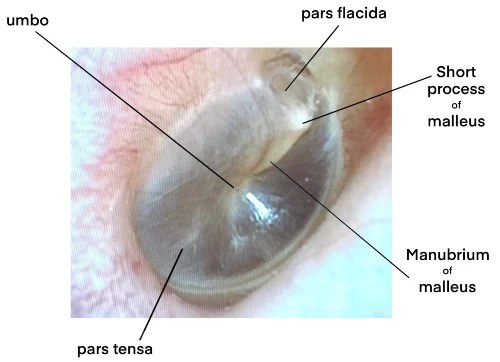
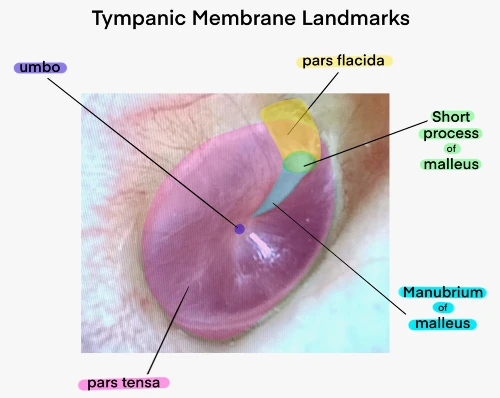
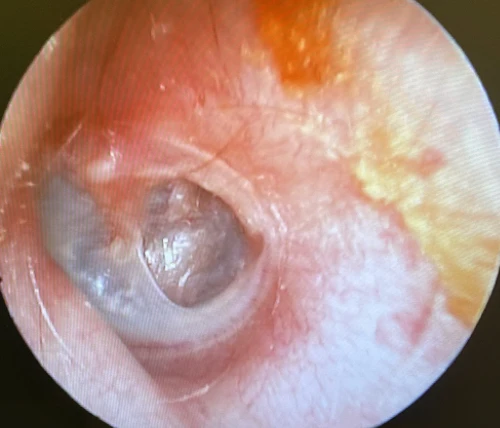
The TM is a mere 0.1 mm thick with a diameter of approximately 1 cm. It is composed of three layers, with the fibrous stratum or lamina propria (the middle layer) providing its stability. The lateral layer is stratified keratinizing epithelium, and the inner/medial layer is cuboidal mucosal epithelium. The majority of the TM is the pars tensa, which should appear transparent on a normal exam. The pars flacida is above the short process of the malleus and is less taut due to its absence of the fibrous layer. The umbo attaches to the inferior aspect of the malleus manubrium and is the most depressed portion of the TM (Figure 1, 2).2
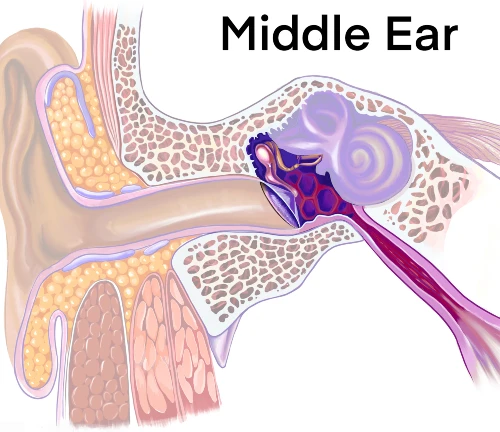
The middle ear space consists of the malleus, incus, and stapes. The middle ear space is connected to the nasopharynx via the eustachian tube (ET). (Figure 3). A patent ET serves the vital function of pressure equalization between the nasopharynx and middle ear.
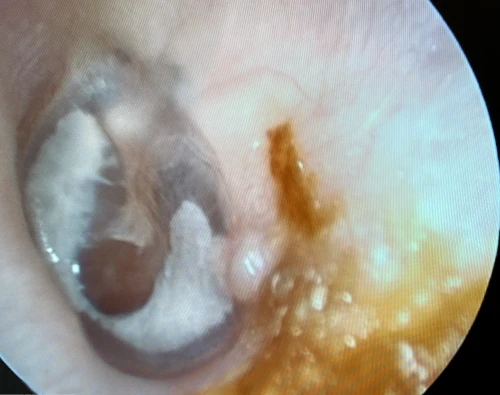
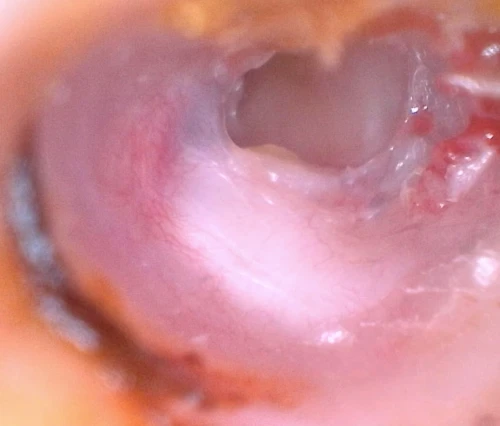
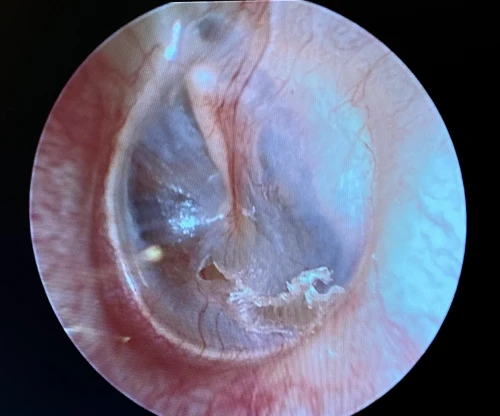
Tympanosclerosis/Myringosclerosis
Tympanosclerosis is a post-inflammatory calcification of the collagen containing structures in the middle ear. In 90% of patients, it will manifest as visible white plaques of the TM, a condition known as myringosclerosis (Figure 4, 5). The condition is common in patients with a history of pressure equalization tubes (PE tubes), chronic otitis media with effusion, and recurrent acute otitis media.3,4 This can be mistaken for cholesteatoma or sometimes gives the appearance of bubbles or fluid in the middle ear (Figure 6, 7). In patients with more extensive myringosclerois, the normal translucent aspects of the TM may appear like a perforation (Figure 8, 9). A type A tympanogram or a mobile TM on pneumatic otoscopy can help rule out a TM perforation or middle ear effusion. Myringosclerosis does not typically cause hearing loss, and an ENT referral should be reserved only for patients complaining of hearing loss in the affected ear.




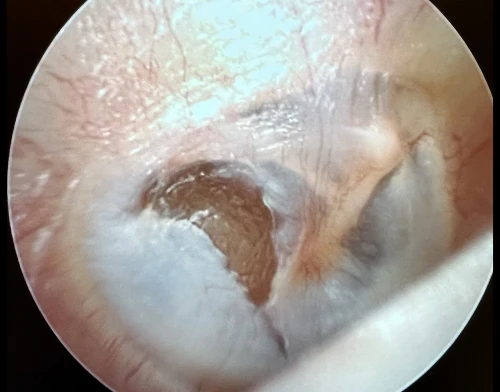

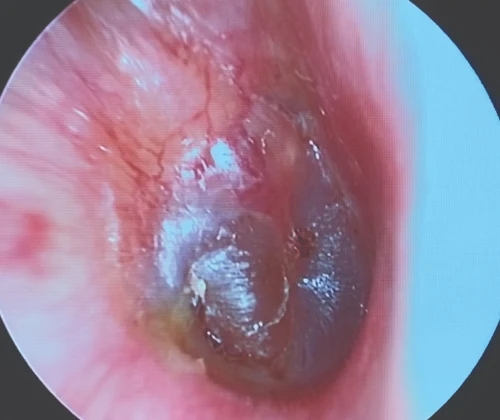
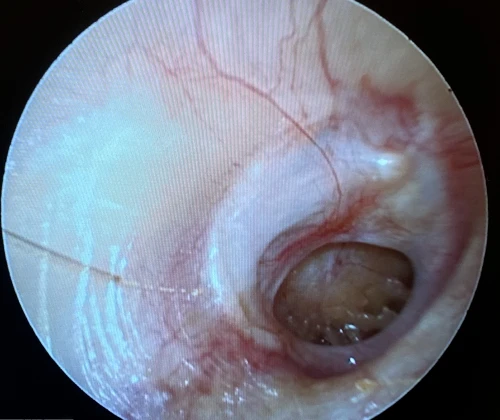
Cholesteatoma
A cholesteatoma is a locally invasive, non-neoplastic lesion of the temporal bone. It occurs when the epidermis of the external ear canal migrates into the middle ear space.5, 6 There are two types of cholesteatomata: congenital, which is unique to childhood; and acquired, affecting both adults and children.7 The congenital type is located medial to an intact tympanic membrane, while an acquired type commonly forms from a retraction pocket located in the pars flaccida TM or the posterior superior aspect of the pars tensa TM (Figure 13, 16).5 An acquired type can also originate from epithelial migration into the middle ear through a TM perforation (Figure 14).8
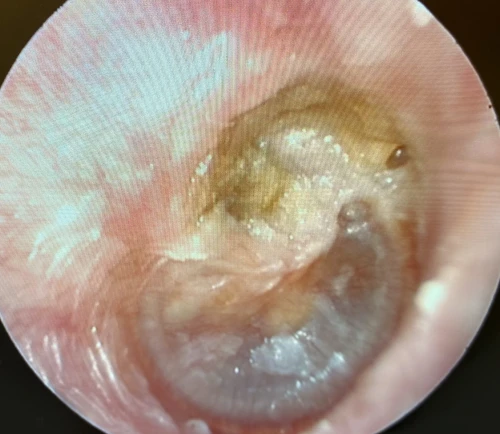

If left undetected and untreated, a cholesteatoma can lead to hearing loss, temporal bone destruction, and intracranial invasion (Figure 15). Cholesteatomata typically appear as cystic structures with a pearly white appearance. The most frequent symptom of a cholesteatoma is foul smelling otorrhea (65% of cases), which can be persistent or intermittent in nature. Other symptoms include otalgia and hearing loss from erosion of the malleus, incus, or stapes.5

The incidence of cholesteatomata is higher in children and is upwards of 9 per 100,000 people in developed countries.9 Any patient with the possibility of a cholesteatoma warrants an ENT referral within 6 weeks. Although rarely urgent, surgical removal is the treatment of choice.
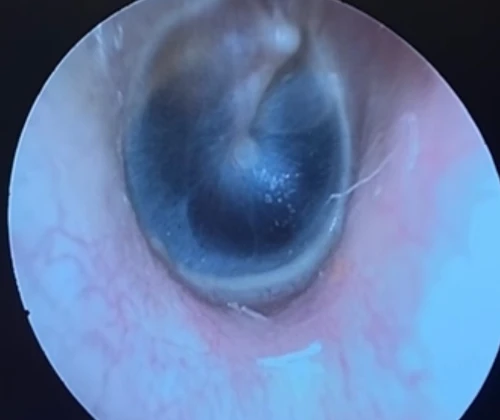
Otitis Media with Effusion
Otitis media with effusion (OME) is the presence of fluid in the middle ear, in contrast to otitis media, which is the presence of purulence in the middle ear. OME is extremely common in childhood affecting 90% of children prior to starting school. The horizontal plane and short length of a child’s eustachian tube impair middle ear ventilation, which is a precursor to OME. Oral antibiotics and oral steroids are not recommended for OME as most cases resolve spontaneously.10
Children that are considered higher risk (eg, pre-existing hearing loss, speech delay, autism, Down syndrome/craniofacial disorders, visual impairment, cleft palate, developmental delay) should be referred for hearing test as this population could be disproportionately affected by hearing loss.10 OME is often misdiagnosed as acute otitis media (AOM) leading to unnecessary oral antibiotics.¹ Becoming more familiar with otoscopic findings of OME versus AOM will help limit this error (Figures 17-26). Although unable to distinguish between AOM and OME, the use of tympanometry is highly accurate for confirming a normal middle ear (type A tympanogram) versus fluid or purulence in the middle ear (type B flat tympanogram).10
Adult-onset OME (AOOME) is less prevalent and is not as universally benign. Even though sinusitis is the most common causal factor of AOOME, the association between AOOME and nasopharyngeal carcinoma (NPC) is well established.11 Therefore, when AOOME is identified in adult patients, ENT referral is indicated within 3 weeks, as many of these patients will have findings of significance on nasal endoscopy. In a series of 167 patients with AOOME, head and neck tumors (mainly NPC) were found in a staggering 4.8% of patients. In the same study, 66% of patients had ethmoid sinus disease, and 19% had nasopharyngeal or lymphoid hyperplasia.12







Tympanic Membrane Perforations
A tympanic membrane perforation (TMP) is most commonly the result of trauma or an episode of AOM with spontaneous TM rupture. A TMP following AOM generally resolves following control of the infection.13 ENT referral should be reserved for adult cases only. Pediatric cases should follow up with the primary pediatric provider to assure closure of the hole. Traumatic TMP are most commonly caused by instrumentation, principally by self-hygiene with cotton-tipped applicators. Other causes of traumatic TMP include water trauma (during diving or waterskiing), strikes to the head, blast injuries, and falls.14
Some 78-97% of traumatic TMP will heal spontaneously without surgical intervention. Systemic antibiotics are not necessary for these patients, but otic antibiotic drops (eg, ofloxacin) are recommended if otorrhea is present. Aminoglycoside-containing drops (eg, neomycin, tobramycin) should be avoided for TMPs due to their ototoxicity (hearing loss and balance problems) if introduced into the middle ear. Dry ear precautions and avoidance of swimming/submersion should be initiated. Patients with traumatic perforations of the TM are advised to have a follow up with an ENT provider within 2 weeks to assess hearing and confirm closure of TMP (Figures 27-29).

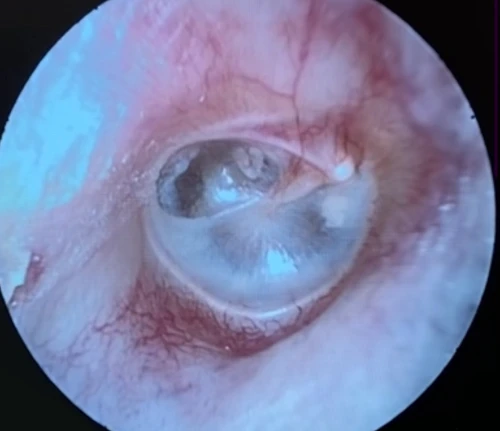
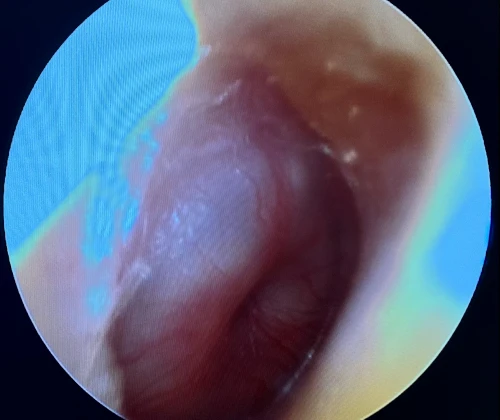
Tympanic Membrane Retraction Pockets
A retraction pocket (RP) of the tympanic membrane is a localized area of the TM invaginated into the middle ear space. RPs are common in children, with a prevalence of roughly 10%; the prevalence in adults is largely unknown.15 The most common sites of RPs are the pars flaccida and the posterior superior aspects of the TM (Figure 10, 11, 12).16 The main etiological factor is negative middle ear pressure caused by eustachian tube dysfunction (ETD) and middle ear inflammation.17,18 Suspicion of a retracted TM can be confirmed via tympanogram demonstrating negative middle ear pressure (type C tympanogram). Patients with retracted TMs should be referred to an ENT provider within 3 months for surveillance, possible pressure equalization tube, or surgery.
Discussion
For many patients with acute or subacute ear complaints, UC centers are the most likely destination for initial presentation. UC clinicians, therefore, should have a comprehensive understanding of these various conditions potentially encountered during otoscopy. Additionally, knowledge of the initial treatment for each condition and indications for ENT referral when TM pathology is encountered are critical for avoiding both unnecessary referrals and for mitigating the risk of long-term sequelae of potentially serious middle ear conditions.
Manuscript submitted June 30, 2023; accepted October 26, 2023.
References
- Pichichero ME., Poole MD. Assisting Diagnostic Accuracy and Tympanocentesis. Skills in the Management of Otitis Media. Arch Pediatr Adolesc Med. 2001; 155(10): 1137-1142
- Luers JC, Hüttenbrink KB. Surgical Anatomy and Pathology of the Middle Ear. Journal of Anatomy 2016; Feb; 228(2): 338-353
- Kay DJ, Nelson M, Rosenfeld RM. Meta-analysis of tympanostomy tube sequelae. Otolaryngology Head Neck Surg. 2001. April; 124 (4): 374-380
- Daly KA, Hunter L, Lindgren B. Chronic Otitis Media with Effusion: Sequelae in Children Treated with Tubes. Arch Otolaryngol Head Neck Surg. 2003; 129(5):517-522.
- Castle JT. Cholesteatoma Pearls: Practical Points and Update. Head Neck Pathol. 2018 Sep; 12(3):419-429
- Soldate D, Mudry A. Knowledge about cholesteatoma, from the first description to the modern histopathology. Otol Neurotol. 2001 Nov;22(6): 723-730
- Kuo C, An-Suey S, Yung M, Sakagami M, Sudhoff H, Wang C, Hsu C, Lien C. Updates and Knowledge Gaps in Cholesteatoma Research. Biomed Res Int. 2015:854024
- Semaan MT, Megerian CA. The pathophysiology of cholesteatoma. Otolaryngologic Clinics of North America. 2006;39(6):1143-1159
- Bonnard A, Berglin CE, Wincent J, Erikson PO, Westman E, Feychting M, Mogensen H. The Risk of Cholesteatoma in Individuals with first degree relatives surgically treated for the disease. JAMA Otolaryngol Head Neck Surg. 2023; 149(5):390-396
- Rosenfeld RM, Shin JS, Schwartz SR, Coggins R, et al. Clinical Practice Guideline: Otitis Media with Effusion (Update). Otolaryngology – Head and Neck Surgery 2016, Vol. 154, S1-S41
- Mills R, Hathorn I. Aetiology and pathology of otitis media with effusion in adult life. The Journal of Laryngology & Otology. 2016. 130, 418-424
- Finkelstein Y, Ophir D, Talmi YP, Shabtai A, Strauss M, Zohar Y. Adult-onset otitis media with effusion. Arch Otolaryngol Head Neck Surg 1994; 120: 517-27
- Principi N, Marchisio P, Rosazza C, Sciarrabba CS, Esposito S. Acute otitis media with spontaneous tympanic membrane perforation. Eur J Clin Microbiol Infect Dis. 2017 Jan. 36(1):11-8
- Carniol E, Bresler A, Shaigany K, Svider P, Baredes S, Eloy JA, Ying YL. Traumatic tympanic membrane perforations diagnosed in emergency departments. JAMA Otolaryngol Head Neck Surg. 2018 Feb; 144(2): 136-139
- Bayoumy AB, Veugen C, Rijssen LB, Yung M, Bok, J-WM. The natural Course of Tympanic Membrane Retractions in the Posterosuperior Quadrant of Pars Tensa: A watchful Waiting Policy. Otol Neurotol. 2021 Jan; 42(1): e50-e59
- Parab SR, Khan MM. Endoscopic Management of Tympanic Membrane Retraction Pockets: A Two-Handed Technique with Endoscope Holder. Indian J Otolaryngol Head Neck Surg. 2019 Dec; 71(4): 504-511
- Danner CJ. Middle ear atelectasis: What causes it and how is it corrected? Otolaryngol Clin North Am 2006; 39:1211-1219
- Ruah CB, Schachern PA, Paparella MM, Zelterman D. Mechanisms of retraction pocket formation in the pediatric tympanic membrane. Arch Otolaryngol Head Neck Surg 1992; 118: 1298-1305
Click Here to download the article PDF
