Urgent message: Parallel lacerations or those that simply occur in close proximity pose a unique challenge for the urgent care clinician. Repairing either wound without inflicting further trauma on the other(s) requires both skill and familiarity with performing the appropriate technique.
Patrick O’Malley, MD
The Problem
Lacerations in close proximity pose a unique challenge for the urgent care clinician. This situation is often encountered in the unfortunate setting of patients engaged in “cutting” behaviors. Narrow spans of tissue (tissue bridges) between lacerations have a limited blood supply. During repair, these bridges can sustain further injury from both repeated violation by the suture needle and from the tension of the suture.
The Solution
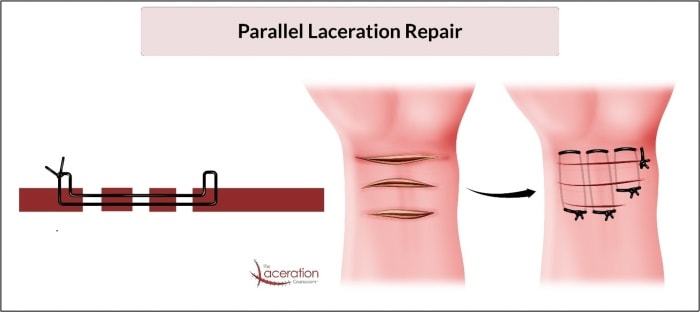
A simple technique commonly referred to as an “extended” or “modified” horizontal mattress can allow for success with approximation in this situation. With this technique, the clinician utilizes tissue forceps to grasp, manipulate, and stabilize the tissue. The initial entry into the tissue is then followed by passing the needle and thread through the dermal layer of adjacent tissue bridges until all lacerations have been crossed. As with any horizontal mattress technique, the needle and thread are oriented back in the opposite direction, passing through the same tissue planes.
The tension in the thread can then be adjusted and the tissue can be manipulated into approximation. Lastly, the suture is tied off in standard fashion, bringing the tissue edges into close proximity. (See Figure 1.)
Other Applications
This technique can prove useful in a variety of situations beyond parallel lacerations. If tissue is macerated (or even avulsed) and in close proximity to another laceration, this technique can be used to help approximate the various wound margins.
Figure 2a depicts a patient with a tractor-related foot injury and is an example where this technique would prove particularly useful. The proximal aspect of the wound had some macerated tissue with lacerations in close proximity, where the tissue would not support individual sutures. Employing this technique allows for the tissue to be approximated while avoiding further trauma from the suture needle. Figure 2b reveals appropriate wound healing (although with some hyperpigmentation).


The technique described above is demonstrated here.
Additional Reading
Mitchell GC. Repair of parallel lacerations. Ann Emerg Med. 1987;16(8):924.
Patrick O’Malley, MD is an emergency physician at Newberry County Memorial Hospital, Newberry, SC, and the creator/owner of The Laceration Course lecture series.

