Published on
Urgent message: Influenza types A and B have demonstrated a pattern that increases patient volumes in urgent care centers during “flu season.” But the COVID-19 virus, including its different variants, continues to have different patterns throughout multiple waves and has shown to overcome/oppress other predictable viruses.
Cesar Mora Jaramillo, MD, FAAFP, FCUCM
Citation: Jaramillo CM. SARS-CoV-2 and influenza type A/B Infection rates: a report of a federal qualified health care center-urgent care department during Omicron wave in Rhode Island. J Urgent Care Med. 2022;16(11):29-33.
INTRODUCTION
The relatively recently detected SARS-CoV-2 B.1.1. Omicron COVID-19 variant is known as highly infectious/transmissible due to its more than 30 mutations on the spike protein (the part the virus uses to attach to human cells) but less virulent than previous variants.1,2 Omicron is considered the fifth COVID-19 variant of concern. By late December of 2021 it was announced as the predominant variant in the United States. Just weeks later, nearly 100% of new COVID-19 infections were attributed to Omicron.2
Influenza Type A and B viruses cause seasonal infections, most commonly during the fall and winter. Prepandemic, the WHO reported an estimated 1 billion cases every year across the globe, of which 3 to 5 million are severe cases, resulting in 290,000 to 650,000 influenza-related respiratory deaths.3
DESCRIPTION
The Express Department of a federal qualified health center (Providence Community Health Centers) has been considered a “hot zone” since the pandemic started. As part of the U.S. Outpatient influenza-like Illness Surveillance Network (ILINet), the department provided nasal swabs for SARS-CoV-2 RT-PCR assay to the Rhode Island Department of Health regardless of rapid tests results, to assess ILI illness rates in our community and to detect COVID-19 infections and variants. Rapid tests were obtained using Sofia 2 Flu + SARS Antigen FIA machine.
Historically, the Express Department managed close to 25,000 visits a year (pre-COVID-19 pandemic). The Community Health Center serves a predominantly Hispanic/Latino population, including many uninsured patients, undocumented immigrants, and households under 200% of the federal poverty level.
METHODOLOGY
Retrospective Descriptive Study
Data were retrospectively obtained from the urgent care department of a Federally Qualified Health Center (FQHC) in Providence, RI, to determine the percentage of SARS-CoV-2 and influenza type A and B infections during the four-wave attributed to the Omicron variant. A query of the electronic medical record database of the point-of-care (POC) rapid SARS-CoV-2 and influenza A/B testing. In addition to the report from the Rhode Island Department of Health (RIDOH) on RT-PCRs swabs, results were identified from November 2021 to January of 2022 (12 weeks). In the Express Department, a total of 3,655 patients with influenza-like Illness (ILI) symptoms were tested during this period.
The data were analyzed to assess the percentage of confirmed infections with RT-PCR and compare with rapid testing POC to study the rate of false-negatives and false-positives results. Providence Community Health Centers approved the project.
RESULTS
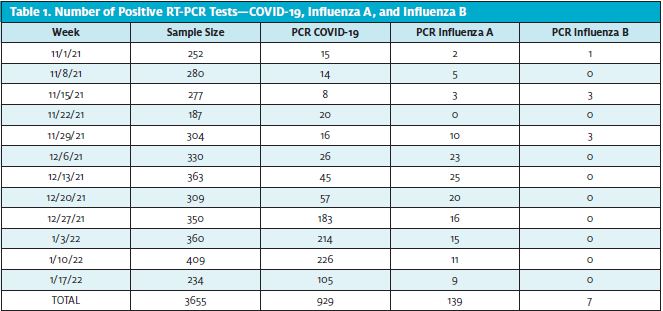
A total of 3,665 patients with ILI symptoms were tested from November 2021 until January 17, 2022. Of these patients, 929 had a positive PCR test for SARs-CoV-2 infection, while 139 tested positive for influenza A and seven for influenza B (see Table 1).
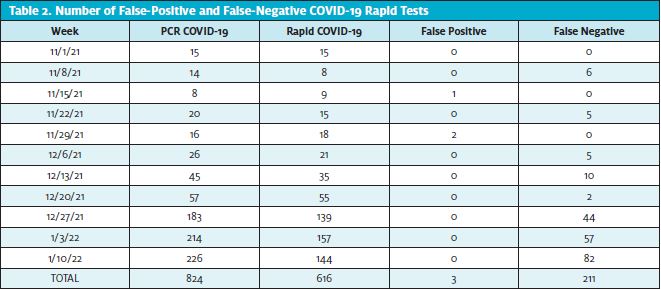
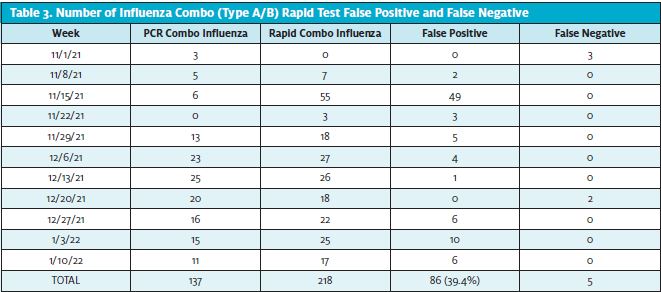
A total of 616 rapid COVID tests and 218 rapid influenza combo tests were obtained from the first week of November 2021 to the third week of January 2022. Regarding COVID-19, 211 rapid false-negative tests (34%) were obtained, with only three (0.48%) being false-positives (Table 2). Furthermore, a total of 86 false-positive (39.4%) and five false negatives rapid influenza tests were obtained (Table 3).
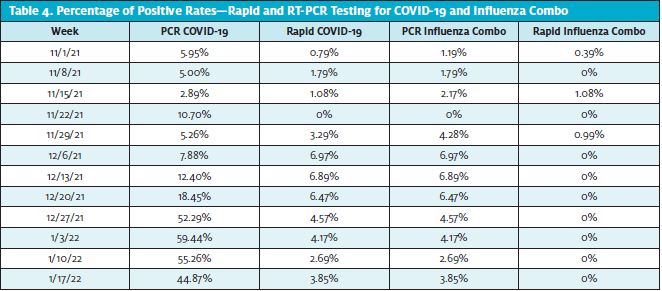
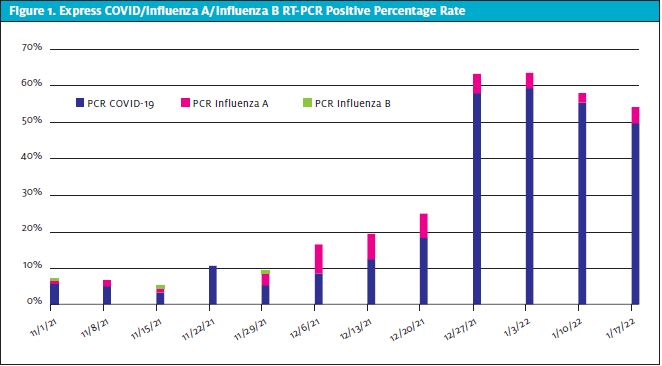
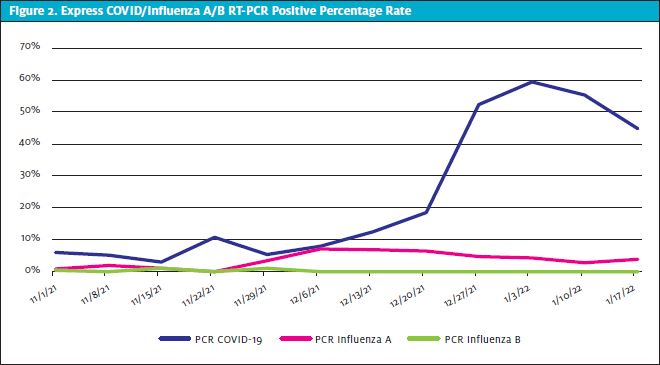
The lowest positive rate of COVID-19 infections was 2.89% during the third week of November, and the highest was 59.44% during the first week of January (Table 4, Figure 1, and Figure 2). Regarding influenza type B, a total of seven positive PCRs were reported, and all the cases were in the month of November, while influenza A highest rates were during the first 2 weeks of December.
DISCUSSION
As SARS-CoV-2 infections spiked nationwide during late fall/early winter of 2021-2022, most cases were attributed to the Omicron variant. On December 11, 2021, RIDOH announced the first case of COVID-19 Omicron variant, 10 days after the first case was reported in the United States.4
One week after the first case of Omicron in Rhode Island, the Express Department experienced a 6% increase in the rate of COVID-19 infections and a 39.89% increase within 3 weeks (2.5 out of five patients had a positive PCR test by the last week of December 2021).
By December 19, the state averaged about 1,068 new COVID-19 cases a day.5 With the rates of SARS-CoV-2 infections increasing in a very short time, the governor of Rhode Island mandated that residents wear masks indoors of large businesses on December 20, 2021. Moreover, at this time, nearly 85% of residents have received at least one shot of a coronavirus vaccine; 74% were fully vaccinated.5
Mask mandates were implemented when the department’s COVID-19 infections were at a 18.45% positive rate. The peak of SARS-CoV-2 infections during the first week of January 2022 (when 5.9 out of 10 patients tested RT-PCR positive) was noticeable 2 weeks after the mask mandate was announced. Consequently, the effect of masks was synergized with the high vaccination rates in the state, showing a decrease in cases 1 week after the peak to a rate of 55.26% (from 59.4%).
During the 12 weeks of analyzed data, almost a quarter (22%) of rapid COVID-19 tests were false-negatives, and only three were false-positives (0.48%). In contrast, 3.9 out of 10 patients had a rapid influenza combo false-positive test. These data show that the risk of COVID-19 false-positive results is low during high prevalence of infections but rather a higher risk for false negatives.6
Sofia 2 Flu + SARS antigen FIA product has a sensitivity for nasal swabs for influenza A of 90%, influenza B of 89%, SARS-CoV-2 of 95.2%, and a specificity of 95%, 96%, and 100%, respectively.7 In this study, the 22% rate of rapid COVID-19 false-negatives and the 39% of influenza false-positive combo contradict the product’s sensitivity and specificity, respectively. With that said, testing should assist clinicians in making medical decisions, but clinical information should also be a vital component. Moreover, testing should be used carefully, with clinicians considering the limitations and the impact of these while evaluating patients. Hence, it is crucial for quality of care to balance test results’ desirable and undesirable significance when deciding which tests should be performed and whether their results will influence medical decisions.8
These data reveal how little we know about viruses, as well as a good deal of uncertain and raising new questions: Will COVID-19 become a seasonal virus? Is another wave coming soon? Are more variants expected this year? Will influenza cases continue to be minimal compared to COVID-19 infections during fall/winter?
CONCLUSION
Urgent care centers continue to play an essential role in healthcare, especially since the SARS-CoV-2 was declared a pandemic. Historically, urgent care’s patient volumes have been highly driven by infections, mostly seasonally, leading clinicians to diagnose and treat accordingly. Medical decision-making should be complemented with testing in certain conditions/situations. When interpreting results, clinicians should understand the limitations of testing and the impact of community infection prevalence in false-positive and false-negative results. Hence, intertwining a detailed clinical history and interview, performing a focused physical exam, obtaining relevant diagnostic testing, and referring or consulting with other clinicians are important tools for gathering information in the process of appropriately diagnosing and treating patients. Furthermore, the clinical decision making must be tailored to the specific patient’s needs and situation. A timely accurate diagnosis decreases the risk of poor health outcomes.
These data accentuate how limited our knowledge is regarding virus behaviors and highlights the concern of how unpredictable they can be. There is still a lot of uncertainty, but urgent care centers will continue to adapt and adjust as they had in the past. Such uncertainty will require continued vigilance toward emerging data at the local, state, and national levels.
References
- Fauci KL. Omicron ‘very different from other variants.’ Medscape. Available at: https://www.medscape.com/viewarticle/963867?ecd=ppc_google_rlsa-traf_mscp_news-perspectives_t1_us. Published December 2, 2021. Accessed January 30, 2022.
- Iuliano AD, Brunkard JM, Boehmer TK, et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods – United States, December 2020 – January 2022. MMWR Morb Mortal Wkly Rep. 2022;71:146-152.
- WHO launches new global influenza strategy. World Health Organization. Available at: https://www.who.int/news/item/11-03-2019-who-launches-new-global-influenza-strategy. Published March 11, 2019. Accessed January 30, 2022.
- Omicron variant identified in Rhode Island. Governor’s Office, State of Rhode Island. Available at: https://governor.ri.gov/press-releases/omicron-variant-identified-rhode-island. Published December 11, 2021. Accessed January 30, 2022.
- Rhode Island partially reinstating indoor mask mandate. US News & World Report. Available at: https://www.usnews.com/news/best-states/rhode-island/articles/2021-12-19/rhode-island-partially-reinstating-indoor-mask-mandate. Published December 19, 2021. Accessed February 13, 2022.
- Healy B, Khan A, Metezai H, et al. The impact of false positive COVID-19 results in an area of low prevalence. Clin Med (Lond). 2021;21(1):e54-e56.
- Food and Drug Administration. Sofia2 Flu+SARS Antigan FIA. Intended use. Available at: https://www.fda.gov/media/142704/download. Accessed February 13, 2022.
- Buehler AM, Ascef BO, Oliveira Júnior HA, et al. Rational use of diagnostic tests for clinical decision making. Rev Assoc Med Bras (1992). 2019 Mar;65(3):452-459.
- Flu causes: types of influenza viruses, contagious transmission, and more. WebMD. Available at: https://www.webmd.com/cold-and-flu/what-causes-flu-viruses. Accessed January 30, 2022.
- Tumolo G. Legal alerts. Rhode Island reimposes indoor mask mandate as COVID-19 cases rise sharply. Lewis Brisbois Bisgaard & Smith LLP. Available at: https://lewisbrisbois.com/newsroom/legal-alerts/rhode-island-reimposes-indoor-mask-mandate-as-covid-19-cases-rise-sharply. Accessed February 13, 2022.
- Polaris JJ, Katz JN. ‘Appropriate’ diagnostic testing: supporting diagnostics with evidence-based medicine and shared decision making. BMC Res Notes. 2014;7:922. Published 2014 Dec 16.
