Urgent message: Patients who present after exposure to tuberculosis test the clinician’s ability to assimilate broad and generalized information, including a unique set of historical, clinical, and laboratory data required to customize appropriate, patient-specific assessment and treatment plans.
By Jacqualine Dancy, PA-C, MPAS
Not long after I contributed the article Tuberculosis Screening in Urgent Care Medicine (JUCM, July/August 2010), our urgent care clinic was faced with the exposure to tuberculosis of numerous employees at a large local institution. What had been theory and a situation we had been trained for but not encountered on such a scale became a real-life challenge.
When an occupational exposure occurs, urgent care clinics—especially those that provide occupational medicine services—are likely to be the primary care providers. Such patients are likely to be workers in higher-risk employment including, but not limited to, healthcare centers, correctional facilities, and other institutions that provide housing.
Post-exposure testing differs from tuberculosis screening in that these patients have had an exposure to someone with active tuberculosis and require monitoring and treatment considerations. Monitoring and surveying of the general public and employees occurs in a number of healthcare venues, including public health clinics, employee health clinics, and private medical offices.
To customize appropriate testing and monitoring recommendations, one first needs to evaluate the significance of the exposure. This requires assessment of how close the contact was regarding droplet exposure and the duration exposure. It is helpful if the source’s illness profile if available. Furthermore, one needs to assimilate this information with the patient’s pertinent medical history.
Ascertaining the contagiousness of the source is helpful. For example, understanding that tuberculosis bacteria are spread via droplets, we should consider an actively coughing source very contagious. Identifying the sensitivity profile of the source’s TB infection will aid in the treatment plan.
The type and duration of exposure is relevant in determining the level of risk and to aid in the interpretation of intradermal (tuberculin skin tests, or TSTs) and/or serological (Interferon Gamma Release Assays, or IGRAs) test results and in developing a working plan. Knowledge of the patient’s past medical history is essential in creating a patient-specific plan. Following are points to be discussed with the exposed patient:
1. Birthplace and immunization history, specifically the Bacille Calmette-Guerin (BCG) vaccine; BCG vaccine may interfere with tuberculin skin test accuracy.
2. Past exposures to TB and/or past treatment for latent tuberculosis infection (LTBI); once a patient has been previously exposed to TB and/or received treatment for LTBI, the IGRA testing is less clinically reliable.
3. Underlying comorbid conditions that are immunosuppressive; Not limited to, but including HIV infection, cancer, diabetes, malnutrition, organ transplant recipient status, chemotherapeutically treated rheumatological and/or dermatological conditions and advanced age, to name a few. These chronic conditions impact the accuracy of tuberculin skin testing. TSTs rely on an immune response to the PPD cocktail; when patients are immunosuppressed, there may be no immune response, therefore manifesting a false-negative TST result.
4. Immunosuppressive chemotherapeutics; there is an increasing array of immunosuppressive medications in use, such as steroids, TNF-alpha inhibitors, antiretrovirals, and many cancer-specific compounds.
Testing Options
Tuberculin skin tests
Before 2001, TSTs were the only test available for detecting LTBI, and certainly continues to be the most common screening test used.(1)
There are, however, limiting factors that need to be considered. The purified protein derivative is a polyvalent antigenic mixture, a cocktail containing multiple antigens that can cause a positive response in persons previously vaccinated with BCG and/or exposed to non-tuberculosis mycobacterium. Furthermore, TST can trigger an anamnestic response (boosting phenomenon), and underlying dermatological conditions can produce a false positive result.(2) This test also depends on the accuracy of placement and window time of interpretation. The CDC reports a 78% sensitivity for TST.(1)
Interferon gamma release assays—serological testing
There are currently two tests widely used, the T-SPOT.TB test (T-Spot) and the QuantiFERON-TB Gold (QFT-G), of which the newer QuantiFERON-TB Gold In-Tube test (QFT-GIT) is available. These tests measure the gamma interferon produced by T-cells from whole or peripheral (T-Spot) blood and the response specific to M. tuberculosis proteins.(3)
The test that has been most widely discussed in the public health arena is the QuantiFERON tests. This test boasts a 98% specificity and sensitivity of at least 89%.(3) These tests report qualitative results, either positive or negative. This poses a problem, however. Non-TB exposed individuals’ interferon levels normally vary over time, which sometimes requires a quantitative result to determine clinical significance of the test result. For example, a positive QFT result of 0.4 (with positive being >0.35) in a patient with no immunological problems and who has had a very low occupational TB exposure, in whom the positive result was unexpected, requires diligent clinical assessment.
Special Considerations
The IGRA tests can be used in all circumstances in which a TST is used.(4) Immunological deficiencies affecting T-cell response may decrease the tests sensitivity and specificity.
TSTs can cause immunological elevations of interferon, and this immunological memory of a prior TST can give a false-positive result.(4) It is not well understood how close in proximity a TST may affect an IGRA result; therefore, caution is needed when the clinician chooses to use both tests simultaneously.
IGRA testing in patients previously treated for active TB or LTBI shows that in many patients their interferon levels drop and may revert their result to negative; however, in others a positive value may represent persistently elevated interferon levels after successful treatment.(1)
When to test
The current recommendation for people exposed to highly contagious active TB source is to complete testing at baseline (when the source was confirmed with active TB) and again eight to 10 weeks after exposure has ceased.(1)
Patient-specific assessment
On the initial evaluation of a patient exposed to tuberculosis, assess the patient’s exposure including type and duration.
For example, type of exposure. Was the patient a registered nurse providing direct care eight hours a day? Or a corrections officer who had no direct contact with an infected person, most often overseeing at a distance but
infrequently being in closer proximity to an infected inmate in his cell?
Another example would be duration of exposure; how long was the actively TB-infected person around others before place in isolation—hours,days, weeks, months?
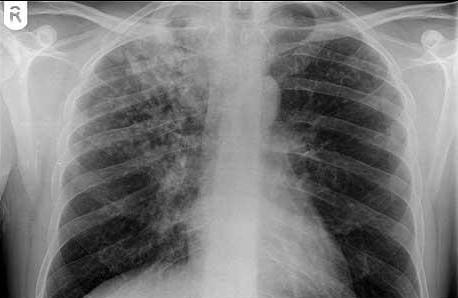
Screen the patient for any signs or symptoms suggestive of active tuberculosis, such as fever, cough (with or without hemoptysis), night sweats, and weight loss. If the patient is at least possibly symptomatic, complete a chest radiograph to assess if active TB is present.
Window Period Prophylaxis
Window period prophylaxis is indicated in severely immunocompromised persons exposed to highly contagious TB(1) where the risk for developing LTBI is significant. The immunocompromised patients must be identified, and to a certain extent the clinician must assess how immunocompromised the patient is.
Consider window-period prophylaxis in patients with HIV, cancer (especially on chemotherapeutic agents), organ transplant recipient suppressive medication, chronic steroid use, dermatological and/or rheumatological conditions on TNF-alpha inhibitors. Treatment recommendations are isoniazid (INH) 300 mg daily and vitamin B-6 25 mg daily (increase to 50 mg if paresthesia occurs).(5) Begin treatment at the initial visit and continue until the second QFT test result (eight to 10 weeks after the first) is available, then assess if it is safe to discontinue the window-period prophylaxis treatment.
Current Treatment for LTBI
It is important to understand that for a patient with a positive TST, the lifetime risk for active tuberculosis is estimated to be 5% to 10%.(2)
Current treatment recommendations from the Centers for Disease Control and Prevention for LTBI is isoniazid 5 mg/kg up to 300 mg daily for nine months. It is recommended to adjunct INH with pyridoxine (B6) 25 mg to 50 mg daily to reduce the INH side effect of paresthesias, using the lowest effective dose. The alternant antibiotic is rifampin 10 mg/kg (600 mg) daily for four to six months.
With both INH and rifampin, baseline liver function tests (LFT) are necessary. Periodic LFTs are recommended; in addition, when using rifampin, complete blood count and platelet monitoring is advised.(5)
If the source’s TB strain is a resistant pathogen, follow the sensitivities and treat appropriately.
Conclusion
Understanding the currently available testing, monitoring, and treatment options are essential to providing thoughtful consideration to patients exposed to tuberculosis. Furthermore, while there are limitations to the current data, patient specific interpretative assessment of the available data is crucial.
References
1. MMWR. Guidelines for using the QuantiFERON-TB Gold Test for detecting mycobacterium tuberculosis infection, United States. December 16, 2005/54(RR15);49-55.
2. MMWR. Guidelines for using interferon gamma release assay to detect mycobacterium tuberculosis infection, United States, 2010. June 25, 2010/59(RR05);1-25.
3. Miranda C, Tomford JW, Gordon SM. Interferon-gamma-release assays: Better than tuberculin skin testing? Cleve Clin J Med. 2010;77(9):606-611.
4. QuantiFERON In-Tube: Use of quantitative information. September 2010 City and County of San Francisco Department of Public Health: Tuberculosis Control Section. Director: L. Masae Kawamura, MD.
5. CDC Guide for Primary Health Providers: Targeted tuberculin testing and treatment of latent tuberculosis infection 2005. Available at: www.cdc.gov/tb/publications/LTBI/treatment.htm.
(Note: The recommendations and guidelines offered in this article are directed at patients 18 years and older. Among other sources, the Centers for Disease Control recommendations are a helpful resource. Given the current CDC testing parameters and management recommendations for patients exposed to tuberculosis, interpretive guidelines are helpful and are the goal this article.)
Ms. Dancy, in addition to her clinical work as a physician assistant, serves as compliance officer and clinical staff educator at Med+Stop Urgent Care Centers in San Luis Obispo, CA. She is a graduate of the University of Nebraska School of Medicine, with a specialization in urgent care medicine, and received training at the University of California–Davis School of Medicine.
