Urgent message: Urgent care operators must be mindful of costs and labor efficiency to navigate the challenges of rising and falling revenue in what’s been a highly seasonal business.
Alan A. Ayers, MBA, MAcc, is President of Experity Consulting and is Senior Editor of The Journal of Urgent Care Medicine.
For much of 2020 and 2021, the COVID-19 pandemic drove both uncertainty and higher volumes (and thus profits) to urgent care centers. With the 2022-2023 flu season behind us, it’s back to “business as usual” and operators are expressing an increased interest in improving efficiency and managing operating costs.
So, what do urgent care operators need to consider?
Reducing expenses and rethinking resource-hungry strategies adopted during the pandemic is essential in the coming months.
Volume-Driven Business
Urgent care has always been considered a volume-driven business because once there’s sufficient visits to cover a “skeletal” staffing model, each additional visit accrues to the bottom line.
In this sense, labor in an urgent care center is a fixed cost because without a provider, the center cannot serve patients. As with any fixed cost, profitability is increased as labor expense is spread across more patients.
Due to these basic economic factors, urgent care centers have always emphasized volume. In fact, one key performance indicator (KPI) that drives site selection, scheduling, and financials is patients per hour per provider.
Historically, urgent care has been a business that breaks even for 9 months of the year but then sees a windfall during flu season, when volume increases dramatically. This is why sustained COVID volume was so profitable for urgent care—COVID had added a second, year-round flu, in essence.
But what happens when this pattern isn’t followed? The last quarter of 2022 saw an abbreviated “quadremic” crisis of flu, COVID, strep, and RSV that ended abruptly compared to previous years. The impact was regionalized, with the greatest volume seen in states like Texas and Utah that have disproportionally large pediatric populations.
This is a reminder that flu season is not a guarantee. Many operators are still overstaffed from pandemic levels. With volumes levelling, finances will likely be tight this year, so finding ways to maximize efficiency—especially during the slower months—is essential to the survival of any urgent care business.
Managing Labor Costs
Labor, particularly provider labor, by far is the greatest expense of an urgent care center; generally, we assume it constitutes about 85% of operating costs. But without a skeletal staff of at least one provider and someone to support the front desk, an urgent care cannot operate. Creatively managing your workforce and finding new ways to maximize efficiency are powerful tools to increase your profitability.
Maximize Patients Per Hour Per Employee
In any business, revenue equals volume times rate. Since reimbursement rates are set by payers, assuming optimized coding and collections practices, this leaves operators with only one major lever to manipulate—volume. So, when managing your labor costs, your approach needs to be volume-driven and guided by data.
Focus on the KPI of patients per hour per employee. Improving this metric is key to increasing your volume while not overspending on additional staff.
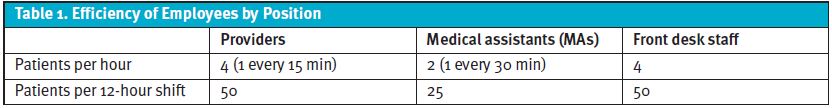
The efficiency of employees varies by position (see Table 1). While four patients per hour per provider (ie, one patient every 15 minutes) is a good rule of thumb, some operators would argue it’s “too slow” (ie, the number should be six) while other providers will argue it’s “too fast,” resulting in quality or safety issues (and that somewhere between two and three is a better number).
Attainable patient-per-hour efficiencies are affected by many factors, including patient demand in a trade area, patient acuity, scope of services offered, pacing vs ebb-and-flow of patient arrivals, use of standing orders, provider urgent care job experience and confidence, and the use of lean processes, support staff, automation, and technology.
Urgent care centers were so profitable during the pandemic because many providers were able to see eight to 10 patients per hour. However, this isn’t sustainable when demand is low, and your urgent care shouldn’t be using flu season extremes to guide year-round decisions.
Many operators get stuck in a mindset that the staffing model is set and consistent from site to site. This typically entails one receptionist, one medical assistant, and one provider…regardless of volume. Add that the front desk or medical assistant is also a radiologic technician and “fixed” labor costs per hour raise the bar on needed patient visits to break even.
These operators don’t think that a center seeing less than 20 patients per day can function with 1:1 staffing, meaning one provider and one cross-trained medical assistant/front desk person. When you have a rigid staffing model that disregards volume, your staff becomes idle and your center loses money each hour.
Because offering seasonal employment is highly impractical given credentialing and training requirements, what happens if a center schedules staff for “average” volume but then sees a sudden influx of patients? The answer is simple: Your staff works harder and patients wait.
That’s where technology that enables patients to “join the waitlist” and wait comfortably from home comes into play. Such queuing and registration systems pace arrivals to provider productivity, reducing stress and average wait and resulting in a better patient and provider experience. Wait times expand or contract based on provider productivity, and patients receive text message updates as their check-in time approaches.
An urgent care operator should continually focus on increasing the efficiency of existing staff by eliminating waste. “Waste” constitutes non-value-added activities that consume time. Shift administrative tasks like registration data entry to patients, utilize standing orders to test patients for flu, COVID or strep before the provider exam, and simplify provider documentation to enable your team to handle more patients per hour. By doing so, you’ll avoid the need to hire more people. Remember, adding additional staff drops the efficiency of your entire team.
Rethink Your Staffing Model
Aligning an urgent care center’s staffing model with patient demand plays a major role in managing labor-related costs. Maintaining a high “headcount” of full-time employees is expensive. To save money without sacrificing the quality care your center offers, a smarter approach is needed.
When there’s insufficient volume to justify a dedicated, full-time role, cross-training is one strategy. Nurse practitioners (NPs) and MAs can function as basic or limited-scope x-ray operators in many states. MAs can work the front desk in slower locations. To take this a step further, ensure each of your staff members practices at the top of their licensure and/or training. In urgent care, this means utilizing NPs or physician assistants over more costly MDs and DOs, or hiring an MA with a limited-license x-ray certificate instead of a fully licensed radiology tech.
Operators also need to take a serious look at benefits. Offering personal time off requires your center to have backup coverage when employees take it, in turn creating redundancy, excess capacity, and double the benefits costs. Instead, consider swapping or flipping the schedule for providers who work 3.5 days per week so they can have contiguous days off for travel or whatever they please.
For health benefits, limit coverage to spouses who don’t have benefits from their job. Consider offering a high-deductible health plan with discounts for healthy habits like preventative testing and tobacco abstinence.
Finally, realistically examine the staffing needs of your center. Your volume isn’t always at peak levels. So don’t stay locked into a rigid schedule. Instead, have a list of flexi- or traveling staff members or PRN providers ready. Then, when your regular staff becomes too busy, you can call in reinforcements.
Add Additional Services
What happens when the efficiency of your staff is maximized to patient demand, but you still have excess capacity? Adding additional services is one avenue for increasing profitable revenue in urgent care. Keep in mind, however, not all services result in profit. Though you may generate more revenue, if that revenue isn’t profitable, it doesn’t meet your goals.
Enhancing revenue from existing visits is low-hanging fruit. For example, assume the front desk is verifying coverage, entering data correctly, and collecting copays on every visit. Where deductibles apply, consider a credit-card preauthorization service. Ensure visits are being coded appropriately and optimize EMR usage to capture codes appropriately. Doing so generates more revenue from reimbursement without any additional cost. Increasing the clinically appropriate use of lab services and x-ray, such as for diagnostics, can also be effective. Finally, adding convenience services like medication dispensing can capture more revenue from each patient who visits your center.
Many operators fall into the trap of ignoring new opportunities. Don’t forget your patients need a wide range of healthcare services. Is your urgent care center able to add them?
Orthopedic specialty services are the number-one referral from urgent care centers. Rather than sending orthopedic patients to another local facility, consider bringing in an orthopedist one day a week with a management services organization arrangement. Doing so lets you keep the follow-up visit, and its revenue in your center.
When revenue from flu season-related services isn’t coming in, adding new services and optimizing existing processes can help buffer your bottom line.
Managing Operating Expenses
While generating more profitable revenue is never a bad thing, urgent care operators also need to take a hard look at cutting their expenses as we move into 2023. The COVID pandemic and its related effects led many centers to increase spending. Some of this spending is inflation driven—particularly of wages and supply costs—but others are surplus. Now, even with revenues slowing down, those centers may have not scaled back their spending accordingly.
Reducing operating expenses is essential for centers struggling to weather the “drought” months outside of flu season. In practice, this can take many forms.
Supply Inventory Management
Saving on non-labor operating costs begins with managing your supply inventory and acquisition. Centers may use the same supplier for years without researching offers from competitors. To ensure your center is getting the best price, always solicit bids from several suppliers (Medline, McKesson, Henry Schein, et al).
Moreover, be mindful of your ordering habits. Order less frequently to take advantage of the lower shipping costs of larger orders.
Does your center have an abundance of supplies sitting unused in the cabinetry of patient rooms? If so, have you noticed the staff doesn’t get the supplies they need from those cabinets, but rather, the central supply closet?
Sitting inventory is money you’re wasting when you could use the capital to help cover operating expenses. In fact, one recommendation is to just eliminate cabinetry that’s a magnet for unused supplies Next, aim to reduce formulary SKUs to the essentials, eliminating duplicate items that serve the same purpose, and switching from branded to generic or private-label products.
Focusing again on the issue of volume, reduce your inventory levels and order frequency to match the demand your center sees. Without massive surges of COVID (and especially outside of flu season), you don’t need to hoard supplies.
It’s time to re-examine how much supply inventory your center goes through over time and pace your orders accordingly.
Lowering Occupancy Expenses
The amount paid for your space is unavoidable in that it’s typically locked in by your lease. However, you can save money by taking a few steps. First, consider renegotiating your lease renewals at the updated market rate. Real estate prices are changing all the time. If your initial lease contained TI (tenant improvement) that’s been fully amortized, or if “escalators” resulted in annual rent increases in excess of actual market rent, then you should try to negotiate a renewal lease reduction. Do your research and don’t pay more than you should.
Many landlords are also unfamiliar with the ebb-and-flow nature of urgent care volumes. With this in mind, operators may want to ask for flexibility in rent payments during slow periods to ease some pressure.
Occupancy expenses don’t just cover rent. Operators should also consider the third-party services they spend money on. For example, does every center need daily professional cleaning? Or could a center with less traffic assign MAs to clean during the day and bring in professional cleaners once a week?
The same is true when considering services like printer and copier maintenance, window washing, document shredding, and bottled water delivery to name a few. Often, a cheaper alternative is available. Try cutting down the number of printers/copiers at your center, handling documents electronically rather than printing and faxing, having staff clean the windows, purchasing shredding machines, or installing water filters for staff to refill their bottles. This might not be glamorous, but for many centers, it’s low-hanging fruit.
Conclusion
In today’s world of tight margins and fluctuating revenue, tightening your belt is simply part of running a successful urgent care. Cut out unneeded spending where possible and focus on funneling your dollars back into your center in ways that improve your services and create growth opportunities.
Focusing (or refocusing) on the basics will allow your center to thrive in the face of economic uncertainty as our industry continues adapting to the post-COVID world.
Read More
- Smoothing Ebb-And-Flow For Greater Staff Efficiency And Shorter Wait Times In Urgent Care
- Using Key Performance Indicators To Measure, Track, And Improve Performance In Urgent Care
- Open For Debate: Minimum Operating Hours For Urgent Care

