Urgent message: Concern over the potential spread of COVID-19 may (or may not) have affected the timeliness with which parents chose to present with children who had symptoms concerning for acute otitis media, thereby throwing the concept of “delayed” antibiotic prescribing into question.
Emily J. Montgomery, MD; Brian R. Lee, PhD, MPH; Amanda Montalbano, MD, MPH; Amanda Nedved, MD
Citation: Montgomery RJ, Lee BR, Montalbano A, Nedved A. Time to presentation for acute otitis media during the COVID-19 pandemic. J Urgent Care Med. 2022;16(4):31-35.
INTRODUCTION
In an era of increasing antibiotic resistance,1–3 acute otitis media (AOM) is a prime target for antibiotic stewardship efforts as the diagnosis for which antibiotics are most prescribed to children.4,5 The intervention of delayed antibiotic prescribing is a safe, cost-effective option for the treatment of eligible patients with AOM6 that could decrease unnecessary exposure to antibiotics. The 2013 American Academy of Pediatrics’ clinical practice guideline for AOM states antibiotic treatment may be delayed while the patient is observed for progression or resolution of symptoms for 48-72 hours if a patient 6–23 months of age has nonsevere unilateral AOM or a patient >24 months of age has nonsevere unilateral or bilateral AOM.4 However, immediate prescription of antibiotics for AOM is still the preferred practice among medical providers.4
The COVID-19 pandemic resulted in delayed care-seeking for severe acute pediatric diagnoses, including appendicitis,7 new-onset diabetes with diabetic ketoacidosis,8 sepsis, and malignancy.9 Families also delayed routine outpatient pediatric care, including immunizations.10 What is unknown is whether families delayed care for more common acute pediatric diagnoses like AOM during the pandemic. Postponement in seeking care effectively serves as an observation period which could affect the patient’s eligibility for delayed antibiotic prescribing by the time they are seen in a care setting.
This study compares the time of presentation for AOM to pediatric urgent care centers across the United States before and during the COVID-19. We hypothesized that there was a greater time to presentation for AOM during the pandemic with an increased percentage of patients presenting outside of the delayed antibiotic prescribing window compared with those presenting prior to the pandemic.
MATERIALS and METHODS
Study Design
We performed a retrospective secondary analysis of data collected for a national quality improvement project across 24 institutions with freestanding pediatric urgent care sites for 2 consecutive years. Data were collected from a convenience sample of pediatric urgent care physicians and advanced practice providers participating in the quality improvement project. Data were entered by the prescribing providers into an online data repository (Research Electronic Data Capture [REDCap]).11,12 The pre-pandemic time period reflected data submitted from May-November 2019 and the pandemic period was May–November 2020. We included all submitted records with a diagnosis of AOM based on ICD-10 code. Records were excluded if they had a co-diagnosis for which an antibiotic is almost always required, such as urinary tract infection or pneumonia.13 We recorded patient demographics (age, race, language, insurance) and clinical characteristics (time to presentation [duration of symptoms at the time of the encounter], associated fever, co-diagnoses, antibiotic prescription information) for each encounter.
Measures
The primary outcome measured the median time to presentation (days) for pre-pandemic encounters compared with encounters during the pandemic. We also evaluated the time to presentation for each time period by sociodemographic and clinical characteristics. A secondary outcome measure evaluated the percentage of eligible encounters for delayed antibiotic prescriptions and of those eligible encounters, what percentage received delayed antibiotic prescriptions. We considered encounters eligible for delayed antibiotic prescriptions if the patient was >24 months, symptoms had been present for <2 days, and fever was absent.
Data Analysis
We used the Wilcoxon rank-sum test to compare time to presentation between the two study periods. Pearson’s chi-square test was used to compare categorical factors. All analyses were completed using SAS (version 9.4; Cary, NC).
The Institutional Review Board at Children’s Mercy Kansas City determined this project was not human-subjects research.
RESULTS
There were 1,996 encounters that met inclusion criteria during the pre-pandemic period. We excluded 13 of these encounters for having a co-diagnosis requiring antibiotics. During the pandemic study period, 403 encounters met inclusion criteria. We excluded one encounter with a co-diagnosis requiring antibiotics from this group.
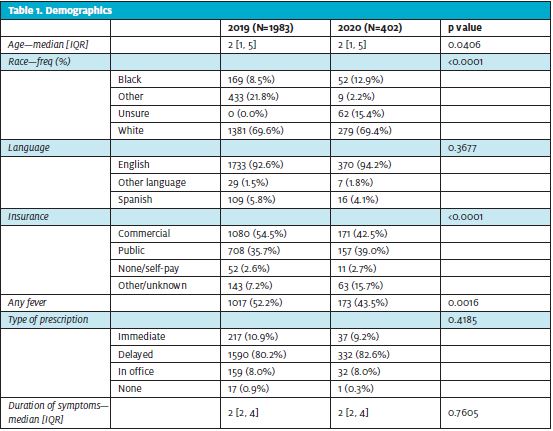
During the pandemic there was a decrease in the number of patient encounters with AOM. However, when comparing patient-level characteristics, there were some changes in the proportion of AOM encounters pre- and during-pandemic. There was an increased number of encounters in which AOM was diagnosed for black patients (p< 0.001). There was a decrease in proportion of encounters with commercial insurance (p<0.001). The clinical characteristics also showed a decrease in the proportion of encounters with associated fever (p=0.002). The median time to presentation did not change during the pandemic (2 days; IQR [2,4]) compared with pre-pandemic (2 days; IQR [2,4]) (Table 1).
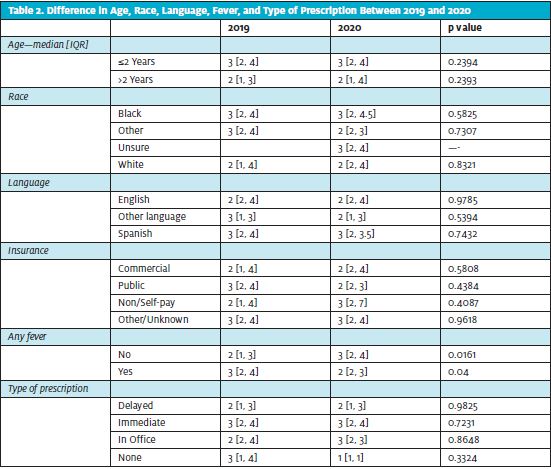
Encounters with associated fever had a shorter median time to presentation during the pandemic (2 days; IQR [2,3]) compared with pre-pandemic (3 days; IQR [2,4]); p=0.04). However, encounters with no associated fever had a longer median time to presentation during the pandemic (3 days; IQR 2,4compared to the pre-pandemic (2 days; IQR [1,3]; p=0.02) (Table 2).
The percentage of encounters eligible for delayed prescribing pre-pandemic (18.4%) compared with during the pandemic did not change (16.4%; p=0.34). Of those encounters eligible for delayed antibiotics, the rate of receiving immediate antibiotics did not change between the pre-pandemic (26.0%) and pandemic (21.2%; p=0.58).
CONCLUSIONS
In a national database of pediatric urgent care encounters, there was no difference in time to presentation for patients diagnosed with AOM before and during the COVID-19 pandemic. While other studies have reported a delay in seeking care for higher-acuity diagnoses and routine well-care, our results suggest that the common diagnosis of AOM did not see similar delays in presentation to pediatric urgent care centers.
While AOM is a low-acuity condition, it is often associated with symptoms of viral upper respiratory infections similar in presentation to COVID-19. During the pandemic, families presented for evaluation sooner when fever was associated with ear pain, possibly due to COVID-19 concerns, or conversely were more willing to watch and wait at home if their child was not having fevers in an attempt to avoid interacting with the healthcare system during the pandemic.
Given that overall patients presented in similar time frames for AOM both before and during the pandemic, it is unsurprising that the percentage of encounters eligible for delayed antibiotics also did not change. Additionally, the percentage of eligible patients who received delayed antibiotics remained low for both time periods. This practice of providing immediate antibiotic prescription for AOM rather than recommending a period of observation is consistent with previous studies.6,14–17 A multitude of provider and parental factors contribute to continued high immediate prescribing rates.14,18,19 However, many patients in our study presented after the symptoms had been present for at least 2 days, which precludes those patients from being eligible for further watchful waiting. The lack of serious complications in our study population who on average presented after 2 days of symptoms adds to the evidence that delayed prescribing is a safe treatment option for eligible patients with AOM.
LIMITATIONS
There are several limitations to this study. This was a retrospective secondary analysis of a quality improvement project database and causality of our findings cannot be identified. Our study only included patients diagnosed with AOM and we did not evaluate the time to presentation for ear pain due to other diagnoses. Although our study included patient encounters from 24 different pediatric urgent cares across the United States, our results are limited to patients treated by pediatric urgent care clinicians participating in an antibiotic stewardship project and may not be generalizable to other settings.
Despite a growing body of evidence of delayed pediatric care during the COVID-19 pandemic, there was no difference in time to presentation for patients diagnosed with AOM in a national multicenter pediatric urgent care study. However, during the pandemic, families presented sooner if there was associated fever with the ear pain. Most AOM encounters were not eligible to receive delayed antibiotics due to presentation after 2 days of symptoms, which adds to the evidence that children who present with otalgia earlier in their course can be safely monitored for at least 48 hours prior to starting antibiotics.
REFERENCES
- Vaz LE, Kleinman KP, Lakoma MD, et al. Prevalence of parental misconceptions about antibiotic use. Pediatrics. 2015;136(2):221-231.
- Song J-H, Dagan R, Klugman KP, Fritzell B. The relationship between pneumococcal serotypes and antibiotic resistance. Vaccine. 2012;30(17):2728-2737.
- Dagan R, Barkai G, Leibovitz E, et al. Will reduction of antibiotic use reduce antibiotic resistance? The pneumococcus paradigm. Pediatr Infect Disease J. 2006;25(10):981-986.
- Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964-e999.
- Vaz LE, Kleinman KP, Raebel MA, et al. Recent trends in outpatient antibiotic use in children. Pediatrics. 2014;133(3):375-385.
- Sun D, McCarthy TJ, Liberman DB. Cost-effectiveness of watchful waiting in acute otitis media. Pediatrics. 2017;139(4).
- Gerall CD, DeFazio JR, Kahan AM, et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. Available at: https://www.jpedsurg.org/article/S0022-3468(20)30756-9/pdf. Accessed December 8, 2021.
- Rabbone I, Schiaffini R, Cherubini V, et al. Has COVID-19 delayed the diagnosis and worsened the presentation of type 1 diabetes in children? Diabetes Care. 2020;43(11):2870-2872.
- Lynn RM, Avis JL, Lenton S, et al. Delayed access to care and late presentations in children during the COVID-19 pandemic: a snapshot survey of 4075 paediatricians in the UK and Ireland. Arch Dis Child. 2021;106(2):e8-e8.
- Santoli JM. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69.
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
- Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among us ambulatory care visits, 2010-2011. JAMA. 2016;315(17):1864-1873.
- Bourgeois T, Griffith C, Johnson E, et al. Barriers to current guidelines in the management of pediatric acute otitis media. J Pediatr Med. 2019;3(3). Available at: https://www.pediatricsresearchjournal.com/articles/barriers-to-current-guidelines-in-the-management-of-pediatric-acute-otitis-media.html. Accessed April 13, 2021.
- Brinker DL, MacGeorge EL, Hackman N. Diagnostic accuracy, prescription behavior, and watchful waiting efficacy for pediatric acute otitis media. Clin Pediatr (Phila). 2019;58(1):60-65.
- Büyükcam A, Kara A, Bedir T, et al. Pediatricians′ attitudes in management of acute otitis media and ear pain in Turkey. Int J Pediatr Otorhinolaryngol. 2018;107:14-20.
- Kemp C. Following watchful waiting guidelines for children with AOM cost-effective. AAP News. Available at: http://www.aappublications.org/news/2017/03/03/AOM030317. Accessed June 11, 2021.
- Broides A, Bereza O, Lavi-Givon N, et al. Parental acceptability of the watchful waiting approach in pediatric acute otitis media. World J Clin Pediatr. 2016;5(2):198-205.
- MacGeorge EL, Smith RA, Caldes EP, Hackman NM. Toward reduction in antibiotic use for pediatric otitis media: predicting parental compliance with “watchful waiting” advice. J Health Commun. 2017;22(11):867-875.
Author affiliations: Emily J. Montgomery, MD, Children’s Mercy Kansas City; University of Missouri-Kansas City. Brian R. Lee, PhD, MPH, Children’s Mercy Kansas City; University of Missouri-Kansas City. Amanda Montalbano, MD, MPH, Children’s Mercy Kansas City; University of Missouri-Kansas City. Amanda Nedved, MD, Children’s Mercy Kansas City; University of Missouri-Kansas City. The authors have no relevant financial relationships with any commercial interests.

