Urgent message: Do not be fooled by the diagnosis made by clinicians before you. Many seemingly benign symptoms can be harbingers of more serious pathology.
JESSICA HOFFMANN, MS-4, and JOHN SHUFELDT, MD, JD, MBA, FACEP
Chronic back pain is a common presentation in both the urgent care and emergency department (ED) settings. Care-on-demand providers often find themselves deciding how extensive a workup to do for a patient with acute-on-chronic back pain.
After a patient has had 4 to 6 weeks of conservative treatment (i.e., nonsteroidal anti-inflammatory drugs, muscle relaxants, patient education, and physical therapy) without a decrease in pain, imaging should be performed.1 Conventional imaging for lower-back pain includes plain films, and if findings for plain films are nondiagnostic, then computed tomography (CT) or magnetic resonance imaging (MRI) should be performed. In addition, laboratory workups to assess for the presence of inflammation, such as erythrocyte sedimentation rate, C-reactive protein, and complete blood count with differential, may be performed to rule out infectious sources of low-back pain.
This approach, however, should not exclude evaluation of risk and red flags for more serious or threatening causes. Vascular, gastrointestinal, oncologic, and infectious etiologies are often overlooked without careful evaluation. Obtaining a detailed medical history and conducting a thorough physical examination are paramount for avoiding the “big miss” in the urgent care setting, as is an understanding of the red flags that may identify a more serious and even life-threatening etiology.
Case Presentation
RC, a 37-year-old man with obesity, was sent from the urgent care center to the ED after reporting 3 days of severe-on-chronic, constant dull back pain. The patient had a long history of chronic back pain with multiple prior visits to urgent care centers and EDs. His chart at the urgent care center flagged him as a “frequent flyer” who might be seeking narcotics.
In addition, the patient’s primary-care physician and an orthopedic spine specialist had previously evaluated him for similar problems, which the patient stated were long-standing. Prior workups included lumbosacral radiographs, CT of the thoracic and lumbar spine, and MRI, which revealed mild degenerative disc disease.
Earlier disease management had included physical and occupational therapy, and a referral to a pain- management program. The patient was sent from an urgent care center to the ED because he reported flank and low back pain, worse on the right side. Despite the flag on the patient’s chart, the urgent care provider was concerned about ureterolithiasis and sent RC to the ED for further evaluation.
On ED presentation, RC also reported intermittent bilateral lower- extremity numbness and pain that was progressively worsening and became worse with exertion. On further questioning, the patient also reported difficulty developing an erection.
Medical and family histories revealed that RC was a current smoker with a medical history of hypertension without prior treatment and with significant family history of heart disease. The patient’s parents both died of cardiac causes while in their fifties, his half-sister died of heart disease, and his half-brother had a myocardial infarction at an early age.
Observations and Findings
Evaluation of the patient showed the following:
T: 36.8°C
RR: 18
P: 117
BP: 176/124
Physical examination revealed an obese, alert male in mild distress secondary to back pain. Findings on his cardiovascular examination were significant for tachy-cardia and diminished pulses in the bilateral lower extremities. His skin was warm to the touch; however, it had a dusky appearance while the patient was in a dependent position. The patient had bilateral flank tenderness to palpation. There were no other abnormal findings. Findings on the distal neurologic examination were unremarkable. The patient had a strength rating of 5+ (on a scale of 0 to 5) for his lower extremities on flexion and extension. He had good rectal tone and reported no saddle anesthesia. His bilateral deep tendon reflexes were rated 3+ (on a scale of 0 to 5).
Diagnostic Studies
Initially, a noncontrast CT scan of the abdomen and pelvis was ordered to rule out the presence of an obstructing stone. This revealed a 3-mm nonobstructing renal calculi of the left kidney as well as para-aortic stranding with small areas of calcification in the lumen of the aorta, which could represent aortic dissection or aortitis. Follow-up with a contrast-enhanced CT angiogram was recommended.
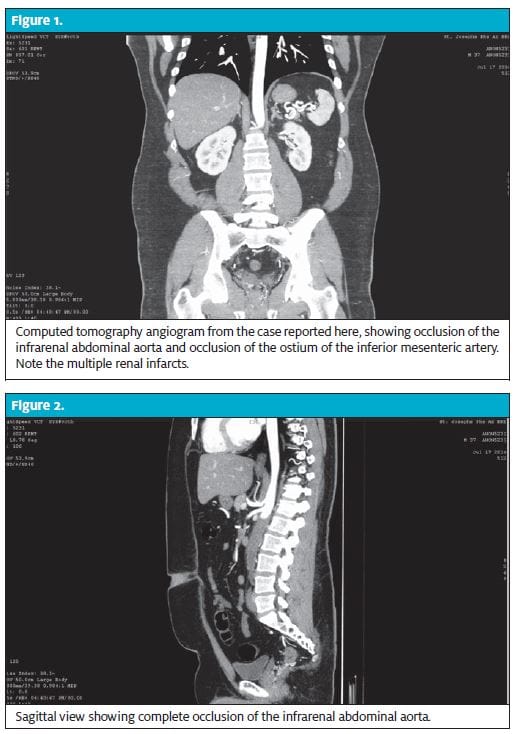
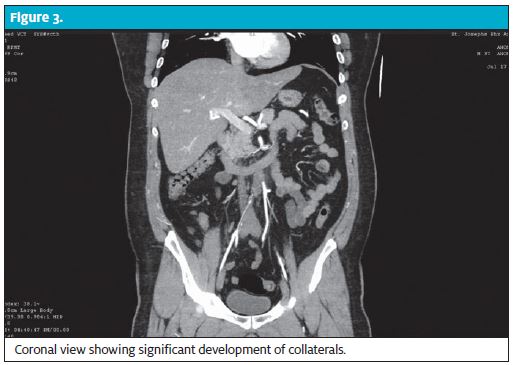
The angiogram revealed complete occlusion of the infrarenal abdominal aorta, extending into the common iliac arteries, with reconstitution of flow at the level of the bifurcation of the internal and external iliac arteries. Also present were occlusion of the ostium of the inferior mesenteric artery, reconstitution of flow distally, diffuse periaortic stranding, and multifocal left renal infarcts (Figures 1, 2, and 3).
Diagnosis
Leriche syndrome (aortoiliac occlusion).
Course and Treatment
The combination of findings on
RC’s medical history, physical examination, and CT angiogram revealed severe vascular disease consistent with Leriche syndrome. A vascular surgeon was consulted. The patient’s blood pressure was controlled, and he underwent preoperative evaluation, including a pharmacologic stress scan using regadenoson (Lexiscan) for evaluation of his coronary arteries. On the third hospital day, he underwent aortobifemoral bypass surgery.
Discussion
Leriche syndrome, or aortoiliac occlusive disease, typically affects men in their fourth to fifth decade of life.2 It is classically characterized by a triad of claudication, decreased femoral pulses, and impotence.3 This constellation of symptoms is secondary to atherosclerotic obstruction of peripheral vessels.4 Occlusion generally begins at the distal abdominal aorta and progresses both proximally and distally. Occlusion of the abdominal aorta at the bifurcation of the iliacs in Leriche syndrome typically develops slowly, which allows time for collateral vessel development and minimization of the risk of life-threatening ischemia. Risk factors for Leriche syndrome include cigarette smoking, hypertension, and hyperlipidemia.5
Several prior cases of Leriche syndrome presenting atypically have been described, including paraplegia,6 sciatic neuropathy,7 and treatment-resistant hypertension due to extension of occlusion to the bilateral renal arteries.8 In the case described here, Leriche syndrome was disguised by a long history of chronic back pain and untreated hypertension. To our knowledge, this is the first case of Leriche syndrome presenting as worsening chronic back pain. In this case, the chronic and worsening nature of back pain likely correlated with the onset and degree of occlusion of the aorta.
The standard low back pain workup algorithm generally does not include specific vascular etiologies.1 As in the case of RC, a generally healthy 37-year-old man without obvious warning signs is presumed to have musculoskeletal back pain until there is a failure to improve with conservative treatment. According to traditional algorithms, RC received proper management of his lower-back pain before he presented to the urgent care center. The finding of mild degenerative disc disease on MRI likely led clinicians astray during previous assessments and contributed to the early missed diagnosis. The combination of hypertension, obesity, smoking history, and strong family history of cardiac disease placed RC at high risk for vascular pathology. If the numerous physicians who cared for RC prior to his ED visit had maintained broad differentials and performed thorough vascular examinations, RC might have received an accurate diagnosis and therefore more appropriate care much earlier in the course of his chronic back pain.
This case highlights the importance of obtaining a thorough medical history and performing a detailed physical examination even in patients with commonly benign chief symptoms. In addition, the case illustrates the value of maintaining broad differentials and ruling out serious pathology before attributing chronic back pain to musculoskeletal causes.
Take-Home Points
It is easy and convenient to work off the same diagnosis that health-care providers before you made. Patients with back pain are often ticking time bombs: Their back pain may be a symptom of significant disease such as epidural abscess, epidural hematoma, cauda equine secondary to canal stenosis, or aortic aneurysm. A high degree of vigilance is necessary to make the proper diagnosis in cases like this one.
References
- Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85:343–350.
- Diehm C, Schuster A, Allenberg JR, et al. High prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: cross-sectional study. Atherosclerosis. 2004;172:95–105.
- Leriche R, Morel A. The syndrome of thrombotic obliteration of the aortic bifurcation. Ann Surg. 1943;127:193–206.
- Wooten C, Hayat M, du Plessis M, et al. Anatomical significance in aortoiliac occlusive disease. Clin Anat. 2014;27:1264–1274.
- Frederick M, Newman J, Kohlwes J. Leriche syndrome. J Gen Intern Med. 2010;25:1102–1104.
- Akhaddar A, Eljebbouri B, Saouab R, et al. Acute paraplegia revealing Leriche syndrome. Intern Med. 2012;51:981–982.
- Yoon do H, Cho H, Seol SJ, et al. Right calf claudication revealing Leriche syndrome presenting as right sciatic neuropathy. Ann Rehabil Med. 2014;38:132–137.
- Yilmaz M, Kaptanogullari OH, Caliskan C, et al. Inevitable hemodialysis for treating resistant hypertension in a patient with Leriche syndrome. Clinics (Sao Paulo). 2012;67:1483– 1486.